Odontogenic Ghost Cell Carcinoma
Images



CASE SUMMARY
A 10-year-old presented with oral pain and swelling that had been worsening for approximately 1 week.
IMAGING FINDINGS
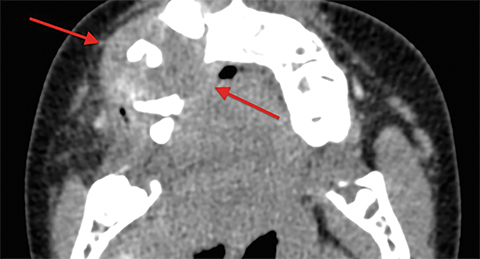
Radiographs obtained by the patient’s dentist demonstrated a right maxillary lytic lesion. Axial soft tissue and bone algorithm CT images demonstrated a lytic, soft-tissue-attenuating mass arising from the alveolar process of the right maxilla, with destruction of the buccal and lingual cortices (Figure 1). Tumor extension into the right buccal space, as well as into the hard palate, were also demonstrated. No significant periosteal reaction was identified.
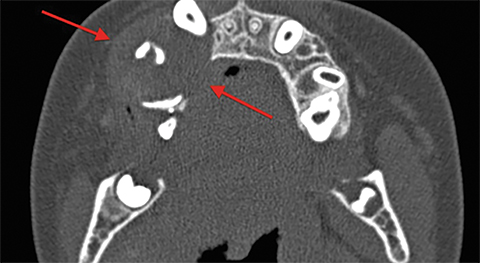
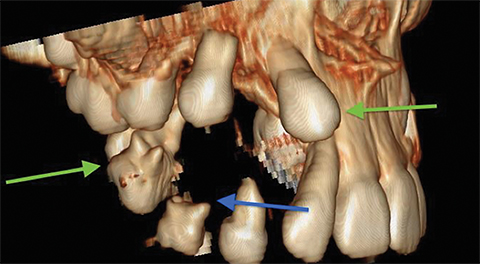
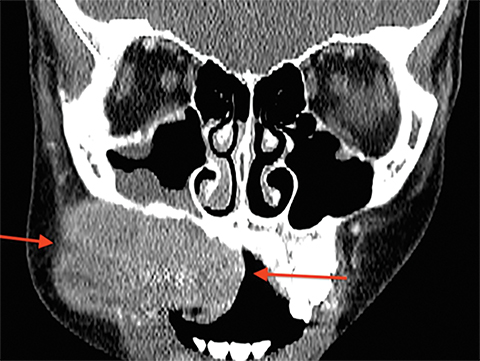
Coronal CT image viewed in bone window and a volume-rendered 3D image viewed in the RAO projection showed destruction of the maxillary alveolar process with dehiscence of the right maxillary sinus floor (Figure 2). Multiple maxillary teeth were displaced, with root resorption. Coronal and axial CT images obtained 5 weeks later, following partial resection and extraction of involved maxillary teeth, showed significant mass enlargement, with large exophytic components extending into the adjacent buccal space and oral cavity near the hard palate (Figure 3).
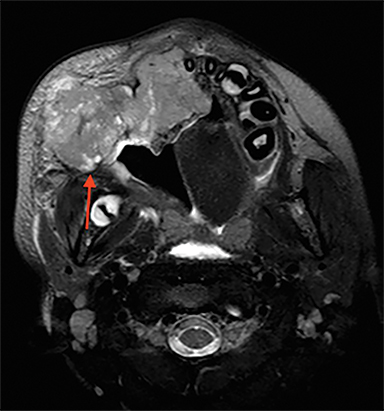
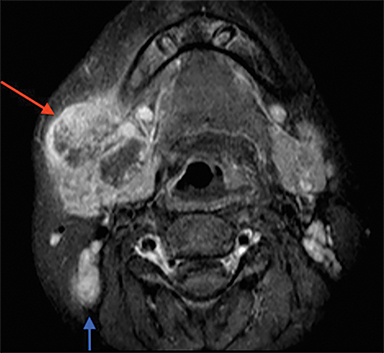
Axial and coronal magnetic resonance imaging (MRI) showed this mass to be predominantly solid and T2 hyperintense to muscle, with some small cystic components (Figure 4). Postcontrast axial T1 images showed avid contrast enhancement, as well as large, partially necrotic level 1B lymph node metastases (Figure 5).
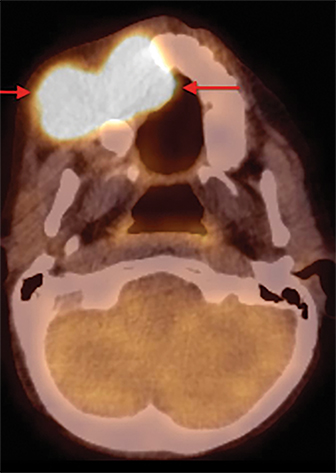
Axial PET/CT imaging demonstrated significant hypermetabolism within the mass, maximum SUV 12.1 (Figure 6).
DIAGNOSIS
Odontogenic ghost cell carcinoma.
Differential diagnosis includes giant cell granuloma, sarcoma (Ewing, rhabdomyosarcoma), lymphoma, minor salivary gland malignancy, mucoepidermoid carcinoma, ameloblastoma, Langerhans cell histiocytosis, and metastasis.
DISCUSSION
Odontogenic ghost cell carcinoma (OGCC) is an extremely rare, malignant odontogenic tumor within a spectrum of lesions composed of odontogenic epithelium-containing “ghost cells.” This term refers to characteristic eosinophilic epithelial cells that have lost their nuclei but otherwise have retained their underlying cell morphology.1 This group of tumors is classified according to their solid or cystic nature, as well as malignant behavior. The three classifications recognized by the World Health Organization consist of calcifying cystic odontogenic tumors, dentinogenic ghost cell tumors, and ghost cell odontogenic carcinomas.1 The majority of these tumors fall into the benign cystic category; only 33 cases of the malignant OGCC have been reported in the literature worldwide. These tumors show a peak occurrence in the fourth decade of life, ranging from 13 to 72 years of age.2 OGCC occurs four times more commonly in males and seems to have a predilection for patients of Asian descent.3 Clinical presentation is normally characterized as a long-term swelling followed by more rapid onset of pain and swelling at the tumor site. Many of these lesions are believed to represent malignant transformation of a preexisting calcifying odontogenic tumor.
Imaging features vary, with no specific radiologic features that allow confident diagnosis based on imaging characteristics alone. Therefore, OGCC remains a predominantly histologic diagnosis. Most reported tumors have occurred in the maxilla (70%), with the balance occurring within the mandible. Also, in most of the reported cases the lesions are described as mixed radiolucent and radiopaque with poorly defined margins. These tumors often invade surrounding structures, particularly the paranasal sinuses and orbits. Displacement of teeth and root resorption may also be seen.
Clinical outcomes in the reported cases of OGCC are variable and unpredictable. Recurrence is common; the 5-year patient survival rate among the reported cases is 73%.1 Wide resection is recommended for all tumors; supplemental postoperative radiation and adjuvant chemotherapy may be recommended.3
CONCLUSION
Although rare and predominantly a histologic diagnosis, odontogenic ghost cell carcinoma is a differential consideration when presented with an aggressive lesion arising in the maxilla.
REFERENCES
- Neville B, Damm D, Allen C, Chi A. Odontogenic cysts and tumors. In: Oral and Maxillofacial Pathology. 4th ed. St. Louis, MO: Elsevier, Inc; 2016:15, 632-689.
- Nazaretian S, Schenberg M, Simpson I, Slootweg P. Ghost cell odontogenic carcinoma. Int J Oral Maxillofac Surg. 2007; 36:455-458.
- Sun Z, Zhao Y, Zhang L, Li Z, Chen X, Zhang W. Odontogenic ghost cell carcinoma in the maxilla: A case report and literature review. J Oral Maxillofac Surg. 2007; 65:1820-1824.
Citation
R C, SA J, AJ T, R T.Odontogenic Ghost Cell Carcinoma. Appl Radiol. 2020; (4):42-43.
June 30, 2020