MRI in abdominopelvic emergencies
Images



Acute abdominal pain is a common symptom for patients presenting to the emergency department (ED). It could be due to a variety of reasons, with etiologies ranging from innocuous to life threatening. Imaging is often required to confirm the diagnosis and to make sure that only appropriate patients proceed to the operating room. Computed tomography (CT) is the imaging modality of choice in these situations,except when acute cholecystitis is suspected. CT has been shown to have significant effects on patient management, and its cost-effectiveness has been proven.1
However, with the rising use of CT, there has been a rising concern about its harmful effects, especially the risk of induced cancers.2 Magnetic resonance imaging (MRI) does not involve the use of ionizing radiation and has the potential of answering the diagnostic questions inpatients presenting to the ED with acute abdominal pain.
Yet, it is not possible to use MRI in all clinical situations. In this article, we examine the role of MRI in abdominopelvic emergencies and the practical issues involved. We will also discuss specific issues related to MRI, such as allergic reactions to gadolinium chelates, side-effects of gadolinium, nephrogenic systemic fibrosis (NSF), and its use in patients with renal failure and on dialysis. The use of MRI in vulnerable populations like pregnant women and children is also discussed. This is followed by a brief description of the MRI protocol used at our institute and the contraindications to MRI.
Advantages and disadvantages
MRI has many advantages over CT, such as lack of ionizing radiation, superior contrast resolution, multiplanar capabilities, and an excellent safety profile of gadolinium chelates. However, despite these advantages, MRI is not currently utilized extensively for imaging patients with acute abdominal pain. There are many reasons for this. First and foremost, the literature supporting the use of MRI for abdominopelvic emergencies is sparse.3 Good accuracy of MRI has been reported for acute appendicitis, acute cholecystitis, and sigmoid diverticulitis.4-6 However,most of these studies are limited by small sample sizes and have been limited to special populations like pregnant women. Secondly, MRI is costlier than CT and ultrasound (US), and availability is limited. It also takes much more time to complete an MRI examination. Lastly, most radiologists are not as familiar with MRI features of acute abdominal and pelvic conditions as they are with CT and US features.1 Table 1 illustrates the reasons why MRI is not extensively used in the clinical setting of acute abdominal and pelvic emergencies.
Contrast allergy
Allergic reactions to iodinated contrast are common and sometimes can be severe and life-threatening. The majority of these reactions are not due to true Ig-E mediated allergy, but due to release of histamine from mast cells due to the osmolarity of the contrast agent or binding of contrast molecules with membrane receptors. An activation of the complement cascade or the kinin system may also be responsible for histamine release.7 A previous severe allergic reaction to iodinated contrast increases the risk of subsequent reactions and may necessitate the use of alternative imaging methods.8 MRI can be of help in such situations because of its high intrinsic contrast resolution, and contrast administration may be avoided altogether.1 However, even gadolinium-based contrast agents may cause an allergic reaction. An adverse reaction rate of 0.17 to 0.24 has been reported. However, the rate of severe allergic reactions is less than that of iodinated contrast media.9-12 Also, it is important to note that there is a 2.3 to 3.7 times increased incidence of allergic reactions to gadolinium in patients who have had an allergic reaction to iodinated contrast. The role of premedication to mitigate reaction to gadolinium has not been well studied in clinical trials. It is recommended that a different class of gadolinium chelate be used in these patients rather than the one that had caused the allergic reaction. In our own institute, the authors do not prescribe premedication to patients who are getting gadolinium and have an allergy to iodinated contrast. The guidelines used in our institution for establishing the risk of contrast reaction are presented in Table 2, and the guidelines for premedication are depicted in Table 3.
Renal dysfunction
Another controversial issue regarding the use of gadolinium is its effect on renal function and induced nephropathy. As consolidated by numerous studies, gadolinium does not cause contrast-media induced nephropathy in patients with normal renal function.12,13 The safety of gadolinium in patients with renal insufficiency is less clear. There are multiple reports in the literature that suggest gadolinium may cause contrast-media induced nephropathy at all doses.14,15 To the contrary, there are also studies that suggest gadolinium does not worsen renal function in patients with renal insufficiency.16-18 As such, there is no conclusive evidence of either safety or toxicity of gadolinium in renal insufficiency.
Nephrogenic systemic fibrosis
Nephrogenic systemic fibrosis (NSF) may develop in patients with renal failure on gadolinium administration and may even be life-threatening. Patients with end-stage renal disease, acute renal failure, and those on dialysis are particularly vulnerable. It is clinically identified by a thickening and hardening of the skin, usually involving the upper and lower extremities. The clinical course is usually progressive,and patients may develop joint contractures as well as systemic fibrosis. Diagnosis is made by skin or muscle biopsy that demonstrates an increase in fibroblasts and elastic fibers with mucin deposition and a thickening of collagen bundles. It has been hypothesized that free gadolinium ion released from unstable chelates is deposited in tissues and induces the recruitment of fibrocytes.19
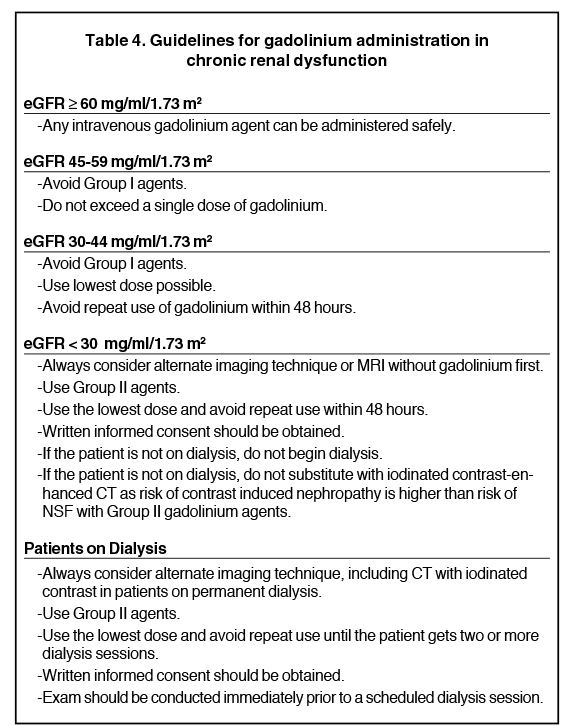
NSF is mostly seen with an estimated glomerular filtration rate of < 30 ml/min/1.63m2. It occurs most commonly in patients who receive high doses of gadolinium, either in a single dose or cumulatively.20,21 Hence, the lowest possible dose should be used and administration should not be repeated for the next several days if gadolinium must be administered to these patients. Also, Group II gadolinium-based agents, such as gadoteridol and gadobenate dimeglumine, should be used rather than Group I agents like gadodiamide and gadopentatatedimeglumine, which are associated with the greatest number of NSF cases. For patients on chronic dialysis, CT with iodinated contrast is preferred over MRI with gadolinium. Our departmental guidelines for administration of gadolinium in chronic renal dysfunction, according to the estimated glomerular filtration rate (eGFR), are presented in Table 4.
MRI in pregnant women
MRI has been used in the evaluation of pregnant women with acute abdominal or pelvic pain. In a retrospective analysis of MRI in pregnant women with acute abdominal pain, an accuracy of 94.1% in detection of patients requiring surgical/interventional treatment has been reported.4 In another retrospective study, in 29 pregnant women, MRI was able to correctly detect the disease process in all but one patient.22 Common etiologies of abdominal pain in pregnant women include appendicitis, inflammatory bowel disease (IBD), cholecystitis, choledocholithiasis, ureteric calculi, pyelonephritis, ovarian torsion, and degenerating fibroids.
MRI features of common disorders
MRI findings of the common abdominal disorders have been well described in the literature. In retrospective analysis, the sensitivity and specificity of MRI in the diagnosis of acute appendicitis in pregnant patients was reported to be 90.0% and 98.1% respectively.4 Signs of appendicitis on MRI are a caliber of ≥ 7 mm, wall thickening that appears hyperintense on T2 and hypointense on T1 images, and periappendiceal fluid/fat stranding.23 MRI has been shown to be highly accurate in the detection of disease in patients with known or suspected IBD.24,25 It can readily detect complications of inflammatory bowel disease like abscesses, obstruction, and intussusception. MRI is of particular advantage in IBD as repeated imaging is often needed and ionizing radiation can be avoided.
US is commonly used in the initial evaluation of suspected acute cholecystitis.26 However, calculi in the cystic duct or gallbladder neck may not always be visualized. MRI has been reported to have a higher sensitivity in detection of cholecystitis. The MRI findings in acute cholecystitis are gallstones, wall thickness of > 3 mm, and pericholecystic fluid.27-30 US is insensitive for the diagnosis of choledocholithiasis as the distalCBD is commonly not visualized. MR cholangiopancreaticography has been shown to have a high sensitivity and specificity for detection of biliary calculi in various studies as compared to the gold standard, endoscopic retrograde cholangiopancreaticography (ERCP). The biliary calculi appear as dependent hypointense structures in the hyperintense bile on T2-weighted images.31-33 MR is also useful for imaging of patients with acute pancreatitis to delineate the extent of inflammation and necrosis and detect complications. It can detect all the components of acute pancreatitis, such as pancreatic swelling, fluid, fat stranding, pseudocysts, hemorrhage, and necrosis and is comparable to CT in this respect.34,35
MRI has recently begun to be used in imaging of suspected pyelonephritis. The involved areas of the kidneys appear hypointense on T1- and hyperintense on T2-weighted images without appearance on postgadolinium T1-weighted images. These areas also demonstrate restricted diffusion.36-38 In the diagnosis of renal and ureteric and renal calculi, MRI relies on indirect detection of calculi by demonstrating wall thickening,edema, and hydronephrosis. It is not sensitive for direct detection of calculi that are < 1 cm in size.39 MRI can also be useful in patients with ovarian torsion. Although it is neither sensitive nor specific for diagnosis, it can help rule out torsion when normal ovaries are identified and confirm the diagnosis when specific features, such as a twisted pedicle or lack of ovarian enhancement, are demonstrated.40 The experience withMRI in imaging of ectopic pregnancy is limited. This entity can be diagnosed when there is no intrauterine sac in a pregnant woman, and other features like hemoperitoneum, hematosalpinx, or complex adnexal mass are detected on MRI. T1-weighted images are particularly helpful in this scenario, as blood products are readily identified. A well-defined extrauterine gestational sac is seldom seen.41
MRI in children
Exposure to ionizing radiation is particularly concerning in children, and there has been a push to replace CT with alternative imaging that does not involve radiation exposure whenever possible. MRI is a very promising tool in this regard. The accuracy of MRI for the diagnosis was prospectively studied in children with acute abdominal pain. The investigators used selected sequences with the mean duration of MR exams being 5 min 40 sec. Oral or intravenous contrast was not used. A sensitivity of 100% and specificity of 99% were reported.42 MRI may also be used for imaging of IBD in children.
MRI protocol
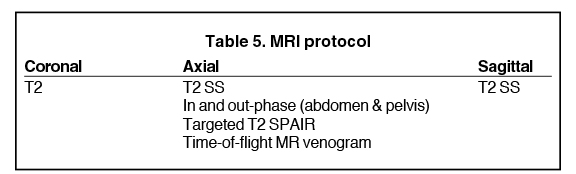
It is essential to tailor the MRI examination protocol for each and every patient so that the examination time is minimized and the relevant clinical question is answered. Gadolinium is not necessary in all patients, and specific sequences may be necessary in some patients. Breath-hold MRI may be used in cooperative patients while free-breathing protocols should be used for patients who cannot hold their breath. The basic protocol used for MRI of the abdomen at the University of Washington Medical Center is illustrated in Table 5. However, most of the time, it is modified according to the specific clinical scenario at hand.
Contraindication to MRI
This review cannot be complete without identifying situations when MRI should not be used. MRI cannot be performed in patients with claustrophobia and cardiac pacemakers. Also, in intensive care unit patients, it is difficult to perform MRI as most of the life support and monitoring equipment may not be MRI compatible. MRI is considered to be safe in pregnancy, and no harmful fetal effects have been reported to date.43,44 No adverse effects of gadolinium on human fetuses have been reported in its use in pregnant women. However, because there is no large-scale scientific data yet available, it is recommended that gadolinium be used in pregnant women only when the benefits of its use surpass the potential risk to the fetus, the information desired cannot be obtained from an alternate imaging study, and it would be harmful to wait until the patient is not pregnant.45,46
Conclusion
MRI can be used to answer the diagnostic question in patients with acute abdominopelvic emergencies in specific clinical situations. It provides high-intrinsic contrast resolution, and hence, contrast-media administration and their side effects may be avoided altogether. Even if contrast medium is required, the rate of allergic reaction to gadolinium is less than that of iodinated contrast. However, gadolinium should be used with caution in renal dysfunction as it can cause NSF. MRI is particularly useful in pregnant patients and children as they are more susceptible to radiation-induced damage. Unfortunately, MRI cannot be used in all clinical situations due to limitations posed by the magnetic field, time, costs, and availability. However, in situations where it can be used, MRI can go a long way in reducing the overall radiation burden and incidence of serious allergic reactions.
REFERENCES
- Stoker J, Randen A, Lameris W, Boermeester MA. Imaging patients with acute abdominal pain. Radiology. 2009;253:31-46.
- Trinavarat P, Kritsaneepaiboon S, Rongviriyapanich C, et al. Radiation dose from CT scanning: Can it be reduced? Asian Biomedicine. 2011;5: 13-21.
- Stoker J. Magnetic resonance imaging and the acute abdomen. Br J Surg. 2008;95:1193-1194.
- Oto A, Ernst RD, Ghulmiyyan LM, et al. MR imaging in the triage of patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34:243-250.
- Heverhagen JT, Sitter H, Zielke A, Klose KJ. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum. 2008;41: 1810-1815.
- Oh KY, Gilfeather M, Kennedy A, et al. Limited abdominal MRI in the evaluation of acute right upper quadrant pain. Abdom Imaging. 2003;28:643-651.
- Morkos SK. Acute serious and fatal reactions to contrast media: Our current understanding. Br J Radiol. 2005;78:686-693.
- Saini S, Seltzer SE, Bramson RT, et al. Technical cost of radiologic examinations: Analysis across imaging modalities. Radiology. 2000;216:269-272.
- Idee JM, Pine E, Prigent P, Corot C. Allergy-like reactions to iodinated contrast agents. A critical analysis. Fundam Clin Pharmacol. 2005;19: 263-281.
- Nelson KL, Gifford LM, Lauber-Huber C, et al. Clinical safety of gadopentetate dimeglumine. Radiology. 1995;2:439-443.
- Niendorf H, Dinger J, Haustein J, et al. Tolerance data of Gd-DTPA: A review. Eur J Radiol. 1991;13:15-20.
- Murphy KJ, Brunberg JA, Cohan RH. Adverse reactions to gadolinium contrast media: A review of 36 cases. AJR Am J Roentgenol. 1996;167:847-849.
- Li A, Wong CS, Wong MK, et al. Acute adverse reactions to magnetic resonance contrast media gadolinium chelates. Br J Radiol. 2006;79:368-371.
- Niendorf HP, Haustein J, Cornelius I, et al. Safety of gadolinium-DTPA: Extended clinical experience. Magn Reson Med. 1991;22:222-228.
- Sam AD 2nd, Morasch MD, Collins J, et al. Safety of gadolinium contrast angiography in patients with chronic renal insufficiency. J Vasc Surg. 2003;38:313-318.
- Ergun I, Keven K, Uruc I, et al. The safety of gadolinium in patients with stage 3 and 4 renal failure. Nephrol Dial Transplant. 2006; 21:697-700.
- Tombach B, Bremer C, Reimer P, et al. Renal tolerance of a neutral gadolinium chelate (gadobutrol) in patients with chronic renal failure: Results of a randomized study. Radiology. 2001;218:651-657.
- Swan SK, Lambrecht LJ, Townsend R, et al. Safety and pharmacokinetic profile of gadobenate dimeglumine in subjects with renal impairment. Invest Radiol. 1999;34:443-448.
- Nainani N, Panesar M. Nephrogenic systemic fibrosis. Am J Nephrol. 2009;29:1-9.
- Joffe P, Thomsen HS, Meusel M. Pharmacokinetics of gadodiamide injection in patients with severe renal insufficiency and patients undergoing hemodialysis or continuous ambulatory peritoneal dialysis. Acad Radiol. 1998;5:491-502.
- Wertman R, Altun E, Martin DR, et al. Risk of nephrogenic systemic fibrosis: Evaluation of gadolinium chelate contrast agents at four American universities. Radiology. 2008;248:799-806.
- Kallen AJ, Jhung MA, Cheng S, et al. Gadolinium-containing magnetic resonance imaging contrast and nephrogenic systemic fibrosis: A case-control study. Am J Kidney Dis. 2008;51:966-975.
- Birchard KR, Brown MA, Hyslop WB, et al. MRI of acute abdominal and pelvic pain in pregnant patients. AJR Am J Roengenol. 2005;184: 452-458.
- Singh A, Danrad R, Hahn PF, et al. MR Imaging of the acute abdomen and pelvis: Acute appendicitis and beyond. Radiology. 2007;27:1419-1431.
- Umschaden HW, Szoler D, Gasser J, et al. Small bowel disease: Comparison of MR enteroclysis images with conventional enteroclysis and surgical findings. Radiology. 2000;215:717-725.
- Koh DM, Miao Y, Chinn RJ et al. MR imaging evaluation of the activity of Crohn’s disease. AJR Am J Roengenol. 2001;177:1325-1332.
- O’Connor OJ, Maher MM. Imaging of cholecystitis. AJR Am J Roentgenol. 2011 196:367-374.
- Park MS, Yu JS, Kim YH, et al. Acute cholecystitis: Comparison of MR cholangiography and US. Radiology. 1998;209:781-785.
- Weissleder R, Stark DD, Compton CC, et al. Cholecystitis: Diagnosis by MR imaging. Magn Reson Imaging. 1998;6:345-348.
- Loud PA, Semelka RC, Kettritz U, et al. MRI of acute cholecystitis: Comparison with normal gall bladder and other entities. Magn Reson Imaging. 1996;14:349-355.
- Hakkanson K, Leander P, Ekberg O, Hakkanson HO. MR imaging in clinically suspected cholecystitis: A comparison with ultrasonography. Acta Radiol. 2000;41:322-328.
- Shanmugam V, Beattie GC, Yule SR, et al. Is magnetic resonance cholangiopancreaticography the new gold standard in biliary imaging? Br J Radiol. 2005;78:888-893.
- Hurter G, Vries CD, Potgieter PH, et al. Accuracy of MRCP compared with ERCP in the diagnosis of bile duct disorders. South African Journal of Radiology. 2008;12:14-22.
- O’Connor OJ, O’Neill S, Maher MM. Imaging of biliary tract disease. AJR Am J Roentgenol. 2011;197:551-558.
- Amano Y, Oishi T, Takahashi M, Kumazaki T. Nonenhanced magnetic resonance imaging of mild acute pancreatitis. Abdom Imaging. 2001;26:59-63.
- O’Connor OJ, McWilliams S, Maher MM. Imaging of acute pancreatitis. AJR Am J Roengenol. 2011;197:221-225.
- Pascale AD, Piccoli GB, Priola SM, et al. Diffusion-weighted magnetic resonance imaging: New perspectives in the diagnostic pathway of non-complicated acute pyelonephritis. Eur Radiol. 2013;231:3077-3086.
- Vivier PH, Sallem A, Beurdeley M, et al. MRI and suspected acute pyelonephritis in children: Comparison of diffusion-weighted imaging with gadolinium-enhanced T1-weighted imaging. Eur Radiol. 2014;24:19-25.
- Faletti R, Cassinis MC, Fonio P, et al. Diffusion-weighted imaging and apparent diffusion coefficient values versus contrast-enhanced MR imaging in the identification and characterisation of acute pyelonephritis. Eur Radiol . 2013;23: 3501-3508.
- Kalb B, Sharma P, Salman K, et al. Acute abdominal pain: Is there a potential role of MRI in the setting of the emergency department in a patient with renal calculi? J Magn Reson Imaging. 2010;32:1012-1023.
- Duigenan S, Oliva E, Lee SI. Ovarian torsion: Diagnostic features on CT and MRI with pathologic correlation. AJR Am J Roentgenol. 2012;198:122-131.
- Parker RA, Yan M, Tai AW, et al. MR imaging Findings of ectopic pregnancy: A pictorial review. Radiographics.2012;32:1445-1462.
- Johnson AK, Filippi CG, Andrews T, et al. Ultrafast 3-T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis. AJR Am J Roengenol. 2012;198:1424-1430.
- De Vilde JP, Rivers AW, Price DL. A review of the current use of magnetic resonance imaging in pregnancy and safety implications for the fetus. Prog Biophys Mol Biol. 2005;87:335-353.
- Nagayama M, Watanabe Y, Okumura A, et al. Fast MR imaging in obstetrics. Radiographics. 2002;22:563-582.
- De Santis M, Straface AF, Cavaliere B et al. Gadolinium periconceptinal exposure: Pregnancy and neonatal outcome. Acta Obstet Gynecol Scand. 2007;86:99-101.
Citation
MRI in abdominopelvic emergencies. Appl Radiol.
June 5, 2014