MRI Contrast Innovation | A New High-Relaxivity, High Stability GBCA
Please see additional safety information below.
Introduction
With millions of doses administered over the past 30 years, gadolinium-based contrast agents (GBCAs) have long been recognized for their efficacy in improving the diagnostic utility of magnetic resonance imaging (MRI), as well as for their safety. However, in 2006, it was documented that in patients with severe renal dysfunction administered certain GBCAs, a sometimes-fatal disease known as nephrogenic systemic fibrosis (NSF) could develop.1 The GBCAs associated with the greatest number of NSF cases include the linear GBCAs Omniscan, Magnevist, and OptiMARK, while the macrocyclic agents Dotarem, ProHance, and Gadavist, as well as the linear agent MultiHance, were associated with few, if any, unconfounded cases of NSF.2 Additionally, many studies documented that use of a higher-relaxivity GBCA was associated with better contrast enhancement and higher diagnostic confidence;3-9 however, until 2022, the only high-relaxivity GBCA available was linear. The race was on to develop a high-relaxivity, high-stability macrocyclic GBCA. Guerbet led the way, and in September, 2022, the Food and Drug Administration (FDA) announced approval of Elucirem™ (gadopiclenol), a novel high-relaxivity, macrocyclic GBCA.
At a recent expert panel forum sponsored by Guerbet, Ahmed Abdelal, PharmD, Global Head of Medical Affairs, Interventional Imaging, and North America Head of Medical & Regulatory Affairs at Guerbet, introduced the novel high-relaxivity GBCA Elucirem. Dr. Abdelal reviewed the development, key properties, and approval process for this new contrast agent. Lawrence Tanenbaum, MD, FACR, Chief Technology Officer, Director of Advanced Imaging, and Vice President at RadNet Inc., moderated the expert panel forum. Additional participants included: Laurie Loevner, MD, Division Chief of Neuroradiology at Penn Medicine; Jeffrey Weinreb, MD, Chief of Radiology Services and Director of MRI Services at Yale New Haven Hospital; and Donna Roberts, MD, Professor of Radiology at Medical University of South Carolina. This article is based on Dr. Abdelal’s presentation, with contribution from other participants’ presentations and discussions related to use of Elucirem use in their area of expertise. An educational monograph is in development that will explore in more detail all of the presentations and discussions from this Elucirem expert panel forum.
Elucirem: A Unique Molecular Design
Dr. Abdelal explains the unique molecular design of Elucirem, and how it translates into higher relaxivity compared to any of the existing GBCAs:
“There are two ways to increase the relaxivity of a GBCA. One is to slow the rate of molecular tumbling; this is the mechanism by which MultiHance® (gadobenate dimeglumine) achieves higher relaxivity. By binding to the macromolecule albumin, the molecular tumbling rate of MultiHance is slowed and the relaxivity is increased. Another way to increase relaxivity is related to water exchange kinetics and the hydration number q (ie, the number of bound water nuclei per Gd ion). Elucirem has an increased hydration number (q=2) vs all of the other GBCAs (q=1).10 So, Elucirem possesses higher relaxivity due to two water exchange sites, not from protein binding. And, notably, the relaxivity of Elucirem is more than twice as high as that of MultiHance.10”
Elucirem Efficacy
The higher relaxivity of Elucirem would be expected to provide greater signal intensity; however, rather than pursue approval based on higher efficacy, Guerbet chose an innovative approach that focused on demonstrating equivalence at half dose, with the goal of reducing patient exposure to gadolinium (Gd). Dr. Abdelal describes the Elucirem clinical development program:
“There were two main studies upon which the approval of Elucirem was based: one in the CNS (the PICTURE trial; N=256) and one in the body (the PROMISE trial; N=304).11 Both were multicenter, randomized, double-blind, crossover studies. They had two primary objectives: to demonstrate superiority compared to unenhanced MRI (a standard FDA requirement) and to show noninferiority of Elucirem at half dose (0.05 mmol/kg) compared to a full dose (0.1 mmol/kg) of Gadavist® (gadobutrol). For the CNS study, noninferiority of half dose Elucirem vs Gadavist was indeed demonstrated. Moreover, the overall diagnostic preference of the 3 blinded readers leaned toward Elucirem, and the image quality and border delineation were comparable. The PROMISE body imaging trial results similarly showed that half dose Elucirem was noninferior to full dose Gadavist.”
Elucirem Safety
Both the adverse reaction rate results from the Phase 3 clinical trials, as well as the overall safety results from the entire clinical development program, show that Elucirem has a safety profile similar to Gadavist.11 Dr. Abdelal explains:
“In the Phase 3 clinical trials of Elucirem, the most common adverse reactions in patients receiving Elucirem (N=708) were injection site pain and headache, similar to what is seen with other GBCAs.11 Importantly, there was no statistical difference in the adverse reaction rates reported in patients receiving 0.05 mmol/kg Elucirem and those receiving 0.1 mmol/kg Gadavist. In the entire clinical development program (N=1,047 patients and healthy volunteers), it was found that: there was no prolongation of QT interval at both 0.1 mmol/kg and 0.3 mmol/kg Elucirem; clinical laboratory, vital signs, and ECG assessments raised no safety concerns; and no NSF cases were reported in any patient receiving Elucirem, including in patients with renal impairment.”
Summary
Elucirem is a high-relaxivity, macrocyclic GBCA designed to deliver high-quality brain and body lesion visualization at half the conventional Gd dose. Dr. Abdelal summarizes the unique benefits of Elucirem:
“The approved dose of Elucirem is 0.05 mmol/kg – half that of the conventional GBCAs. This lower dosing regimen is in line with recommendations of health agencies and radiology associations to reduce Gd exposure,2,12 but with no reduction in the quality of the images, and no need for further dose reduction in pediatric or renally-impaired patients.11 This is highly beneficial on two fronts: Elucirem is designed to reduce the lifetime quantity of Gd injected into patients and, as a result, to lower the amount of Gd put out into the environment, which can be another significant advantage. Elucirem was granted FDA approval after priority review, and this designation is assigned to applications for drugs that provide significant improvements in the safety or effectiveness compared to available therapies. In addition, Elucirem has been listed by the FDA among the novel drug approvals for 2022. We are very proud to bring Elucirem to market.”
References
- Thomsen HS, Morcos SK, Dawson P. Is there a causal relation between the administration of gadolinium based contrast media and the development of nephrogenic systemic fibrosis (NSF)? Clin Radiol. 2006;61:905-906.
- American College of Radiology (ACR) Website. ACR Manual on Contrast Media; 2022. Available at: https://www.acr.org/Clinical-Resources/Contrast-Manual.
- Pintaske J, Martirosian P, Graf H, et al. Relaxivity of gadopentetate dimeglumine (Magnevist), gadobutrol (Gadovist), and gadobenate dimeglumine (MultiHance) in human blood plasma at 0.2, 1.5, and 3 Tesla. Invest Radiol. 2006;41: 213-221 [erratum in Invest Radiol. 2006;41:859].
- Maravilla KR, Maldjian JA, Schmalfuss IM, et al. Contrast enhancement of central nervous system lesions: multicenter intraindividual crossover comparative study of two MR contrast agents. Radiology. 2006;240:389-400.
- Rowley HA, Scialfa G, Gao PY, et al. Contrast-enhanced MR imaging of brain lesions: a large scale intraindividual crossover comparison of gadobenate dimeglumine versus gadodiamide. AJNR Am J Neuroradiol. 2008;29:1684-1691.
- Schneider G, Maas R, Schultze Kool L, et al. Low-dose gadobenate dimeglumine versus standard dose gadopentetate dimeglumine for contrast-enhanced magnetic resonance imaging of the liver: an intra-individual crossover comparison. Invest Radiol. 2003;38:85-94.
- Martincich L, Faivre-Pierret M, Zechmann CM, et al. Multicenter, double-blind, randomized, intraindividual crossover comparison of gadobenate dimeglumine and gadopentetate dimeglumine for Breast MR imaging (DETECT Trial). 2011;258:396-408.
- Wang J, Yan F, Liu J, et al. Multicenter, intra-individual comparison of single dose gadobenate dimeglumine and double dose gadopentetate dimeglumine for MR angiography of the peripheral arteries (the Peripheral VALUE Study). J Magn Reson Imaging. 2013;38:926-937.
- Li Y, Li X, Li D, et al. Multicenter, intraindividual comparison of single-dose gadobenate dimeglumine and double-dose gadopentetate dimeglumine for MR angiography of the supra-aortic arteries (the Supra-Aortic VALUE study). AJNR Am J Neuroradiol. 2013;34:847-854.
- Robic C, Port M, Rousseaux O, et al. Physicochemical and Pharmacokinetic Profiles of Gadopiclenol: A New Macrocyclic Gadolinium Chelate With High T1 Relaxivity. Invest Radiol. 2019;54:475-484.
- Elucirem™ (gadopiclenol) [prescribing information]. Princeton, NJ: Guerbet LLC; October, 2022.
- Food and Drug Administration (FDA) website. FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body.
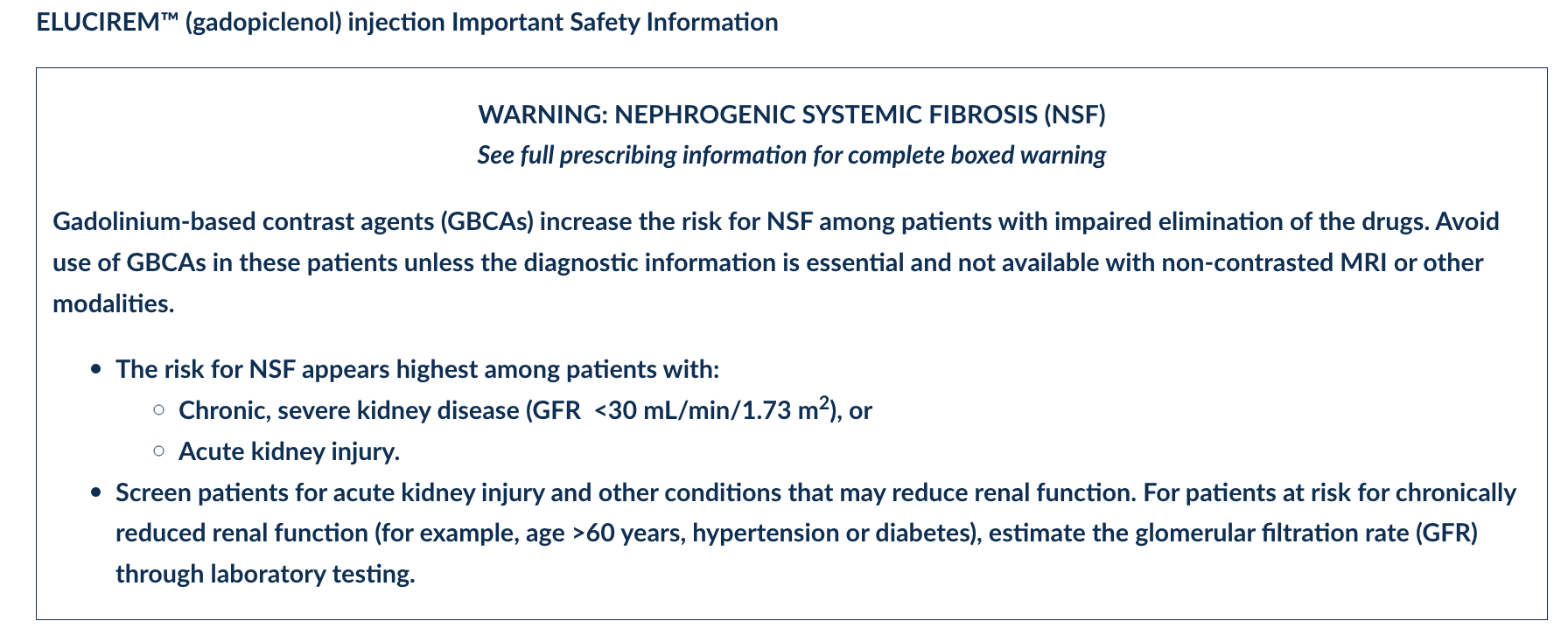
ELUCIREMTM (gadopiclenol) injection Important Safety Information
Indications and Usage
ELUCIREMTM (gadopiclenol) injection is indicated in adult and pediatric patients aged 2 years and older for use with magnetic resonance imaging (MRI) to detect and visualize lesions with abnormal vascularity in the central nervous system (brain, spine, and associated tissues), and the body (head and neck, thorax, abdomen, pelvis, and musculoskeletal system).
Contraindications
History of hypersensitivity reactions to ELUCIREM.
Warnings and Precautions
- Nephrogenic Systemic Fibrosis: GBCAs increase the risk for NSF among patients with impaired elimination of the drugs. Avoid use of GBCAs among these patients unless the diagnostic information is essential and not available with non-contrast MRI or other modalities. The GBCA-associated NSF risk appears highest for patients with chronic, severe kidney disease as well as patients with acute kidney injury.
- Hypersensitivity Reactions: With GBCAs, serious hypersensitivity reactions have occurred. In most cases, initial symptoms occurred within minutes of GBCA administration and resolved with prompt emergency treatment. Before ELUCIREM administration, assess all patients for any history of a reaction to contrast media, bronchial asthma and/or allergic disorders. These patients may have an increased risk for a hypersensitivity reaction to ELUCIREM.
- Gadolinium Retention: Gadolinium is retained for months or years in several organs. Linear GBCAs cause more retention than macrocyclic GBCAs. Consequences of gadolinium retention in the brain have not been established. Pathologic and clinical consequences of GBCA administration and retention in skin and other organs have been established in patients with impaired renal function. While clinical consequences of gadolinium retention have not been established in patients with normal renal function, certain patients might be at higher risk. These include patients requiring multiple lifetime doses, pregnant and pediatric patients, and patients with inflammatory conditions. Consider the retention characteristics of the agent when choosing a GBCA for these patients. Minimize repetitive GBCA imaging studies, particularly closely spaced studies when possible
- Acute Kidney Injury: In patients with chronically reduced renal function, acute kidney injury requiring dialysis has occurred with the use of GBCAs. The risk of acute kidney injury may increase with increasing dose of the contrast agent. Do not exceed the recommended dose.
- Extravasation and Injection Site Reactions: Injection site reactions such as injection site pain have been reported in the clinical studies with ELUCIREM. Extravasation during ELUCIREM administration may result in tissue irritation. Ensure catheter and venous patency before the injection of ELUCIREM.
- Interference with Visualization of Lesions Visible with Non-Contrast MRI: As with any GBCA, ELUCIREM may impair the visualization of lesions seen on non-contrast MRI. Therefore, caution should be exercised when Gadopiclenol MRI scans are interpreted without a companion non-contrast MRI scan.
Adverse Reactions:
In clinical trials, the most frequent adverse reactions that occurred in > 0.2% of patients who received ELUCIREM included: injection site pain, headache, nausea, injection site warmth, injection site coldness, dizziness, and localized swelling
Adverse reactions that occurred with a frequency ≤ 0.2% in patients who received 0.05 mmol/kg BW ELUCIREM included: maculopapular rash, vomiting, worsened renal impairment, feeling hot, pyrexia, oral paresthesia, dysgeusia, diarrhea, pruritus, allergic dermatitis, erythema, injection site paresthesia, Cystatin C increase, and blood creatinine increase.
Use in Specific Populations
- Pregnancy: GBCAs cross the human placenta and result in fetal exposure and gadolinium retention. There are no available data on ELUCIREM use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or other adverse maternal or fetal outcomes.
- Lactation: There are no data on the presence of ELUCIREM in human milk, the effects on the breastfed infant, or the effects on milk production. However, published lactation data on other GBCAs indicate that 0.01 to 0.04% of the maternal gadolinium dose is excreted in breast milk.
- Pediatric Use: The safety and effectiveness of ELUCIREM have not been established in pediatric patients younger than 2 years of age.
- Geriatric Use: This drug is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function.
- Renal Impairment: In patients with renal impairment, the exposure of gadopiclenol is increased compared to patients with normal renal function. This may increase the risk of adverse reactions such as nephrogenic systemic fibrosis (NSF). Avoid use of GBCAs among these patients unless the diagnostic information is essential and not available with non-contrast MRI or other modalities. No dose adjustment of ELUCIREM is recommended for patients with renal impairment. ELUCIREM can be removed from the body by hemodialysis
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please see the full Prescribing Information, including the Medication Guide, for additional important safety information.
https://www.elucirem.com/media/i5hhrokj/elucirem-uspi.pdf
GU08220135
References
Citation
MRI Contrast Innovation | A New High-Relaxivity, High Stability GBCA. Appl Radiol.
February 24, 2023