Obstructive Sialadenitis
Images


Case Summary
A middle-aged patient presented with a history of a right submandibular mass. The mass swelled with meals and poor oral hygiene. The physical exam demonstrated a mobile mass below the right body of the mandible with no lymphadenopathy. Serum lab values were unremarkable.
Imaging Findings
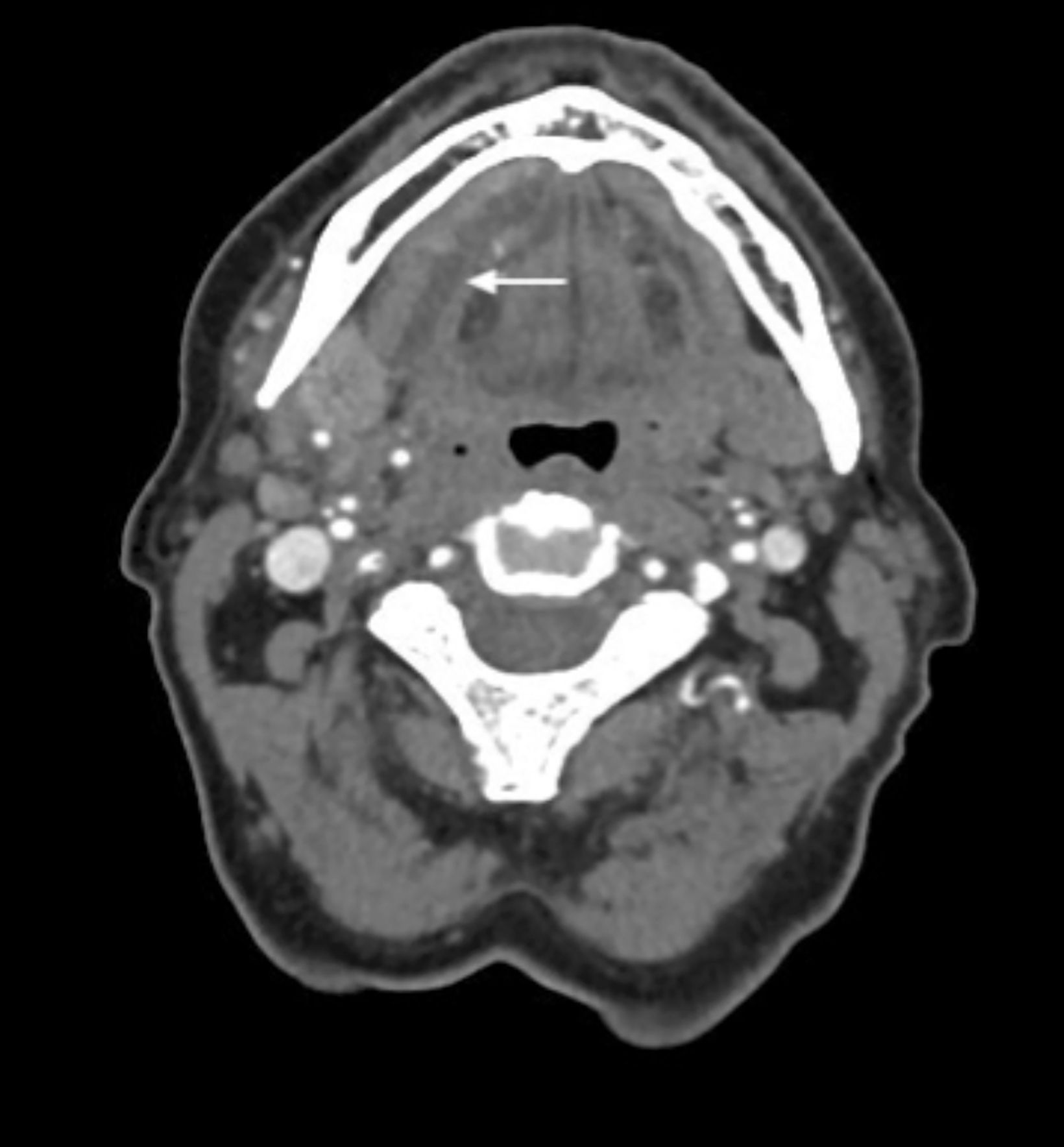
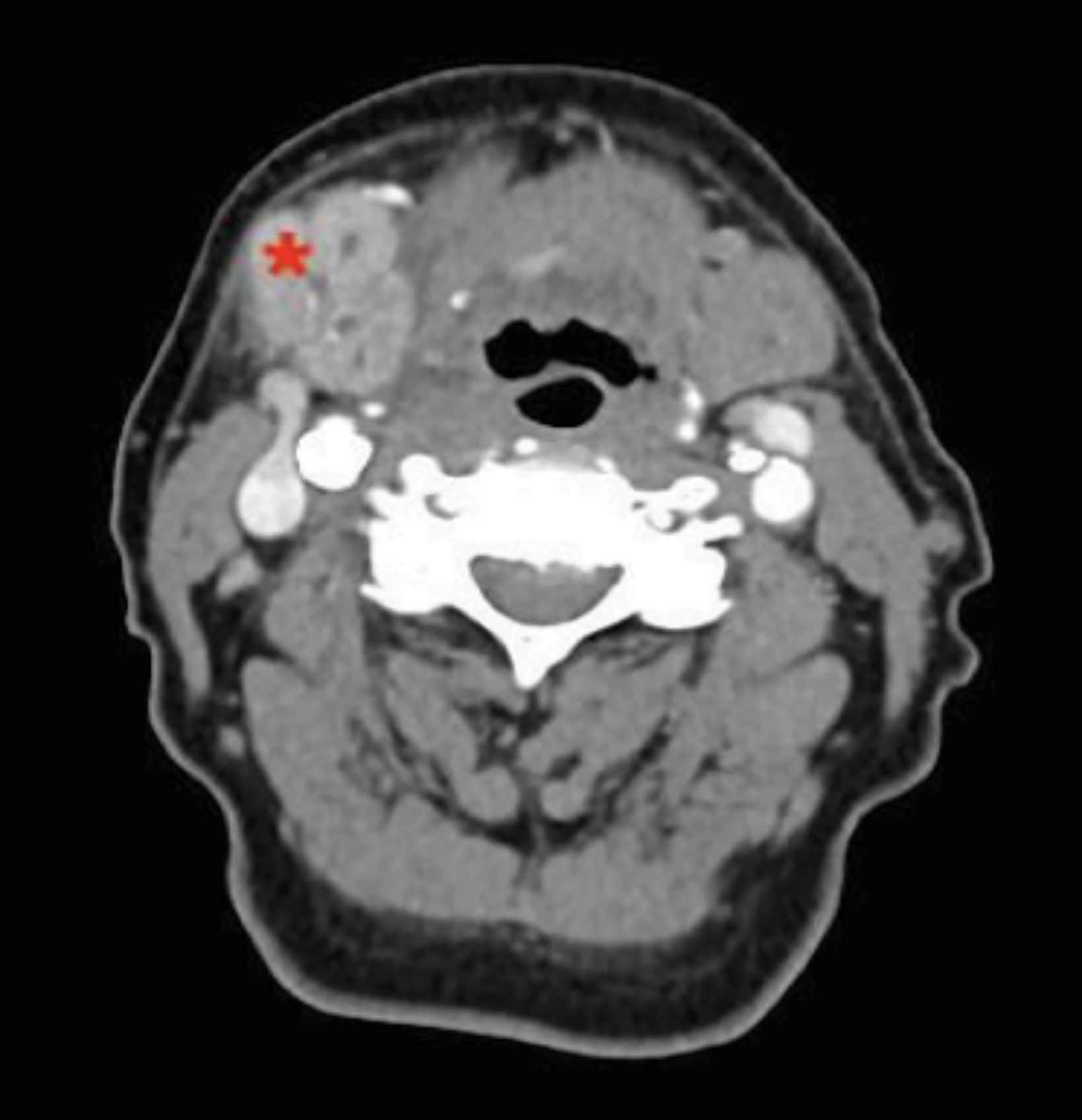
Contrast-enhanced CT neck soft tissue demonstrated a sialolith that measures 0.7 × 1.4 × 1.0 cm and a 0.7-cm dilated Wharton duct (Figures 1,2) extending from the sialolith to the submandibular gland (SMG), a markedly enlarged, enhancing right SMG with adjacent edema and intraglandular ductal dilatation.
Diagnosis
Obstructive sialadenitis secondary to sialolithiasis.
Discussion
Sialolithiasis is a common, benign pathology found in 1.2% in autopsies and 0.45% clinically. 1 Differential diagnosis includes calcified lymph nodes, reactive lymph nodes, mandibular osteomyelitis, cellulitis, benign mixed tumor of the SMG, submandibular carcinoma, and submandibular space nodal metastases. 2 The differential diagnosis for sialolith on CT imaging includes calcified lymph nodes, calcified stylohyoid ligament, tonsilloliths, and phleboliths. 2
False-negative CT can be caused by beam-hardening artifacts from dental implants that obscure the area. 3 Reportedly, 80-92% of sialoliths originate in the SMG. The parotid gland forms 6-20% of sialoliths, and the remainder are in the sublingual and minor salivary glands. 4
The high incidence of SMG calculi results from the viscous, alkaline saliva that contains concentrated amounts of calcium and phosphate. The angulated course of the Wharton duct is also implicated. 4 Most sialoliths measure less than 10 mm, with outliers up to 7 cm having been reported. 1
Risk factors include anticholinergic medications, dehydration, smoking, Sjögren disease, and AIDS. Sialolithiasis is twice as common in males. Clinical presentation ranges from asymptomatic to episodic pain and swelling exacerbated by meals and tends to be self-resolving. However, prolonged duct dilatation and salivary stasis can lead to cellulitis and abscess formation. 4 Chronically, sialadenitis can decrease salivation. Irreversible hyposalivation occurs once the gland has fully atrophied.
The American College of Radiology recommends CECT to assess for non-pulsatile neck swelling. 5 CECT was once suspected to have a higher rate of false positives as blood vessels can simulate calculi in density. However, a recent study showed no difference in the diagnostic accuracy between CECT and non-CECT. 3
Among other modalities, ultrasonography can detect stones to 1.5 mm, however it is user-dependent, with wide-ranging sensitivities (59.1% - 93.7%). 3 A study comparing ultrasound and CT found ultrasound sensitivity to be insufficient as a sole diagnostic tool. 6 Magnetic resonance imaging (MRI), conventional, and digital subtraction sialography (DSS) are second-line techniques to assess gland pathology. Conventional sialography and DSS require cannulating the os of the Wharton duct, which is technically challenging and risks ductal injury. 7
Successful DSS can visualize stones located in third-order branches of the ductal system and demonstrates higher sensitivity than MRI for chronic sialadenitis and sialolithiasis. 7 MR sialography is a noninvasive method whereby stationary fluids appear hyperintense on heavily T2 sequences. It is sufficient to diagnose ductal stenosis and sialolithiasis. 7 Sialendoscopy is a minimally invasive tool that is both diagnostic and therapeutic for a variety of nontumoral salivary gland pathologies. 8
Conservative treatment for symptomatic sialolithiasis involves glandular massage, pharmacological agents that increase salivary flow, antibiotics, and irrigation. 9 Stones more amenable to conservative treatments are small, round, mobile, and distal. 10 Gland-sparing therapies include lithotripsy or lasers to fragment the calculi, but this is contraindicated during acute sialadenitis. 1,9
Sialendoscopy is a means of gland-sparing stone removal whereby a 1.1 mm endoscope with an attached basket is used to retrieve the stone from within the duct. 9 A study found success in combining external lithotripsy and sialendoscopy for advanced sialolithiasis. 8 Refractory SMG sialolithiasis can be treated with surgical extirpation via two routes. Calculi in the anterior SMG duct are removed transorally, while posterior stones are removed with the entire gland. 2
Conclusion
Sialolithiasis is a common salivary gland pathology that presents with pain and swelling during meals but also can be asymptomatic. The most common site is the SMG Wharton duct. Sialoliths can result in abscess, cellulitis, or ductal dilation. The recommended imaging is contrast-enhanced neck CT, in order to visualize stones and local inflammation, and to rule out other causes such as lymphadenitis or tumors.
DSS and conventional sialography, which involve injecting contrast into the os of the duct, have a high sensitivity for diagnosing sialolithiasis but risk ductal injury. MR sialography noninvasively visualizes the ductal system but has lower sensitivity than DSA or conventional sialography. Ultrasound has generally proven insufficient for this pathology. Smaller, mobile stones can be conservatively treated with gland massage, cholinergic drugs, or lithotripsy. More aggressive treatment includes transoral sialoendoscopy or extraoral gland removal.
References
- Capaccio P, et al. Modern management of obstructive salivary diseases. Acta Otorhinolaryngol Italica. 2007;27:161–172.
- Harnsberger HR. Head and Neck: Diagnostic Imaging. 2004;III:4–22.
- Purcell YM, et al. The diagnostic accuracy of contrast-enhanced CT of the neck for the investigation of sialolithiasis. Am J Neuroradiol. 2017;38:2161–2166.
- Kessler AT, Bhatt AA. Review of the major and minor salivary glands, part 1: anatomy, infectious, and inflammatory processes. J Clin Imaging Science. 2018;8:47.
- Aulino JM, et al. Variant 1: Nonpulsatile neck mass(es). Not parotid region ... https://acsearch.acr.org/docs/69504/Narrative. Published 2018.
- Thomas WW, et al. Accuracy of ultrasonography and computed tomography in the evaluation of patients undergoing sialendoscopy for sialolithiasis. Otolaryngology-Head and Neck Surgery. 2017;156:834–839.
- Kalinowski M, Heverhagen JT, Rehberg E, Klose KJ, Wagner HJ. Comparative study of MR sialography and digital subtraction sialography for benign salivary gland disorders. Am J Neuroradiol. 2002;23:1485-1492.
- Nahlieli O, Shacham R, Zaguri A. Combined external lithotripsy and endoscopic techniques for advanced sialolithiasis cases. Int J Oral and Maxillol Surg. 2010;68:347-353.
- Mandel L. Salivary Gland Disorders. Medical Clinics of North America. 2014;98:1407–1449.
- Cox D, et al. Prognostic factors for therapeutic sialendoscopy. J Laryngol Otol. 2017;132:275–278.
References
Citation
S T, V L.Obstructive Sialadenitis . Appl Radiol. 2021; (6):48-50.
November 6, 2021