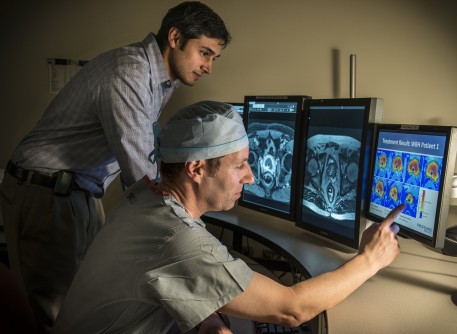
MR Scan Can Predict Radiation Side Effects in Prostate Cancer Patients
Images
A new study suggests that men who have longer prostatic urethras, the part of the urethra that travels through the prostate, may be at a higher risk of experiencing moderate, often chronic urinary side effects after receiving radiation for prostate cancer.
To date, researchers have struggled to determine any risk factors that could shed light on who might experience these types of side effects ahead of time. But now, a simple MR scan and a new metric to determine urethra length could change that.
Results from the Corewell Health study, published in the journal Academic Radiology, indicate that for every 1-centimeter increase in length of the prostatic urethra shown on the MRIs of 361 men, patients were about 60% more likely to experience issues such as having the urgency to urinate as well as needing to urinate more often. Patients with a prostatic urethra length greater than 4.6 centimeters were nearly twice as likely to develop these symptoms.
“We believe this particular area is more exposed to the radiation doses patients receive, resulting in direct inflammation,” said Kiran Nandalur, M.D., principal investigator of the study and a radiologist at Corewell Health. “While chronic moderate urinary side effects were more problematic in approximately 28% of participants after three years, the good news is less than 3% of men experienced severe urinary side effects.”
According to Dr Nandalur, there are very few known risk factors for those who will experience side effects after radiation and, in his study, factors such as type of radiation or underlying medical conditions were not predictive of symptoms. He said this underscores how challenging it has been previously to assess risk factors and highlights the need for novel and innovative methods such as the use of MRI technology in prostate cancer care.
Radiation therapy is one of the most common treatments for prostate cancer and overall, it is considered very safe. However, while radiation therapy is well tolerated by most patients, the portion of men who experience more side effects often can find their quality of life impacted for periods of time.
“Our novel MRI metric may help patients know beforehand what their risk is in developing these symptoms and help them make better and more informed decisions on a course of treatment that optimizes quality of life,” Nandalur said.
He added: “Doctors also can look at ways to better spare the prostatic urethra area from radiation and potentially decrease the side effects.”
Dr Nandalur encourages patients to be proactive in their health and with their doctors.
“I highly recommend patients talk with their urologist or radiation oncologist about getting a prostate MRI before therapy,” he said. “It is robust in diagnosing and evaluating the extent of prostate cancer and can potentially help patients maintain a better quality of life after undergoing treatment.”
Related Articles
Citation
MR Scan Can Predict Radiation Side Effects in Prostate Cancer Patients. Appl Radiol.
October 23, 2023