Luc Abscess
Case Summary
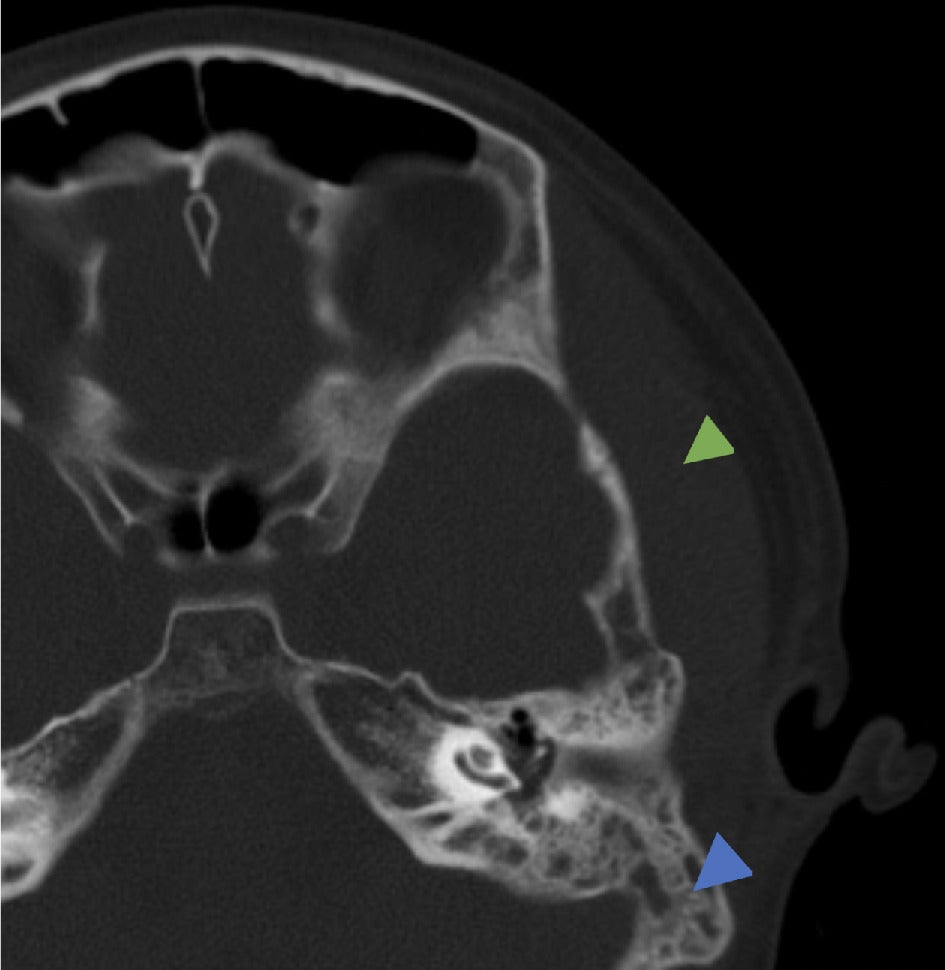
A previously healthy child presented to our institution after CT examination at another institution revealed mastoid air cell effusion and swelling of the left temporal soft tissues ( Figure 1 ). Symptoms included headache, focal pain, and swelling over the left temporal region and decreased left auditory clarity. Physical examination demonstrated left tympanic membrane opacification, suggesting infection, and left temporal swelling anterior and superior to the left ear without edema or tenderness to palpation over the mastoid portion of the temporal bone.
Temporal bone CT. Axial bone window demonstrating mastoid effusion (blue arrowhead) and abnormally thickened left temporal region soft tissues (green arrowhead).
Laboratory findings included elevated C-reactive protein (6.1 mg/dL), red blood cell sedimentation rate (77 mm/hour), and white blood cell count. Intravenous antibiotics were administered. Ultrasound of the left temporal soft tissues was performed, followed by MRI.
Imaging Findings
Ultrasound of the region of concern demonstrated asymmetric thickening of the temporalis musculature measuring approximately 10.9 mm in thickness on the left versus 5.4 mm on the right. Loss of echotexture suggested edema. A small irregular hypoechoic area measuring approximately 9 × 2 × 11 mm was visible.
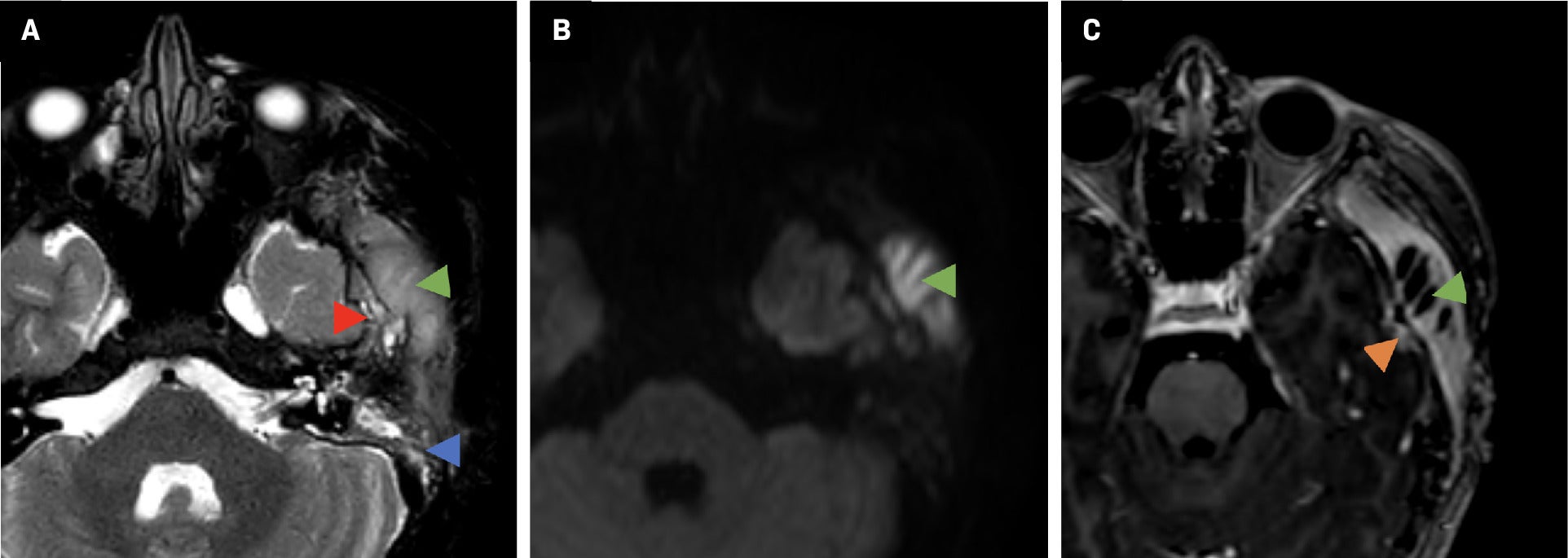
MRI ( Figure 2 ) demonstrated left temporal scalp diffusion-restricting collection with a thick enhancing peripheral rim and abnormal signal within the left squamous and temporal bones, expansion of the bone, irregularity of the cortex and intracranial extension, minimally involving the dura; left mastoid effusion; and edema and enhancement within the left medial pterygoid muscle, left masseter muscle, left mandibular condyle, and left temporomandibular joint place (not shown).
Brain MRI. Axial T2 (A) demonstrates mastoid effusion (blue arrowhead), hyperintense thickened left temporal region soft tissues (green arrowhead), and irregularity of the greater wing of the left sphenoid and squamous temporal bone (red arrowhead). (B) Diffusion-weighted imaging demonstrates left temporal scalp collection with increased signal (green arrowhead) and decreased ADC (apparent diffusion coefficient) (not shown) indicating restricted diffusion in the abscess. (C) Postcontrast T1 demonstrates left temporal scalp fluid collection consistent with abscess (green arrowhead) and a small focus of pachymeningeal enhancement along the temporal lobe surface (orange arrowhead).
Diagnosis
Luc abscess
Discussion
Luc abscess is a rare but dangerous complication of acute otitis media, caused by the spread of infection from the middle ear and creating a subperiosteal suppurative collection beneath the temporal muscle.1 The condition more frequently affects children (80.9%) as a complication of acute otitis media, but also in the setting of congenital cholesteatoma.2 The most common presenting signs and symptoms are preauricular and facial swelling with ipsilateral otalgia, tenderness on preauricular palpation, fever, malaise, trismus, and acute otitis media on otoscopy.3
Named for Henri Luc, the condition was first described in 1913 as Luc sought to identify the abscess as distinct from other subperiosteal abscesses related to acute otitis media and did not involve the mastoid bone. He argued that the infection spread via the notch of Rivinus as well as along branches of the deep auricular artery, which were the proposed pathways connecting the external ear canal to the subperiosteal area deep to the temporalis muscle.1 In an era predating the widespread availability of antibiotics, Luc hoped to reduce unnecessary mastoidectomies, especially in the absence of mastoiditis signs such as ongoing otorrhea and retroauricular swelling.4
Luc’s theory has since been debated; as multiple cases have been reported of patients with subperiosteal abscesses below the temporal bone with concomitant mastoiditis, as seen in our case. In one study, 18 of 19 patients with a subperiosteal temporal abscess also had signs of acute mastoiditis on CT.3 This suggests the presence of an alternative pathway of direct extension from the mastoid air cells to the subperiosteal temporal space. Of note, tenderness of the mastoid and displacement of the pinna often develop days after the onset of preauricular swelling.3 Therefore, concurrent mastoiditis may develop secondary to the subperiosteal temporal abscess.
Contrast-enhanced CT is the preferred initial modality for assessment, including for additional complications such as adjacent venous sinus thrombosis, as well as to rule out other causes of facial edema such as orbital complications of sinusitis.4, 5 MRI can assess for sigmoid sinus thrombosis and other intracranial complications, though it may not be readily available in emergency settings and may require sedation in children.
The preferred treatment for Luc abscess includes incision and drainage with myringotomy and mastoidectomy. However, some believe conservative surgical management with incision and drainage of the subperiosteal temporal abscess is sufficient, even in patients with concurrent mastoiditis.3 Our case was successfully managed with incision and drainage of the abscess. However, mastoidectomy should be considered in patients with acute suppurative mastoiditis or those nonresponsive to antibiotics and drainage alone.
Conclusion
Luc abscess is a rare complication of acute otitis media, caused by the spread of infection from the middle ear to the subperiosteal area deep to the temporal muscle. Although the condition is uncommon with the widespread use of antibiotics for acute otitis media, diagnosing and treating Luc abscess promptly is critical to prevent complications. Radiological studies can assess for the presence of concomitant mastoiditis or intracranial complications as these may alter the treatment plan.
References
Citation
KA S, C A, Kuwabara.Luc Abscess. Appl Radiol. 2025; (2):45-46.
doi:10.37549/AR-D-00072
April 1, 2025