Lung Abnormalities Found on Chest CT Two Years After COVID
 A study published in Radiology reports persistent lung abnormalities in patients two years after COVID-19 were detected by chest CT. This is the first research paper with two-year follow-up data on COVID-19 lung effects.
A study published in Radiology reports persistent lung abnormalities in patients two years after COVID-19 were detected by chest CT. This is the first research paper with two-year follow-up data on COVID-19 lung effects.
Globally, more than 600 million people have recovered from COVID-19, but concerns remain that some organs, especially the lungs, may suffer long-term damage after infection.
Qing Ye, MD, and Heshui Shi, MD, PhD, from Tongji Medical College of Huazhong University of Science and Technology in Wuhan, China, and colleagues set out to assess residual lung abnormalities in patients up to two years post-COVID-19 pneumonia. They also looked at the correlation between residual lung abnormalities and changes in lung function.
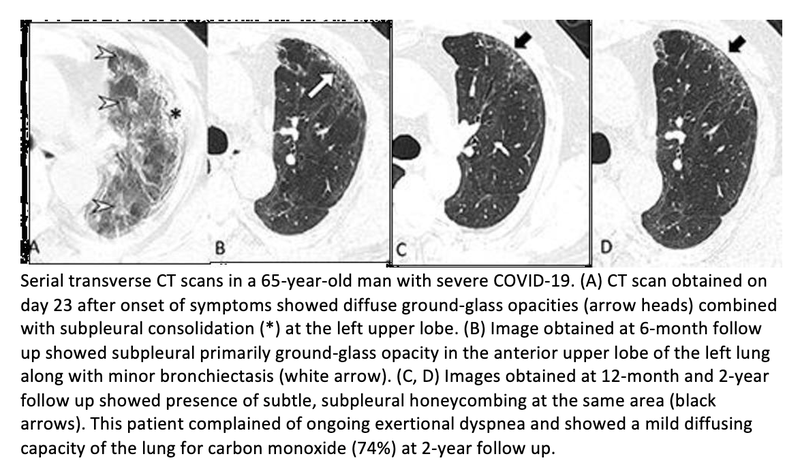
In this prospective study, 144 patients (79 men and 65 women, median age 60) discharged from the hospital after SARSCoV-2 infection between January 15 and March 10, 2020, were included. Three serial chest CT scans and pulmonary function tests were obtained at six months, 12 months and two years after symptom onset.
Residual lung abnormalities after discharge from the hospital included fibrosis (scarring), thickening, honeycombing, cystic changes, dilation of the bronchi, and more.
Over two years, the incidence of lung abnormalities gradually decreased. At six months, 54% of patients showed lung abnormalities. On two-year follow-up CT scans, 39% (56/144) of the patients had lung abnormalities, including 23% (33/144) with fibrotic lung abnormalities and 16% (23/144) with non-fibrotic lung abnormalities.
"In particular, the proportion of fibrotic interstitial lung abnormalities, an important precursor to idiopathic pulmonary fibrosis, remained stable throughout follow-up," the authors said. "Therefore, the fibrotic abnormalities observed in our study might represent a stable, irreversible pulmonary condition, such as lung fibrosis, after COVID-19."
The remaining 88 cases (61%) showed no abnormalities.
Patients with lung abnormalities on CT were more likely to have respiratory symptoms and abnormal lung function. The proportion of individuals with respiratory symptoms decreased from 30% at six months to 22% at two years.
At two-year follow-up, the most common respiratory symptom was exertional dyspnea or shortness of breath (14% [20/144]), while mild and moderate pulmonary diffusion—which refers to how well the air sacs in the lungs are delivering oxygen to and removing carbon dioxide from the blood in the tiny blood vessels that surround them—were observed in 29%(38/129) of patients. Pulmonary diffusion was regarded as abnormal when diffusing capacity of the lung for carbon monoxide was less than 75% of the predicted value. The researchers suggest that persisting residual symptoms and abnormal lung function could be related to the patient's ongoing lung damage.
"Long-term and functional consequences of chest CT findings post-COVID-19 are largely unknown," the authors said. "Our prospective study found that 39% of participants had persistent interstitial lung abnormalities at two-year follow-up, which were associated with respiratory symptoms and decreased diffusion function."
The authors advise that patients with residual lung abnormalities or respiratory symptoms after COVID-19 should be followed up to detect and manage pulmonary changes and functional impairment.
Related Articles
Citation
Lung Abnormalities Found on Chest CT Two Years After COVID. Appl Radiol.
February 14, 2023