Medicaid Patients in States with Higher Reimbursement Are More Likely to Receive Imaging
Images
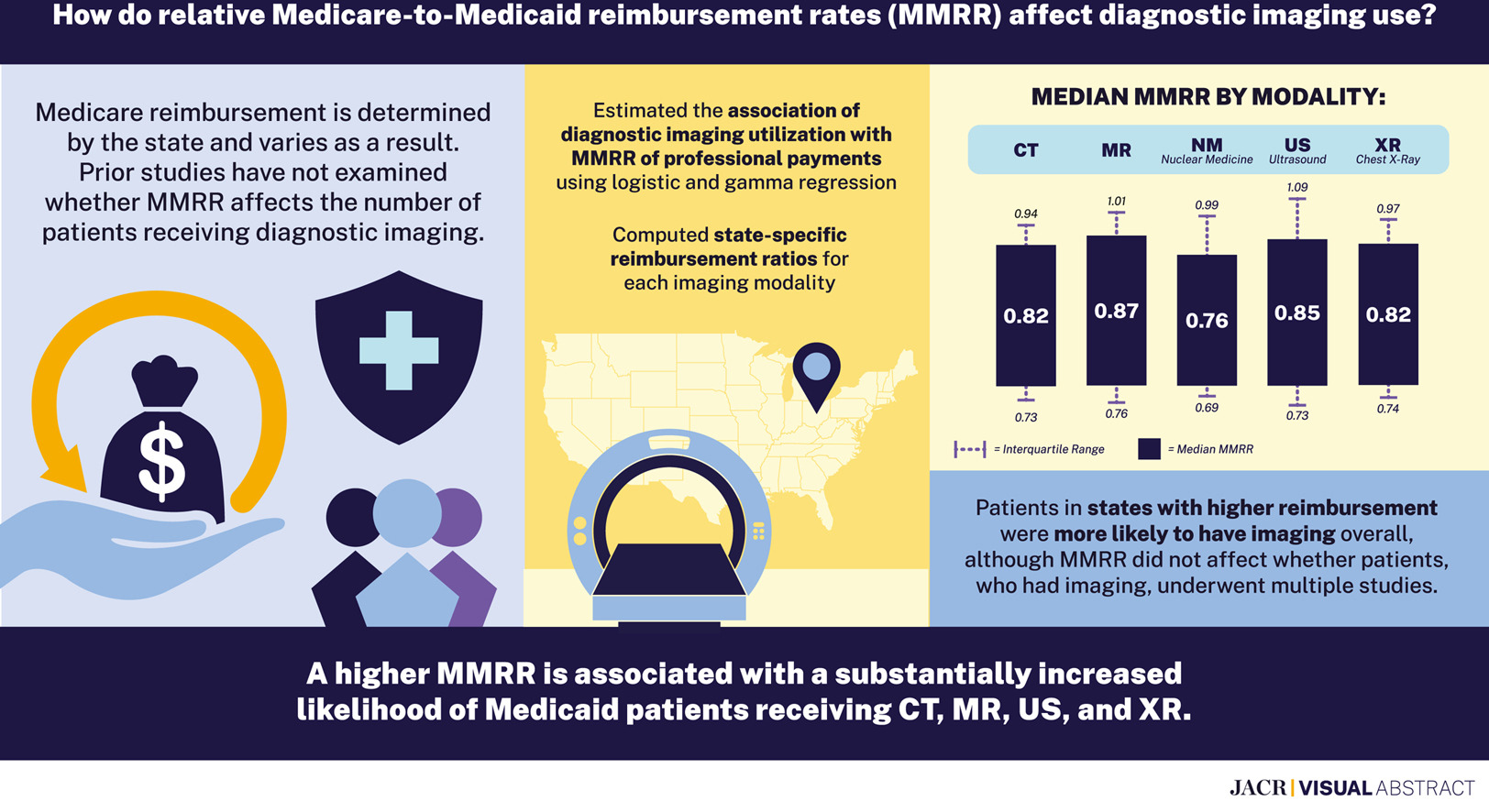
Medicaid patients residing in states with higher Medicaid reimbursement were more likely to receive medical imaging, according to a new Harvey L. Neiman Health Policy Institute study. However, for those who underwent imaging, the number of imaging exams they received did not vary with reimbursement. This study, published in the Journal of the American College of Radiology, was based on nearly 49 million Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries 0-64 years of age in 2019.
As a state-run program, Medicaid reimbursement varies state-to-state. Because the cost of providing care varies across states, simply comparing Medicaid reimbursement from one state to the next would be inappropriate. Because Medicare reimbursement is adjusted to reflect differences in the costs of providing care across locations, the researchers were able to use this information to create the Medicaid-to-Medicare reimbursement ratio (MMRR) to fairly compare Medicaid reimbursement across states.
“The median MMRR ranged from a low of 0.76 for nuclear medicine to a high of 0.87 for CT, meaning that the median Medicaid payment providers receive for imaging ranges from 76% to 87% of what Medicare pays,” said Eric Christensen, PhD, Research Director at the Neiman Health Policy Institute. “Across states there was substantial variation in Medicaid reimbursement compared to Medicare. For example, the median MMRR for X-ray was 0.82, but the bottom 25% of states had a ratio of 0.74 or less. The top 25%, however, had a ratio of 0.97 or more. Hence, differences in Medicaid reimbursement across states are not trivial.”
“Given these differences, we sought to investigate the association between Medicaid reimbursement levels and the utilization of medical imaging by Medicaid beneficiaries,” said Elizabeth Rula, PhD, Executive Director at the Neiman Health Policy Institute. “While utilization is not a direct measure of access, it is reasonable proxy. Providers paid significantly less for providing services to Medicaid patients versus other insured patients, may elect not accept Medicaid insurance. Our finding that states with lower reimbursement systematically have less Medicaid imaging utilization than higher-reimbursement states strongly suggests that reimbursement influences access to care.”
The percentage of patients who receive imaging was lower by approximately 25-28% for CT, MR and ultrasound at the 25th percentile versus 75th percentile of reimbursement as measured by MMRR. The largest difference was for X-ray, with utilization 38% higher at the 75 percentile of reimbursement compared to the 25th. “While our findings are not a direct measure of access to care, it is clear that Medicaid reimbursement is strongly correlated with utilization. The observed disparities show that having Medicaid coverage is not synonymous with equal access to care,” explained Dr Christensen.
“The implication of our study is that increasing state Medicaid reimbursement is a logical option for improving access to care,” said Dr Rula. “As a safety net program, Medicaid serves low-income Americans and a disproportionate percentage of beneficiaries who are Black or Hispanic. Eliminating Medicaid reimbursement gaps may reduce the health care and outcome disparities experienced by these underserved groups.”