Metopic Suture Synostosis
Images
Case Summary
An otherwise healthy and developmentally normal infant presented with trigonocephaly with associated bi-temporal bulging and hypotelorism, first noted at birth. On examination, head circumference was 40.5 cm, which was > 99 percentile for age and gender.1 No positional plagiocephaly was noted, and the anterior fontanelle was soft and flat.
Imaging Findings
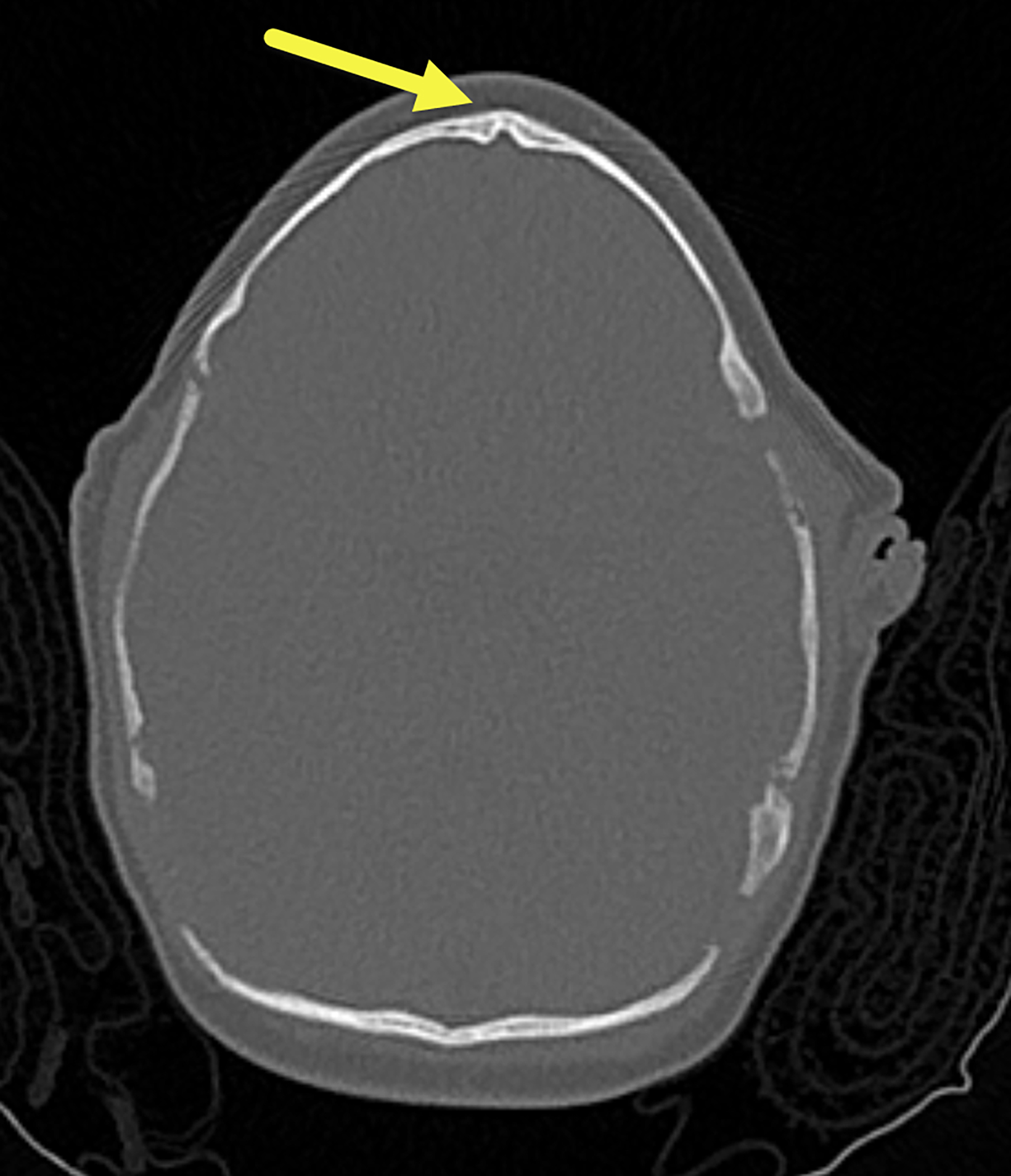
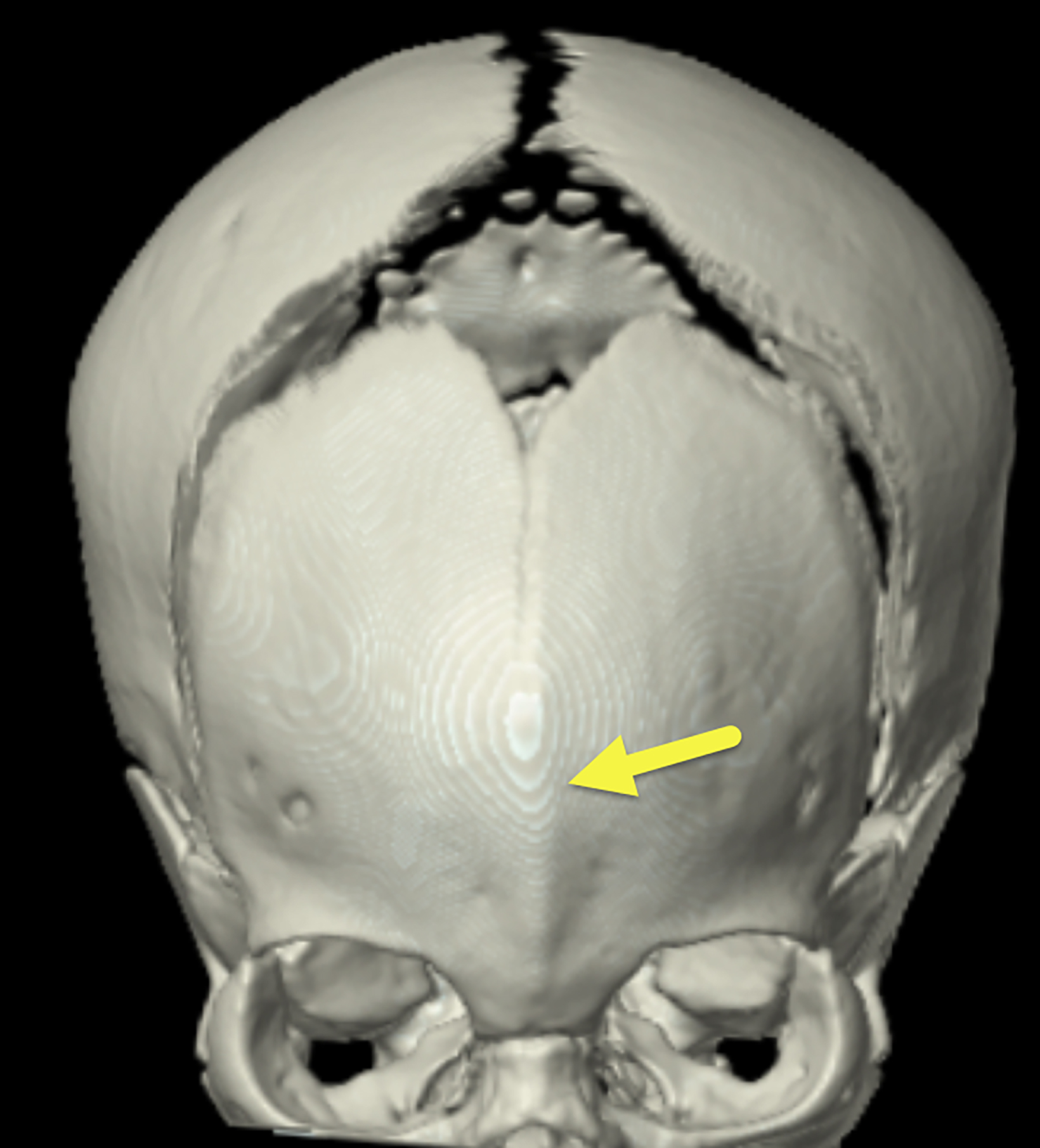
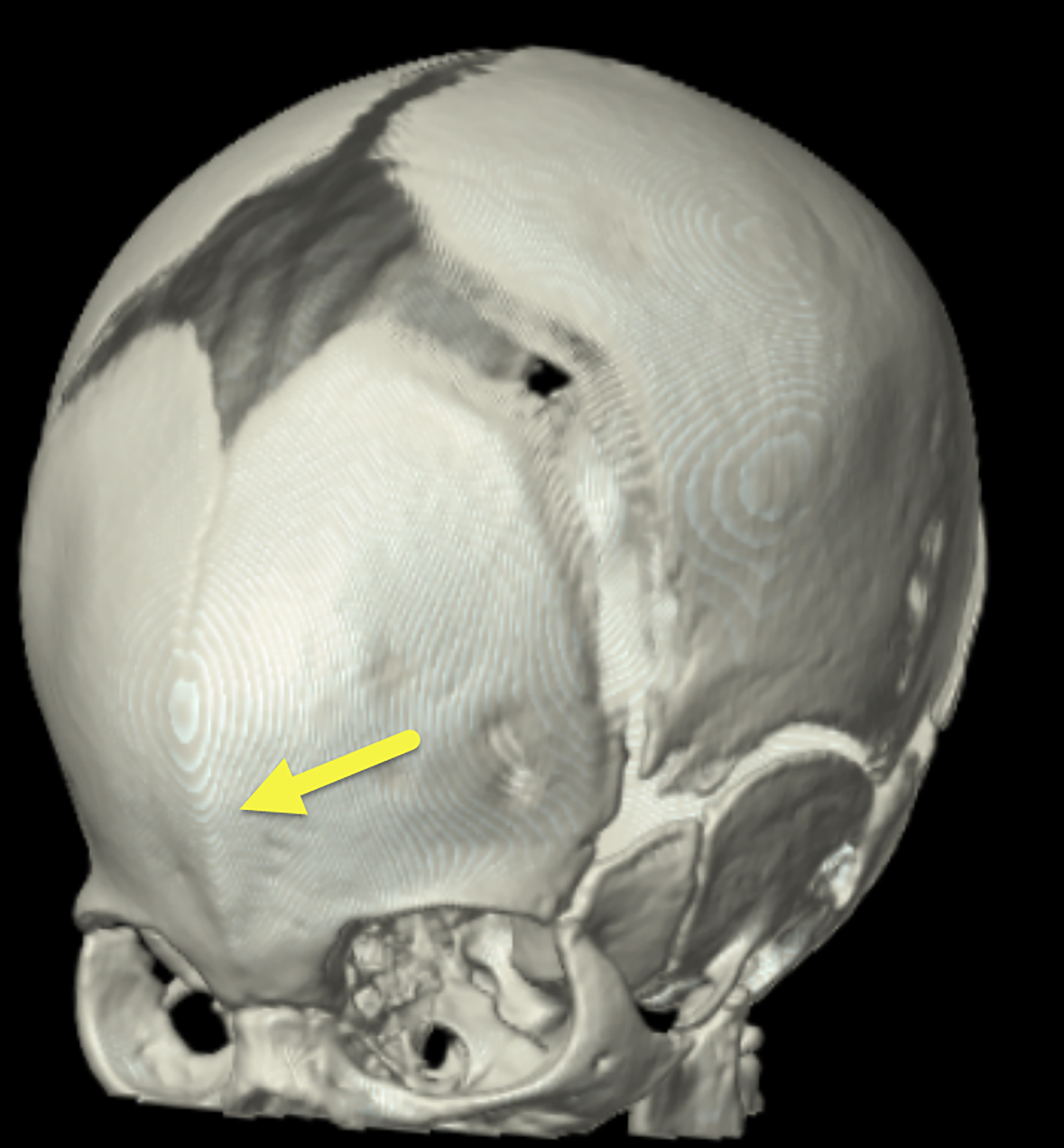
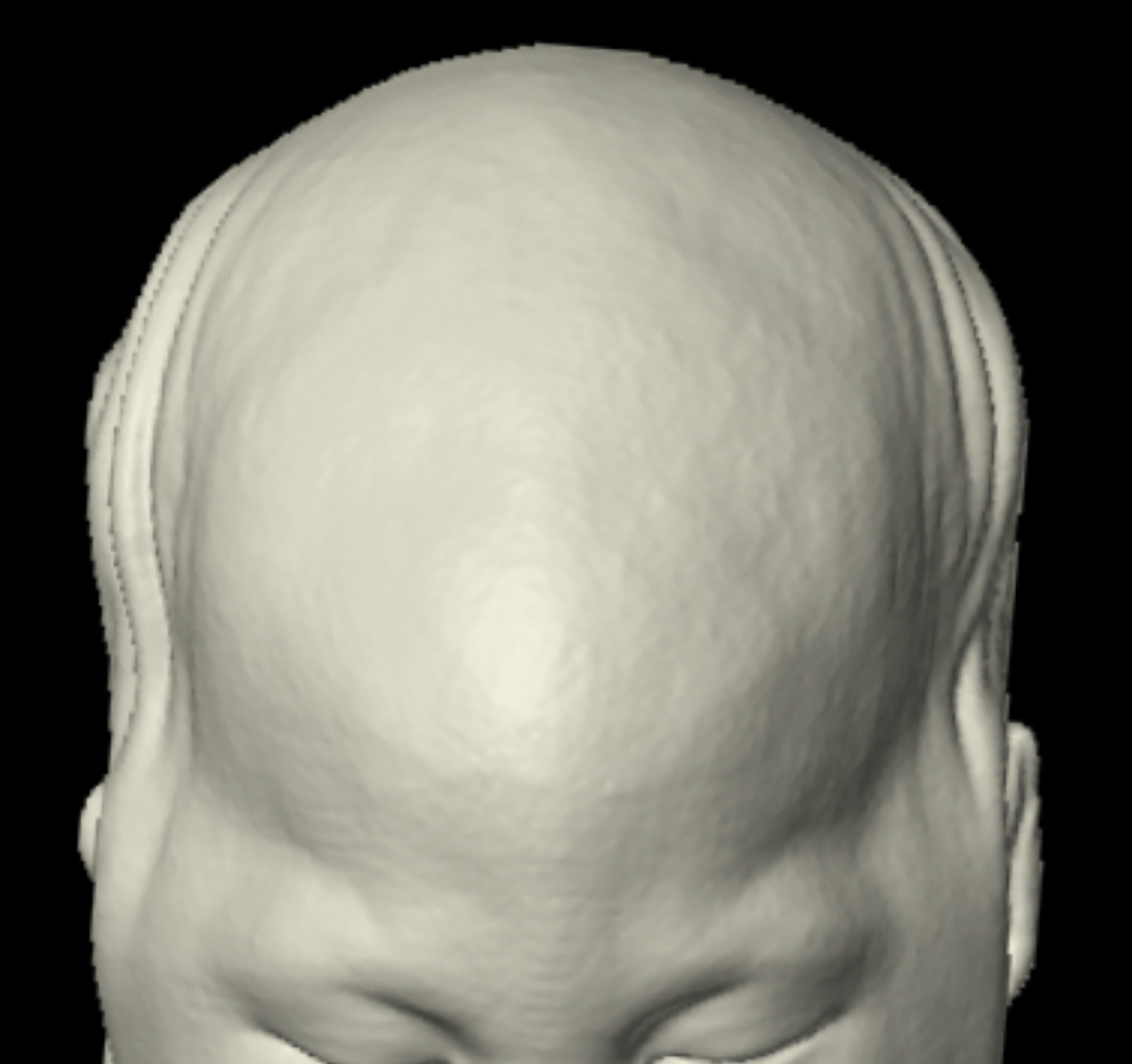
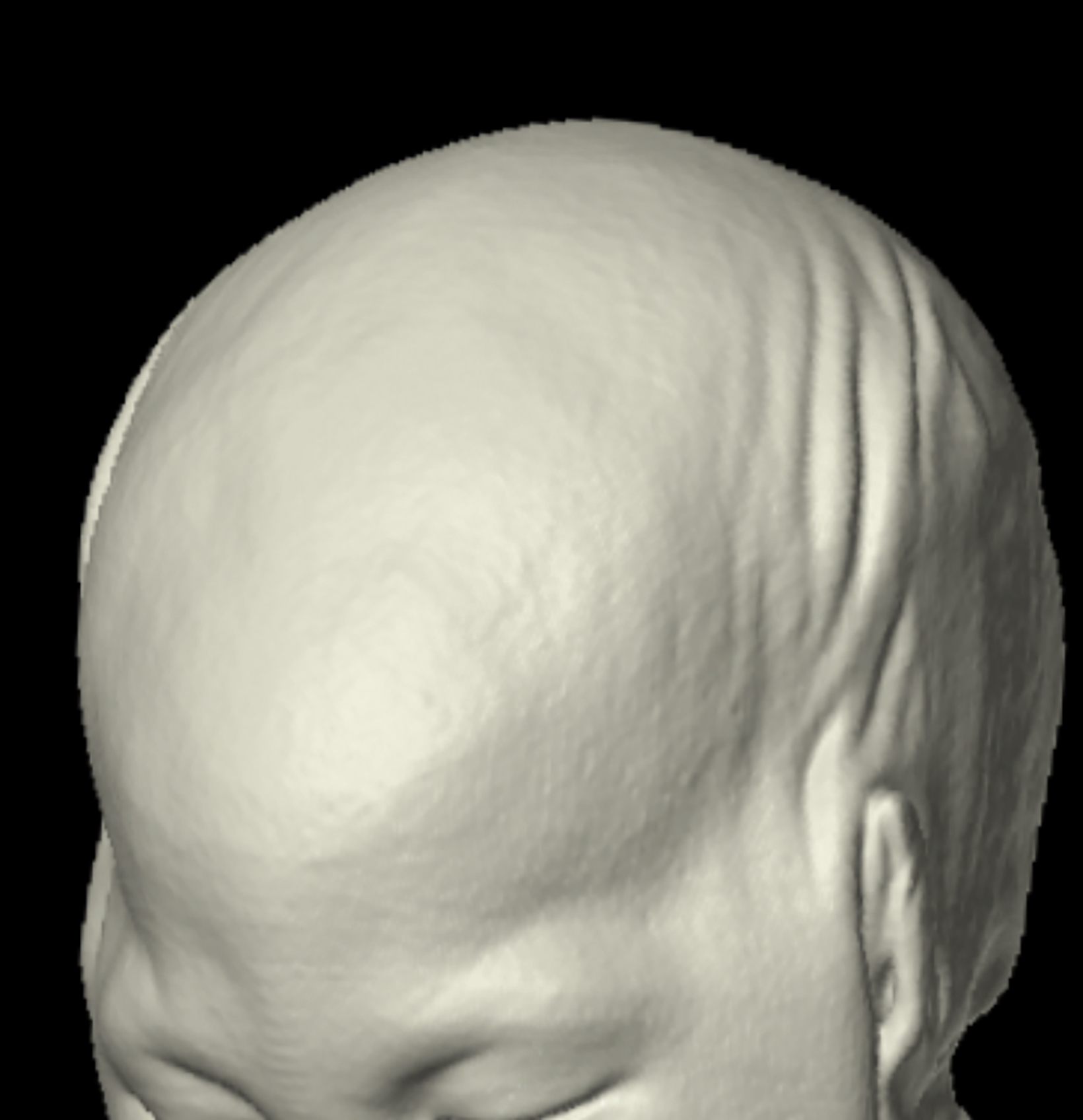
A 3D-reconstructed noncontrast head computed tomography scan (Figure 1) showed premature fusion of the metopic suture with a trigonocephalic configuration of the skull and bony ridging in the midline of the frontal bone, the site of the fused suture.
Diagnosis
Metopic suture synostosis
Discussion
Metopic suture craniosynostosis is the premature fusion of the metopic suture, which normally separates the two frontal bones at birth. Typically, the metopic suture does not begin to fuse until 3 months of age and completely closes by 6-9 months.2 In metopic craniosynostosis, the premature fusion leads to restricted lateral growth of the frontal bones, causing a prow-shaped deformity of the frontal bone, trigonocephaly, and a normal-to-small volume of the anterior cranial fossa.3
The general incidence of craniosynostoses is 6 per 10,000 live births, with approximately 85% of cases being nonsyndromic craniosynostoses.4 Metopic synostosis accounts for about 40% of single-suture synostoses. In recent years, metopic synostosis has become the second-most common form of craniosynostosis after sagittal synostosis, although the reason for its increasing prevalence remains unknown.5 The estimated incidence of metopic synostosis is 1 per 5000 to 15,000 live births.6
As in our patient, metopic synostosis can be differentiated from other craniosynostoses by observing and palpating a fused metopic suture with a triangle-shaped, or trigonocephalic, skull configuration.5 In some instances metopic synostosis may be associated with genetic conditions, such as Jacobsen syndrome.3,4 This syndrome is caused by deletion of genes on chromosome 11. There is a spectrum of presenting signs and symptoms including; developmental delay of speech and motor skills, cognitive impairment, a bleeding disorder and facial dysmorphism with hypertelorism, ptosis, epicanthal folds, broad nasal bridge, small mandible and thin upper lip and downturned corners of the mouth.
One of the main concerns with metopic synostosis, as well as other craniosynostoses, is increased intracranial pressure (ICP). As many as 33% of patients with metopic synostosis may have elevated ICP, which can lead to abnormalities in neurological development if untreated.4
Although the exact etiology for metopic synostosis remains unknown, its cause is thought to be multifactorial. Diagnosis is often made clinically due to the notable midline ridge, trigonocephaly, and hypotelorism.3,4 Other features of metopic synostosis may include anterior displacement of the coronal sutures, widened posterior parietal regions, pterional constriction, and retrusion of the orbits with flattening of the supraorbital ridges and lateral orbital hypoplasia.3
Imaging, specifically CT with 3D reconstruction of the skull, can assist in identifying these bony deformities as well as in planning for surgical intervention.5 3D CT may be able to distinguish true metopic synostosis from a “benign” or physiologic metopic ridge.7,8 Specifically, if the initial physical exam does not distinguish between the two diagnoses, 3D analysis can measure the curvature from different regions (mid-forehead, lateral orbitals, etc.) of the formed ridge. These curvature measurements may then be compared to values that are typical for a ridge found in true metopic synostosis versus a benign ridge.7,8
Treatment depends on the severity of the metopic synostosis and cosmetic deformity. Mild trigonocephaly with a small metopic ridge may be managed without surgical intervention. For moderate-to-severe trigonocephaly, surgical intervention may be considered.9 Severity can be determined on CT by the degree of angulation between the frontal bones, known as the interfrontal angle. Generally, a smaller interfrontal angle suggests a more severe case of metopic synostosis. Although there is currently no gold standard for determining when surgical intervention is needed, Anolik, et al, suggest that an interfrontal angle of less than 118 degrees is a suitable threshold for surgical intervention.10 Surgical options include open cranial vault reconstruction via fronto-orbital advancement or a minimally invasive endoscopic strip craniectomy followed by helmet therapy. The latter is optimal for patients younger than 3 to 4 months, while the former is usually performed in older children.9
Conclusion
Metopic suture synostosis is a rare condition that has been increasing in incidence and can be reliably diagnosed with 3D head CT. The trigonocephaly resulting from premature midline fusion of the metopic suture can lead to increased intracranial pressure. Decisions regarding surgical options consider the severity of the trigonocephaly and age of the patient at presentation.
References
- Head Circumference for age. 2021; Available from: https://www.who.int/tools/child-growth-standards/standards/head-circumference-for-age
- Vu HL, Panchal J, Parker EE, Levine NS, Francel P. The timing of physiologic closure of the metopic suture: a review of 159 patients using reconstructed 3D CT scans of the craniofacial region. J Craniofac Surg. 2001 Nov;12(6):527-32. doi: 10.1097/00001665-200111000-00005.
- Van der Meulen J. Metopic synostosis. Childs Nerv Syst. 2012;28(9):1359-1367. doi:10.1007/s00381-012-1803-z
- Fernández-de Thomas RJ, De Jesus O. Trigonocephaly. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 7, 2021.
- Dias MS, Samson T, Rizk EB, Governale LS, Richtsmeier JT. Identifying the misshapen head: craniosynostosis and related disorders. Pediatrics. 2020;146(3):e2020015511.
- Cornelissen M, Ottelander Bd, Rizopoulos D, et al. Increase of prevalence of craniosynostosis. J Craniomaxillofac Surg. 2016;44(9):1273-1279. doi:10.1016/j. jcms.2016.07.007
- Cho MJ, Kane AA, Seaward JR, Hallac RR. Metopic “ridge” vs. “craniosynostosis”: quantifying severity with 3D curvature analysis. J Craniomaxillofac Surg. 2016; 44(9):1259-1265. doi:10.1016/j.jcms.2016.06.019.
- Cho MJ, Hallac RR, Effendi M, Seaward JR, Kane AA. Comparison of an unsupervised machine learning algorithm and surgeon diagnosis in the clinical dif- ferentiation of metopic craniosynostosis and benign metopic ridge. Scientific Reports. 2018;8(1), 6312. https://doi.org/10.1038/s41598-018-24756-7.
- Proctor MR, Meara JG. A review of the management of single-suture craniosynostosis, past, present, and future. J Neurosurg Pediatr. 2019;24(6):622-631. doi:10.3171/2019.7.PEDS18585.
- Anolik RA, Allori AC, Pourtaheri N, Rogers GF, Marcus JR. Objective assessment of the interfrontal angle for severity grading and operative decision-making in metopic Synostosis. Plast Reconstr Surg. 2016;137(5):1548-1555. doi:10.1097/PRS.0000000000002052
.
Citation
MR D, RB T, CM S, Y L, AJ T.Metopic Suture Synostosis. Supplement to Applied Radiology. 2022; (6):3-5.
November 2, 2022