Optic Disc Drusen
Images

CASE SUMMARY
An overweight 25-year-old with an eight-year history of chronic headaches presented to the emergency department with an acute headache, 10/10 in severity and exacerbated by activity. They described their headaches as bifrontal, recently increasing severity and frequency. The patient also endorsed blurry vision, photophobia, and phonophobia. Their symptoms were alleviated by lying flat in a quiet, dark room.
Unilateral right-sided papilledema was seen on fundoscopic exam. Pseudotumor cerebri (idiopathic increased intracranial pressure) was the working diagnosis based on clinical and ophthalmologic examination. Brain MRI, CT venogram, and lumbar puncture with opening and closing pressures were recommended. Lumbar puncture demonstrated colorless spinal fluid and an opening pressure of 10 mmHg (normal opening pressure 8-15 mmHg). Laboratory analysis of CSF and peripheral blood was unremarkable.
IMAGING FINDINGS
Brain and orbital MRI demonstrated no findings typically associated with idiopathic increased intracranial pressure. There was no evidence of an empty sella, tortuous optic nerves, optic hydrops (increased CSF signal around the neve), flattening of the posterior sclera, optic nerve enhancement, or optic nerve head protrusion.1
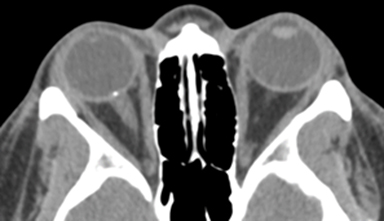
Subsequently, head CT and CT venogram were obtained to evaluate for dural venous sinus thrombosis or intracranial venous stenosis as a cause of the symptoms. The CT venogram demonstrated no dural venous sinus abnormality; however, a punctate calcification was observed at the right optic nerve head junction (Figure 1).
DIAGNOSIS
Optic disc drusen
DISCUSSION
Optic disc drusen (ODD) may present a diagnostic dilemma for the clinician, as it may mimic papilledema on fundoscopic exam and result in an invasive work-up for increased intracranial pressure or optic neuropathy. In patients presenting with a new onset headache, CT of the head remains the most commonly performed exam.
The condition is often apparent on head or orbital CT as a small focus of calcification located at the optic nerve head. However, as a relatively rare finding, ODD may be overlooked on CT scans with minimal or no calcification, scans with insufficient resolution, or scans performed with 5 mm or greater slice thickness.2
MRI is of little diagnostic value in ODD, owing to the limited ability to detect small calcifications on routine sequences; however, pre- and postcontrast brain and orbital MRI remains the most sensitive modality for excluding intracranial and intraorbital pathology that may cause elevated intracranial pressure.3 Susceptibility weighted imaging may add sensitivity for ODD.
A benign calcification at the optic nerve head junction, ODD affects 0.25%-2.0% of the population and is more prevalent in White people.4 The condition is a result of acellular calcific deposition within the optic nerve that may mimic papilledema on fundoscopic exam, thus representing a diagnostic challenge for clinicians.5 It is usually asymptomatic, although some patients may present with headaches, blurry vision, or vision loss. Fundoscopic examination may detect yellow drusen deposits on the surface of the optic nerve, but in cases of deep deposition within the optic nerve, ODD can manifest as pseudopapilledema.6
Accurate diagnosis is crucial, as patients require continuous monitoring for possible complications that include hemorrhage and blindness.7 Ocular sequelae include retinal vascular abnormalities, such as anterior ischemic optic neuropathy, the most common cause of vision loss in patients with ODD.8 Intracellular mitochondrial calcification owing to abnormal axonal metabolism with subsequent deposition of hyaline material in the optic nerve is considered one of the mechanisms leading to ODD formation. Genetic predisposition resulting from inherited dysplasia has been suggested as a predisposing factor.9
Several diagnostic approaches can be pursued with respect to ODD, including fundoscopy, B-scan ultrasonography, and CT. Fluorescein angiography may be useful in diagnosing deeply buried drusen and may demonstrate a fluorescence spot during the late stages of angiogram.7 B-scan sonography can evaluate the entire optic disc and is sensitive to calcium deposits buried deeply in the optic tissue, making it the diagnostic modality of choice.6 Optical coherence tomography may offer enhanced sensitivity for detection of buried drusen deposits.2, 10
CONCLUSION
Optic disc drusen may represent a diagnostic challenge, as it can be misdiagnosed as papilledema, resulting in an imaging work-up for pseudotumor cerebri, optic neuritis, or an intracranial lesion. This often leads to multiple unnecessary clinical and diagnostic studies that can increase patient anxiety and lead to inappropriate utilization of resources. Although B scan sonography remains superior in detection of ODD, CT may provide crucial, clinically relevant information, especially in the setting of increased intracranial pressure.
REFERENCES
- Hingwala DR, Kesavadas C, Thomas B, Kapilamoorthy TR, Sarma PS. Imaging signs in idiopathic intracranial hypertension: Are these signs seen in secondary intracranial hypertension too? Ann Indian Acad Neurol. 2013;16(2):229-233.
- Tuğcu B, Özdemir H. Imaging Methods in the Diagnosis of Optic Disc Drusen. Turk J Ophthalmol. 2016; 46(5):232-236.
- Kurz-Levin MM, Landau K. A comparison of imaging techniques for diagnosing drusen of the optic nerve head. Arch Ophthalmol. 1999; 117(8):1045-1049.
- Rosenberg MA, Savino PJ, Glaser JS. A clinical analysis of pseudopapilledema. I. Population, laterality, acuity, refractive error, ophthalmoscopic characteristics, and coincident disease. Arch Ophthalmol. 1979; 97(1):65-70.
- Hu K, Davis A, O’Sullivan E. Distinguishing optic disc drusen from papilloedema. BMJ. 2008; 337:a2360.
- McNicholas MM, Power WJ, Griffin JF. Sonography in optic disk drusen: imaging findings and role in diagnosis when funduscopic findings are normal. AJR Am J Roentgenol. 1994;162(1):161-163.
- Aumiller MS. Optic disc drusen: complications and management. Optometry. 2007; 78(1):10-6.
- Davis PL, Jay WM. Optic nerve head drusen. Semin Ophthalmol. 2003; 18(4):222-242.
- Antcliff RJ, Spalton DJ. Are optic disc drusen inherited? Ophthalmology. 1999; 106(7):1278-1281.
- Lee KM, Woo SJ. Fundus autofluorescence in the buried optic disc drusen: optical coherence tomography findings. Can J Ophthalmol. 2017; 52(2):e53.
Citation
B K, E S, D R, P F.Optic Disc Drusen. Appl Radiol. 2020; (6):54-55.
November 5, 2020