Increased Coronary Plaque Activity Detected With PET/CT Tied to Greater Risk for Myocardial Infarction
 Late-breaking research presented at the European Society of Cardiology found that a non-invasive imaging technique for detecting coronary artery disease activity in patients with myocardial infarction did not predict the primary endpoint of all coronary events but did predict all-cause mortality and cardiac death or non-fatal myocardial infarction.
Late-breaking research presented at the European Society of Cardiology found that a non-invasive imaging technique for detecting coronary artery disease activity in patients with myocardial infarction did not predict the primary endpoint of all coronary events but did predict all-cause mortality and cardiac death or non-fatal myocardial infarction.
PRE18 FFIR was the first multicenter international study to examine prospectively whether non-invasive assessment of coronary atherosclerotic plaque activity predicts recurrent cardiac events in patients with myocardial infarction. Prediction is currently performed with clinical risk scores and assessment of obstructive coronary artery disease, but accuracy is lacking. High-risk coronary artery plaques identified using invasive imaging approaches have been associated with future coronary events, but these techniques are impractical for widespread clinical use.
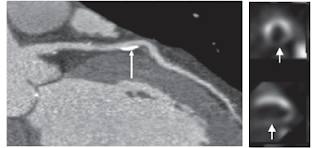
Kwiecinski et al previously found that increased coronary plaque activity (called coronary microcalcification activity; CMA) was associated with a greater risk of myocardial infarction. CMA is a measure of coronary atherosclerotic plaque activity assessed using non-invasive18F-sodium fluoride positron emission tomography (PET) and computed tomography coronary angiography (CTCA). It is based on the finding that coronary artery18F-sodium fluoride uptake is a marker of active calcification in lipid-rich necrotic atheromatous plaques.
The PRE18 FFIR study investigated whether CMA could predict recurrent coronary events in patients with recent myocardial infarction. Between 2015 and 2020, the trial enrolled 704 patients aged 50 years or older with a recent (within 21 days) myocardial infarction and multivessel coronary artery disease on invasive coronary angiography or previous coronary revascularization. The primary endpoint was cardiac death or non-fatal myocardial infarction but was expanded during the study to include unscheduled coronary revascularization due to lower than anticipated primary event rates.
The average age of participants was 64 years and 85% were men. Some 89% had multivessel coronary artery disease, 7% had left main stem disease, and 4% had one-vessel disease. All participants underwent18F-sodium fluoride PET and CTCA, and CMA was determined by an independent blinded core laboratory. CMA=0 indicates low coronary atherosclerotic plaque activity and CMA>0 indicates high coronary atherosclerotic plaque activity. A total of 421 patients had CMA>0 and 283 patients had CMA=0. The two groups had similar mean Global Registry of Acute Coronary Events (GRACE) scores and severity of coronary artery disease.
During a median follow up of four years, the composite primary endpoint of cardiac death, non-fatal myocardial infarction, or unscheduled coronary revascularization occurred in 51 patients (18%) in the CMA=0 group and 90 patients (21%) in the CMA>0 group. Increased coronary atherosclerotic plaque activity was not associated with the primary endpoint
(hazard ratio [HR] 1.25; 95% confidence interval [CI] 0.89–1.76; p=0.20). This was principally due to the lack of an association with unscheduled coronary revascularization (HR 0.98 ; 95% CI 0.64–1.49 ; p=0.91). In secondary analyses, increased coronary atherosclerotic plaque activity was associated with all-cause mortality (HR 2.43; 95% CI 1.15–5.12; p=0.020) and with the original primary endpoint of cardiac death or non-fatal myocardial infarction (HR 1.82; 95% CI 1.07–3.10; p=0.028).
The imaging protocol was associated with 15 adverse events, which were principally venous cannula-related or contrast reactions. Two events were graded as serious: one patient experienced palpitations and one patient had beta-blocker induced bradycardia.
Chief investigator Professor David Newby of the University of Edinburgh, UK said, “Increased coronary atherosclerotic plaque activity is not associated with all coronary events but predicts cardiac death or non-fatal myocardial infarction and all-cause mortality. The association remained after adjusting for the severity of obstructive coronary artery disease or GRACE score. These findings indicate that coronary atherosclerotic plaque activity predicts spontaneous recurrent atherothrombotic events. CMA assessment could guide the application of more intensive lipid-lowering, anti-inflammatory or other advanced therapies to prevent recurrent spontaneous atherothrombotic events.”
Related Articles
Citation
Increased Coronary Plaque Activity Detected With PET/CT Tied to Greater Risk for Myocardial Infarction. Appl Radiol.
August 31, 2022