Intra-Abdominal Rupture of a Uterine Leiomyoma
Affiliations
- 1 Trinity Health Oakland Hospital/Wayne State University School of Medicine, Pontiac, Michigan
- 2 Ross University School of Medicine, Miramar, Florida
- 3 Huron Valley Radiology, Ypsilanti, Michigan
Case Summary
A middle-aged G1P1 female presented to the emergency department with a 2-week history of worsening intermittent abdominal pain and constipation. Pelvic US showed an enlarged uterus with calcified fibroids. Cross-sectional imaging was performed and revealed findings suspicious for superinfection with a necrotic fibroid. Further evaluation with MRI and gynecology consultation was recommended; however, the patient declined administration of intravenous gadolinium-based contrast. She was given antibiotics for a potentially infected necrotic fibroid and was discharged with an outpatient referral to gynecology.
She returned to the emergency department one month after her initial presentation with severe, 10/10 pelvic pain, nausea, vomiting, and diaphoresis. A CT of the abdomen and pelvis with intravenous contrast performed at this time noted the necrotic fibroid had ruptured, resulting in complex ascites. The patient was taken to the operating room for a hysterectomy.
Imaging Findings
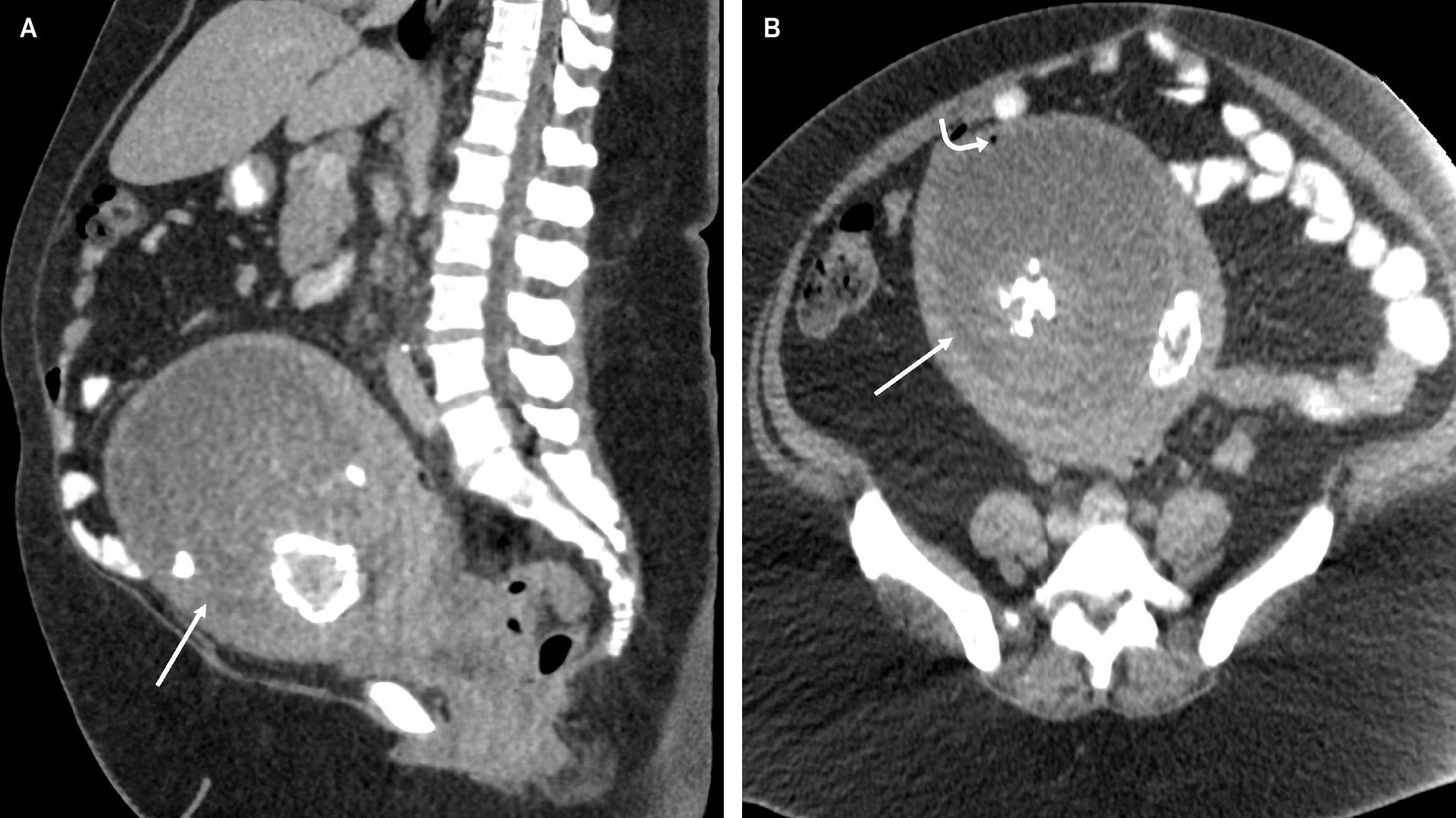
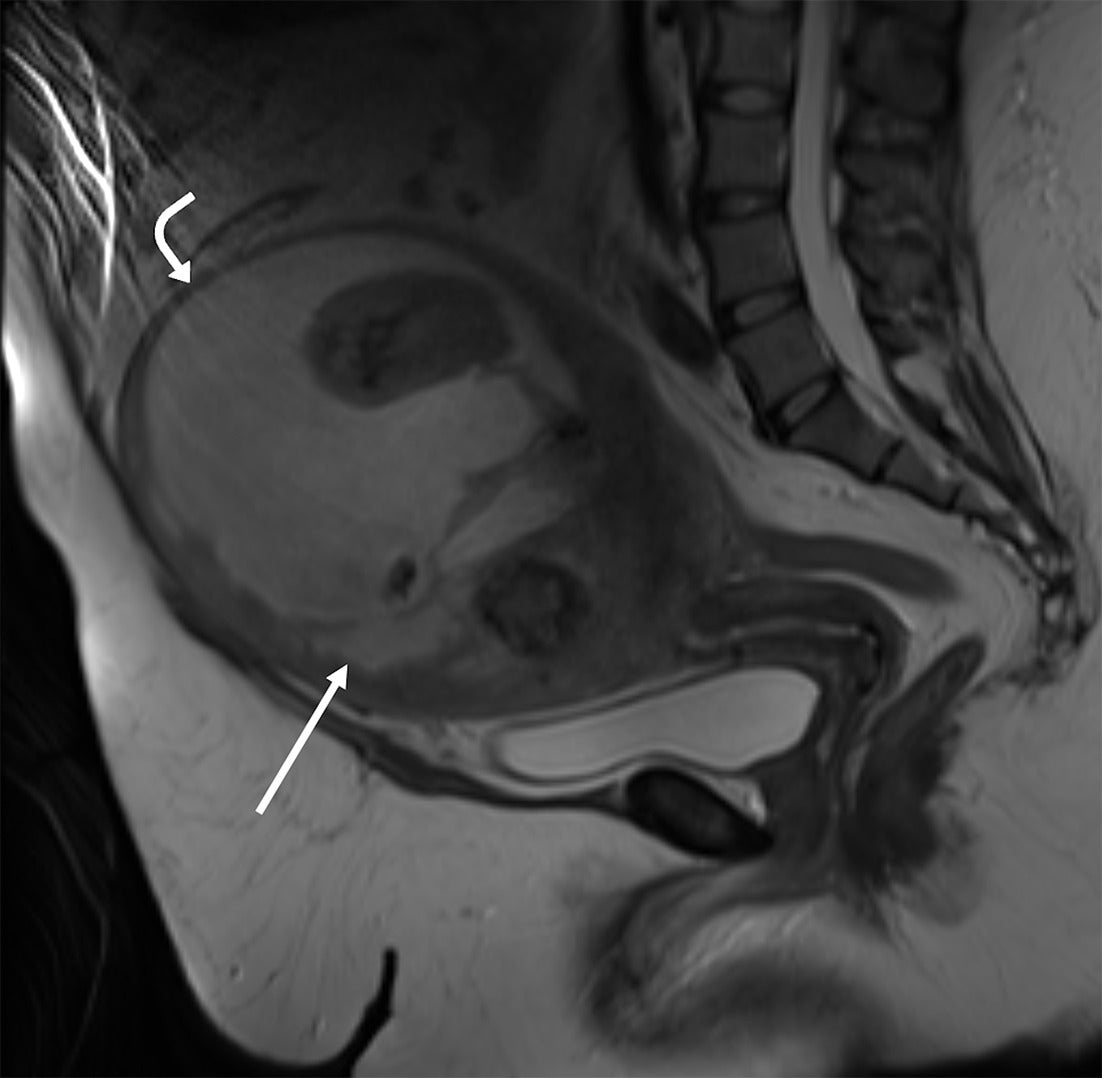
Abdominopelvic CT with intravenous contrast performed upon initial presentation showed a lobular enlarged uterus with a centrally necrotic, partially calcified intramural uterine fibroid at the uterine fundus, which contained a small locule of gas along the anterior myometrial mantle ( Figure 1 ). A subsequent MRI of the pelvis was performed without intravenous contrast and demonstrated similar findings ( Figure 2 ).
Sagittal (A) and axial (B) CT of the abdomen and pelvis after the administration of intravenous contrast shows an enlarged uterus with a centrally necrotic and partially calcified myometrial mass (straight arrow). There is a single locule of air within the necrotic portion of the fibroid anteriorly (curved arrow).
Sagittal T2-weighted MRI of the pelvis without intravenous contrast shows an enlarged uterus with a large, heterogeneous necrotic myometrial mass with cystic, solid, and calcified components (straight arrow). The small locule of gas visualized on the CT was not visualized at the time of MRI. There is marked myometrial thinning along the anterior and superior margins of the necrotic mass (curved arrow).
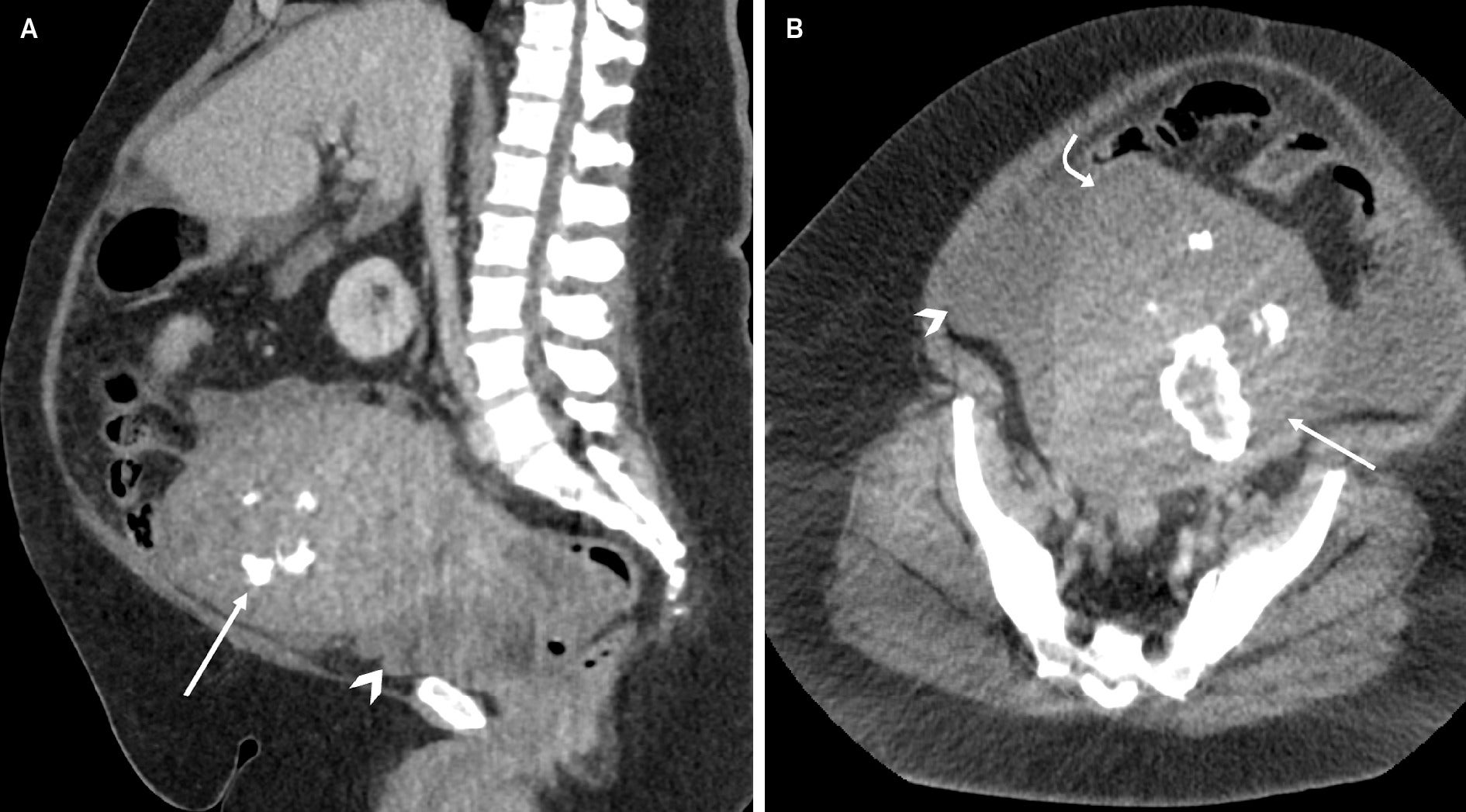
Upon re-presentation to the emergency department approximately one month later, abdominopelvic CT with intravenous contrast showed a small to moderate volume of complex free fluid in the abdomen and pelvis, suspicious for hemoperitoneum ( Figure 3 ). This was suspected to be secondary to a perforated uterine fibroid, given a significant decrease in size and slight change in morphology of the known large necrotic uterine fibroid. Further CT angiographic imaging was performed and noted moderate volume hemoperitoneum without active extravasation.
Sagittal (A) and axial (B) CT of the abdomen and pelvis after the administration of intravenous contrast, obtained one month after initial presentation, shows a significant decrease in size of the cystic component of the previously visualized large necrotic myometrial mass (straight arrow) with a small to moderate volume complex free fluid (arrowhead). Note the abnormal contour (curved arrow) along the right uterine fundus, suspicious for perforation.
Diagnosis
Intra-abdominal rupture of a uterine fibroid. The differential diagnosis included pyomyoma, pyometra, uterine leiomyosarcoma, and uterine sarcoma.
Discussion
Uterine fibroids, or leiomyomas, are the most common benign uterine neoplasm in women and are primarily composed of smooth muscle and fibrous connective tissue. Leiomyomas can be classified as submucosal, intramural, or subserosal depending on location.1 Most leiomyomas are asymptomatic but may present with abnormal uterine bleeding, pain from pressure on abdominal organs, or a palpable abdominal mass.1 Although benign, there are several complications of fibroids that may necessitate intervention. Intra-abdominal hemorrhage due to a ruptured uterine fibroid is extremely rare. Only 125 cases were identified in a 2020 systematic review of the literature for the past century.2 An intraperitoneal hemorrhage from a fibroid is typically secondary to rupture of superficial veins due to an increase in abdominal pressure.3 The resulting bleeding can less frequently be arterial in nature or related to hypertension.3 Other etiologies for intra-abdominal hemorrhage from a fibroid include avulsion due to trauma, torsion of a pedunculated fibroid, and vessel rupture due to venous congestion in menstruation, pregnancy, or strenuous exercise.3, 4
The spontaneous rupture of a fibroid is exceedingly rare, with only ten cases reported in the last half-decade.3 Cases of spontaneous perforation most commonly involve a pathologic provoking factor, such as necrosis or infection, as in our case. Other possible provoking factors include post-dilation and curettage and increased intra-abdominal pressure.5 The bisected gross uterine specimen in our case exhibited uterine fibroids with areas of degeneration and necrosis. Microscopic examination of the surgical specimen from our patient demonstrated hyaline degeneration and ischemic necrosis of the leiomyoma. Hyaline degeneration occurs when smooth muscle is replaced by fibrous connective tissue, resulting in decreased stromal support and tissue integrity.5 This compromised tissue integrity, along with the noted necrotic tissue, could have precipitated a rupture from within the mass. The pathogenesis resulting in the degeneration of fibroids is multifactorial. An enlarging leiomyoma may outgrow its blood supply, resulting in several types of degeneration, including hyaline, calcified, cystic, and red.1 The pathogenesis may also involve steroid hormones.3 Fibroids are responsive to estrogen and progesterone, with symptomatic fibroids being most common in perimenopausal women aged 40 or older.6 Menstrual cyclicity is another important factor affecting the maintenance and growth of fibroids.3 As our patient was perimenopausal, the pathological changes seen in her fibroid might have been related to decreasing levels of estrogen and progesterone and associated with menstrual cycle irregularity. These hormonal changes could have affected the vascular blood supply to her large fibroid, leading to degeneration and necrosis.
US, CT scans, and MRI have been used for the evaluation of ruptured leiomyomas.3 In our case, the CT scan was sufficient to identify the etiology of the small-volume hemoperitoneum, given the absence of the necrotic fibroid visualized on the previous CT. Pelvic US is safe and readily accessible, but the acuity of presentation led to prioritizing CT for a more derivative diagnosis in this scenario. One limitation of the US is the inability to assess for active bleeding and limitations in evaluating adjacent structures. CT angiography was performed to exclude active bleeding in our patient due to the presence of complex ascites. MRI can further delineate the nature of the diagnosis, but it is not appropriate in emergent cases due to acquisition time.4 Only 2 of the 125 patients identified by Lim et al. had an MRI performed.2
Conclusion
Spontaneous rupture of uterine fibroids resulting in hemoperitoneum is a rare complication, as most fibroids will necrose and extrude into the endometrial cavity, rather than rupture into the abdomen. Although acute intra-abdominal bleeding from a ruptured fibroid is rare, it should be included on the differential in any woman with acute hemoperitoneum and a history of fibroids. Prompt surgical intervention based on accurate and timely diagnosis can be life-saving in such circumstances.
References
Citation
Zaki-Metias KM, Vindischman T, MMS LD, Medvedev S, Lu Y, Allen LS.Intra-Abdominal Rupture of a Uterine Leiomyoma. Appl Radiol. 2025;
doi:10.37549/AR-D-25-0106
November 1, 2025