Inflammatory Breast Cancer
Case Summary
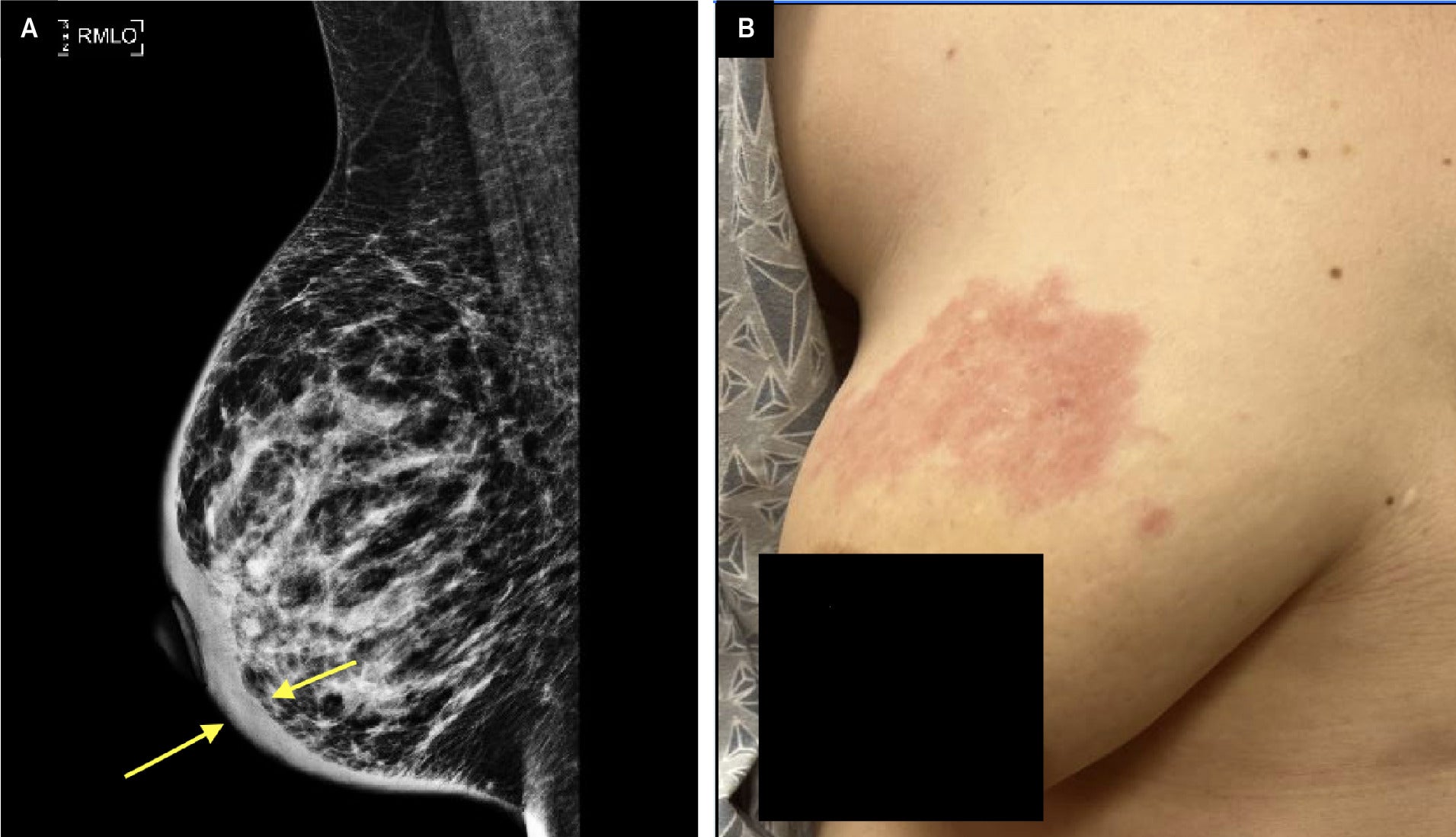
An adult with a past medical history of diabetes presented to the clinic for a 6-week postpartum visit with the chief complaint of a right breast rash. The rash first appeared during her pregnancy and was attributed to atopic dermatitis. She denied pain, fevers, or chills but reported occasional pruritus. The rash worsened despite the use of topical triamcinolone cream ( Figure 1B ). The initial physical exam demonstrated a localized erythematous rash on the right upper outer quadrant without palpable breast or axillary masses. On exam, the left breast was unremarkable. The patient reported no known family history of breast or ovarian cancer.
Mediolateral oblique view mammogram. Diffuse thickening of the dermis (yellow arrows) with trabecular coarsening and thickening in the right breast is seen (A). No masses are visible. Clinical photograph (B) shows a worsening right breast lesion after 1 month of topical triamcinolone.
Imaging Findings
Mammography revealed diffuse dermal thickening of the entire right breast with underlying trabecular coarsening and thickening without definitive masses ( Figure 1A ).
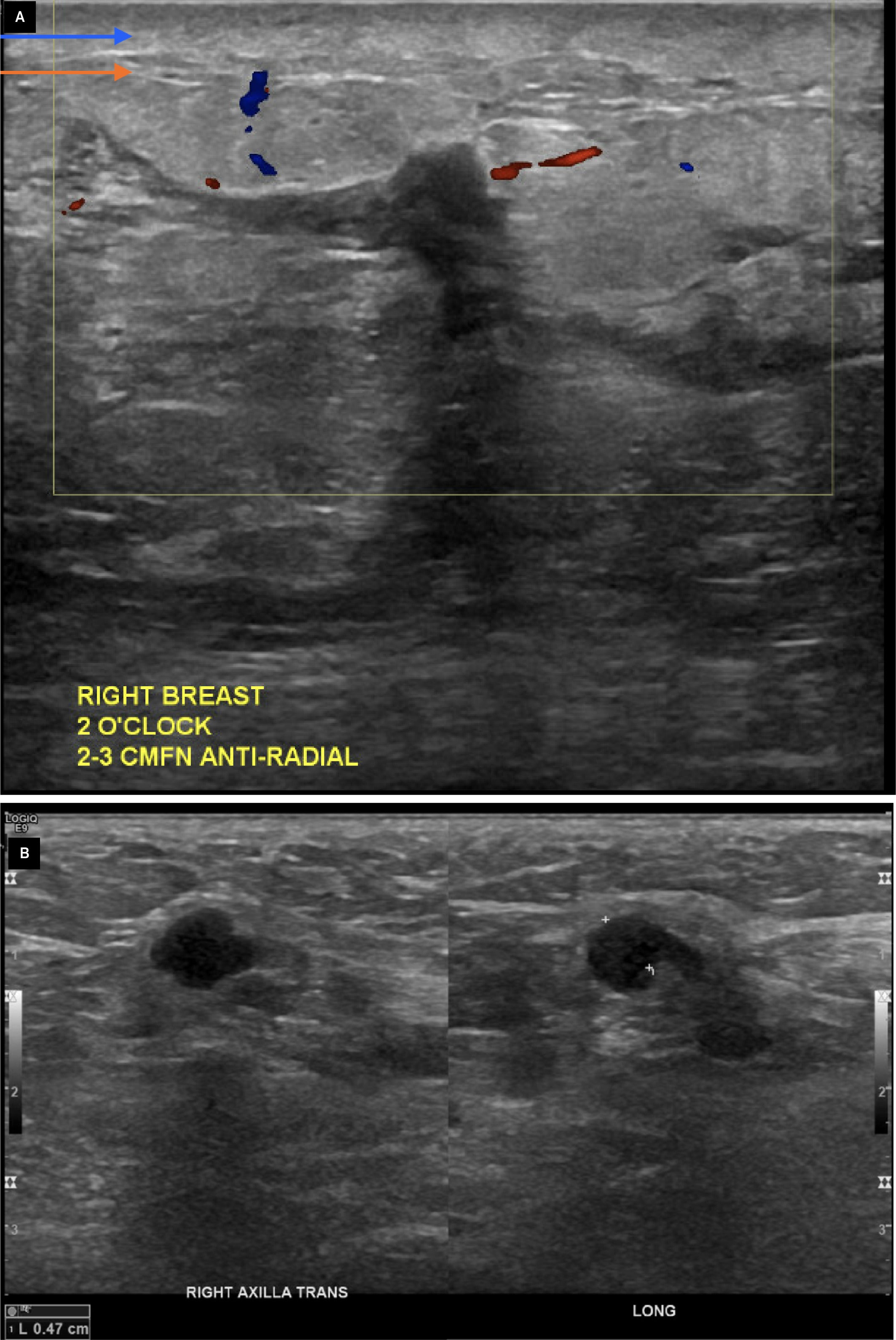
Ultrasound of the right breast revealed marked edema beneath the dermis in nearly every quadrant and below the areola. Additionally, there was an infiltrating appearance of hypoechoic, irregular areas, most prominently seen at 2 o’clock and 6 o’clock positions ( Figure 2A ). Ultrasound of the axilla revealed a mildly prominent lymph node with an eccentrically thickened cortex ( Figure 2B ).
Ultrasound of the right breast imaging shows dermal thickening (blue arrow) with underlying edema (orange arrow), as well as ill-defined hypoechoic collections without discernible Doppler flow (yellow box) at the 2 o’clock position (A). Ultrasound of the right axilla (B) shows a lymph node with an eccentrically thickened cortex (white markers) measuring 0.47 cm and a diminutive fatty hilum.
A punch biopsy was recommended secondary to the skin thickening, which depicted dermal involvement of invasive ductal carcinoma in the superficial and deep dermis, with possible vascular permeation. MRI showed multifocal, suspicious masses and areas of enhancement involving all four quadrants, and the nipple of the right breast was suspicious for multicentric right breast malignancy ( Figure 3A, B ). The most prominent mass measured 2.8 cm.
Axial post-contrast maximum-intensity projection magnetic resonance image shows the left lactating breast without appreciable enhancement (A). The right breast has innumerable foci of enhancement and areas of mass enhancement, with a dominant mass at the 2 o’clock position. Sagittal post-contrast MRI of the right breast (B) shows dermal thickening (blue arrows) with abnormal non-mass enhancement in multiple quadrants and extending to the nipple (red circles). Centrally located, normal background parenchymal enhancement is seen (green circle).

Diagnosis
Invasive ductal carcinoma with lymphovascular permeation, consistent with inflammatory breast cancer.
Discussion
Inflammatory breast cancer (IBC) is a rare malignancy that imparts a worse prognosis than non-inflammatory, locally advanced breast cancer.1 The incidence of IBC rises with age and the plateaus after age 65. The mean age at diagnosis is estimated to be 55-59 years.2 Inflammatory breast cancer accounts for approximately 2%-4% of all breast cancer diagnoses.3
A diagnosis of IBC must meet the following criteria: presence of invasive carcinoma on pathology, rapid onset of less than 6 months, and erythema occupying at least one-third of the breast with edema, peau d’orange, or warmth.4 After confirmation of invasive breast cancer, a clinicopathologic diagnosis of IBC can be made based on the distinct clinical features.5 Interestingly, the patient in this case presented with a localized, pruritic breast rash.
The differential diagnosis of IBC includes atopic dermatitis, infectious mastitis, and idiopathic granulomatous mastitis. Clinical and radiologic features of benign mastitis commonly overlap with breast malignancies such as IBC.6 While infectious mastitis is more common in younger peripartum women,4 providers must have a high clinical suspicion for IBC to ensure early recognition. There should be a low threshold for biopsy, especially when suspected atopic dermatitis or mastitis fails to respond to corticosteroids or antibiotics. Some patients with IBC (20%-40%) will have distant metastasis at initial presentation, so early recognition is imperative.7
Dermal lymphatic involvement is the pathologic hallmark for IBC, as the clinical characteristics are caused by tumor emboli in the papillary and reticular dermis. Cancer cells block the lymphatics, causing subsequent edema and erythema.7
On mammography, IBC may appear with skin thickening, increased breast density, and trabeculation. Less commonly, multiple masses, pleomorphic calcifications, or architectural distortion may be seen.7 On ultrasound, IBC is more likely to appear as a solid mass, whereas mastitis tends to appear as solid-cystic lesions or collections.6
Inflammatory breast cancer and benign mastitis may exhibit similar morphological features on MRI. These features include skin thickening, edema, and the presence of mass lesions or non-mass-like enhancement. However, enhancement features may allow for differentiation between IBC and benign mastitis. In IBC, the initial enhancement is often greater, with more frequent, subsequent washout. Benign mastitis will likely have a more persistent or plateaued enhancement pattern.6
The overall prognosis of IBC is poor, with a 5-year overall survival rate between 29.9% and 42.5%.3 However, multimodal treatment increases 5- and 10-year survival rates by 55.4% and 37.3%, respectively.8 Treatment includes anthracycline-based neoadjuvant chemotherapy followed by modified radical mastectomy and postmastectomy radiation therapy to the chest wall and draining lymphatics.8 Unfortunately, patients with lower incomes, lack of insurance, and multiple comorbidities are significantly less likely to receive multispecialty therapy, resulting in decreased survival rates.8
Conclusion
Inflammatory breast cancer is a rare and aggressive malignancy that, in the initial stages, may mimic benign conditions such as atopic dermatitis, infectious mastitis, or idiopathic granulomatous mastitis. Patients with IBC tend to be younger than those with other breast cancers; thus, there should be a low threshold for biopsy and imaging in younger women with persistent, suspicious skin changes. Metastatic disease is common at initial presentation, and the overall prognosis of IBC is poor. Early diagnosis is crucial for the highest chance of prolonged survival.
References
Citation
Stiller A, Cocco D, Ferraro C.Inflammatory Breast Cancer. Appl Radiol. 2025; (4):
doi:10.37549/AR-D-25-0093
September 8, 2025