Orbital Venous Malformation
Images


CASE SUMMARY
A 4-year-old presenting with painless, right exophthalmos.
IMAGE FINDINGS
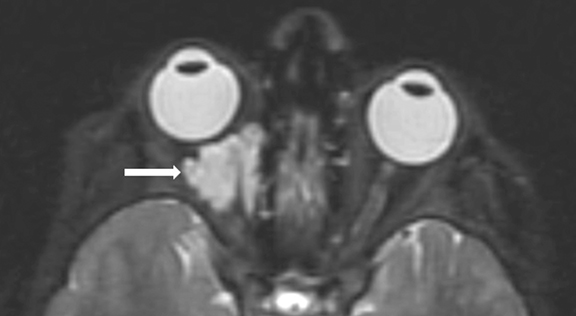
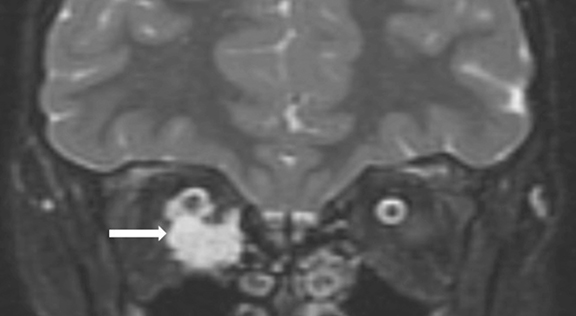
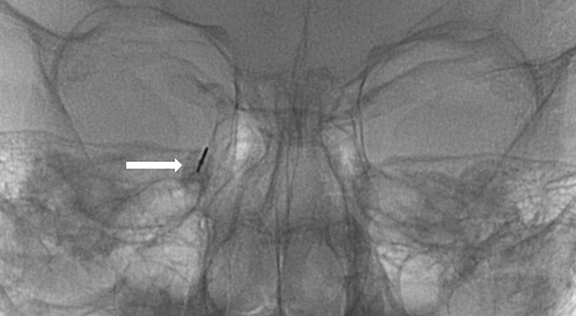
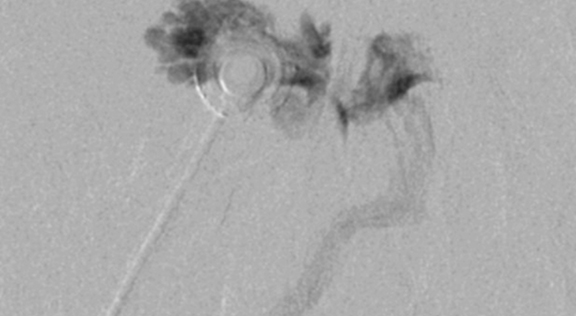
An orbital MRI was performed to evaluate the cause of the exopthalmus (Figure 1). Axial and coronal images revealed a lobulated, non-calcified, intraconal, orbital soft-tissue mass pushing the right globe anteriorly approximately 4 mm. The lobulated nature of the lesion suggested the diagnosis of an intraorbital venous malformation. At the time of sclerotherapy, a needle was guided into the venous malformation using ultrasound (US) guidance (Figure 2). Blood return was noted and an orbital venogram confirmed a venous malformation. A total of 2 mL of Bleomycin (15U/mL) was injected. A second procedure was subsequently performed about 4 months later. Clinical examination showed reduced proptosis. The child tolerated both procedures without complications.
DIAGNOSIS
Intraconal venous malformation of the right orbit
DISCUSSION
The differential diagnosis of proptosis is long; however, the conditions presenting as an intraorbital mass in children is focused on vascular malformations, neoplasms, and infection. The most common vascular lesions are venous malformations, lymphatic malformation, and hemangiomas. Initial evaluation with MR is preferred; however, US helps to distinguish between a congenital vascular lesion and neoplasm, and to guide biopsy or sclerotherapy. Also, US best shows the internal architecture of the lesion and identifies the vascular channels and compressibility of the lesion. This is important, since vascular malformations usually are compressible while neoplasms are not. The most common primary tumor of the head and neck is a rhabdomyosarcoma that can mimic a congenital vascular lesion. Other neoplasms that can be seen in this anatomic locale include neuroblastoma, juvenile fibrosarcoma, granulocytic sarcoma, and metastases. These lesions are often associated with bone destruction, and are solid and non-compressible on ultrasound examination. Lastly, infections are common in the orbital and periorbital regions but are rarely confused with a vascular lesion due to the associated clinical features.
Venous malformations (VMs) are the most common type of congenital vascular malformations and can affect any tissue or organ. Most lesions are isolated and only 1% of cases are multifocal. In a minority of patients, a mutation in the TIE-2 gene has been identified, linking 1.2% of VMs to genetic causes.1,2 Venous malformations involving the face may distend with Valsalva maneuver or positioning the child in a head-down dependent position and can cause deformity, asymmetry, exopthalmus and dental problems. About 40% of slow-flow vascular lesions can be found in the head or neck region, but are also found in the extremities (40%) and trunk (20%). VMs may cause pain, especially when local thrombosis occurs within the VM as a precursor to phlebolith formation. These local clots rarely result in distant embolization. When VMs are superficial they may have a bluish hue.1,3
VMs are the result of a smooth muscle cell deficiency during fetal vein development. This causes improperly functioning, malformed veins resulting in venous malformations. Although these lesions can be present at birth or appear later in life, they generally grow with the patient. However, pain and malformation growth can occur during hormonally active times such as growth spurts, puberty and pregnancy.
Orbital VMs can be located in the periorbital or orbital regions. A VM in the orbit can be intraconal or extraconal (pre- or postseptal). Easily accessible VMs can be treated surgically if complete resection is possible. If complete resection is not likely, sclerotherapy, if possible, should be considered the treatment of choice alone or as an adjunct to surgery. Likewise, sclerotherapy can also be used to reduce residual VM after surgery. Ethanol is the most commonly used agent in sclerotherapy due to its high efficacy, low cost, and high curative potential. Upon injection, ethanol displaces water molecules and penetrates the lipid bilayer of the cells, which compromises the stable membrane and kills the endothelial cells.3,4
Potential complications with ethanol sclerotherapy include nerve injury with sensory loss and blindness in or around the treated eye, cavernous sinus thrombosis, skin necrosis, renal failure, and cardiopulmonary failure. Although it has the highest complication rate, ethanol also has the highest rate of success compared to other agents.4 Other common sclerosing agents include sodium tetradecyl sulfate (STS), Bleomycin, and polidocanol.
Bleomycin is playing an increasingly important role in treating VMs. Bleomycin, a chemotherapeutic agent, differs from the traditional sclerosants in that it has a longer time to action and it causes fibrosis. Also, it is important to know that there is a recommended total lifetime dose of 300 mgs, since pulmonary fibrosis may occur when this dose is exceeded. Currently, it is unknown whether pulmonary fibrosis will occur when Bleomycin is used for sclerotherapy. Considering baseline pulmonary function tests is worthwhile when this drug is used. The key difference between Bleomycin and ethanol is that Bleomycin can be effective when injected within or around a VM. Also, Bleomycin injection does not cause significant post-injection swelling. This is important when treating lesions that may affect the airway eg, a palatal VM or a lesion in a confined space, such as the orbit. For these reasons Bleomycin was used for this child’s intraconal lesion.
CONCLUSION
The location of orbital VMs presents multiple treatment challenges. MRI plays an important role in the initial diagnosis of VMs due to the modality’s large field of view and multiple sequences. Contrast enhancement is helpful in separating components of the differential diagnosis, while US is helpful at determining the internal architecture of the lesion and guiding needle placement for biopsy or sclerotherapy. Ethanol is an effective sclerosant in the treatment of orbital VMs. When ethanol is utilized, the patient is generally admitted for observation due to the risk of swelling that can put the eye at risk from excessive proptosis. In our practice, Bleomycin is preferred over ethanol for the treatment of intraconal VMs because it causes minimal postprocedural swelling. Patients treated with Bleomycin are briefly observed then discharged if proptosis is stable and does not threaten the health of the orbital contents.
REFERENCES
- Venous Malformations. Retrieved from https://www.cincinnatichildrens.org/health/v/venous.
- Benoiton LA, Chan K, Steiner F, FitzJohn T, and Tan ST. Management of Orbital and Periorbital Venous Malformation. 2017. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447072/
- Behravesh S, Yakes W, Gupta N, Naidu S, Chong B. et al. Venous malformations: Clinical diagnosis and treatment. 2016. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5220204/
- Mulligan PR, Prajapati HJ, Martin LG, and Patel TH. Vascular anomalies: Classification, imaging characteristics and implications for interventional radiology treatment approaches. 2014. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4064609/
Citation
A K, R T, C S, R K, S J, T A, A T, D A.Orbital Venous Malformation. Appl Radiol. 2020; (2):48D-48F.
March 17, 2020