Incidental Renal Arteriovenous Malformation
Images




CASE SUMMARY
A 61-year-old presented to the emergency department with lightheadedness. Vital signs included blood pressure of 120/76 mmHg, heart rate of 100 bpm, and oxygen saturation of 99% on room air. Physical examination was normal, except for pallor. The patient had a history of hypertension, well controlled on three different categories of antihypertensives. There was also a history of bleeding diathesis, which was attributed to use of nonsteroidal anti-inflammatory drugs (NSAID). Patient’s medical history was unremarkable for trauma, surgery, or instrumentation to the kidneys. Family history did not include bleeding disorders or genetic renal abnormalities.
Laboratory results revealed normocytic anemia with hemoglobin of 70 g/mL, mildly increased serum creatinine of 103 U/L, as well as borderline low serum potassium of 3.5 mmol/L. Further investigation included endoscopy, which revealed a large mass lesion in the cecum, consistent with villous adenoma.
IMAGING FINDINGS
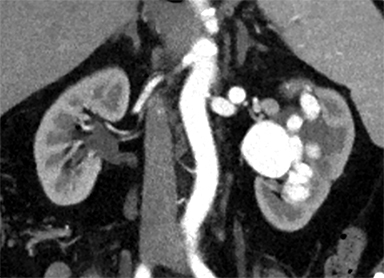
Contrast-enhanced CT of the abdomen and pelvis to evaluate the cecal mass demonstrated an incidental large, left renal arteriovenous malformation (AVM) (Figure 1). Subsequent multiphasic CT examination dedicated to the kidneys (including arterial and venous phases) was conducted with coronal and sagittal reformations (Figure 2). The left main renal artery was significantly enlarged and tortuous, measuring up to 9.6 mm in maximal cross-sectional diameter.
The left kidney was found to have a complex arterial supply, including two arterial branches to the upper pole of the kidney, one arterial branch to the interpolar region, and an accessory renal artery arising from the abdominal aorta and supplying the lower pole.
The renal AVM showed direct communication between the arterial circulation and markedly dilated draining venous structures within the renal sinus as well as multiple venous lobulations with vermiform appearance at the periphery. The left kidney also demonstrated mild hydronephrosis.
DIAGNOSIS
Incidental renal arteriovenous malformation
DISCUSSION
Renal AVMs are abnormal direct communications between intrarenal arterial and venous systems, avoiding flow through the capillary bed. They were first described in 1928 by Varela and are uncommon in the general population, representing approximately 1% of all AVMs.1 Renal AVMs are congenital or acquired in etiology. The term “AVM” more commonly refers to the congenital type of vascular abnormality, whereas acquired malformations are usually referred to as arteriovenous fistulas.2 Although congenital AVMs are more prevalent, their etiology is not well understood. It is thought that they may occur during the first trimester of gestation as a result of focal spontaneous errors in vascular development.3
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu disease, was postulated to be associated with congenital renal AVMs.4,5 A rare, autosomal dominant genetic disorder, HHT is characterized by spontaneous recurrent epistaxis, musculocutaneous and visceral telangiectasias and AVMs, with a strong family predisposition.4,5 A clinically significant proportion of HHT patients have AVMs of the internal viscera. As recently shown, endoglin and activin receptor-like kinase 1 are likely correlated to the pathogenesis of congenital AVM formation.4–6
Acquired AVMs, on the other hand, can be idiopathic or develop as a sequela of trauma, percutaneous renal biopsy, ureteroscopy, previous partial nephrectomy, or renal malignancy.7 In patients with hypertension following penetrating renal injury, AVMs may be found in one-third of cases; conversely, patients with AVMs are reported to have effects on the renin-angiotensin-aldosterone system (RAAS) and to develop hypertension resulting from secondary aldosteronism.1,3
The signs and symptoms of vascular renal lesions vary widely from asymptomatic to hematuria (72%), hypertension (50%), flank pain, abdominal mass, perinephric hematoma, flank bruit, and high-output heart failure.1,6 Renal AVMs are usually found while investigating a patient presenting with gross hematuria; flank pain and hypertension are less common.4
Our patient complained mainly of lightheadedness and reported no hematuria, abdominal pain, or increased blood pressure at examination. However, the patient had a history of hypertension, which may have resulted from renal AVM owing to its impact on the RAAS.1,3 The patient also had a history of bleeding diathesis, which was attributed to NSAID use. The significance of an underlying hematological disorder may potentially be further related to renal AVM formation. The patient had no other signs of renal function impairment, except for slightly elevated creatinine, but was found to have normocytic anemia, which eventually led to the diagnostic endoscopic procedure revealing a colon cancer.
Dedicated kidney arterial- and venous-phase CT is the preferred minimally-invasive imaging technique to identify and classify renal vascular abnormalities.8 Doppler sonography and magnetic resonance angiography are also beneficial tools that reduce the need for radiation exposure and the use of iodine-contrast materials. Renal digital subtracted angiography remains the imaging “gold standard” for diagnosing renal vascular malformations.2,3
The goal of renal AVM treatment is to preserve the renal parenchyma while alleviating symptoms and maintaining hemodynamic stability. Asymptomatic or minimally symptomatic small peripheral AVMs with hemodynamic stability can be managed conservatively. Transcatheter arterial embolization has replaced major surgical intervention as the treatment of choice.8 However, open surgery should be considered in cases related to malignancy and those in which patient anatomy is not favorable to endovascular treatment.8
The goal of embolization therapy is to occlude the abnormal arterial and venous connections while maintaining patency of the mainstem vessels.9 Nephrectomy can be considered in complicated cases.1,8,9 Successful treatment can resolve hematuria and cure or improve hypertension in 60-85% of patients.5,9
CONCLUSION
Although uncommon, renal AVMs should be considered when evaluating patients with hypertension refractory to multiple antihypertensive agents, anemia, bleeding diathesis, abdominal pain, and impaired renal function. Doppler sonography and CT are accessible imaging modalities that help to diagnose AVMs. Given the appropriate clinical context, arterial embolization may be used as a safe and effective treatment.
REFERENCES
- Cura M, Elmerhi F, Suri R, Bugnone A, Dalsaso T. Vascular malformations and arteriovenous fistulas of the kidney. Acta Radiol. 2010;51(2):144-149. doi:10.3109/02841850903463646
- Whitehead KJ, Smith MCP, Li DY. Arteriovenous malformations and other vascular malformation syndromes. Cold Spring Harb Perspect Med. 2013;3(2): a006635-a006635. doi:10.1101/cshperspect.a006635
- King BF, Hattery RR. Case of the day. Ultrasound. Congenital cirsoid renal arteriovenous malformation (AVM) involving the lower pole of the right kidney. RadioGraphics. 1990;10(6):1101-1104. doi:10.1148/radiographics.10.6.2259764
- Messing E, Kessler R, Kavaney PB. Renal arteriovenous fistulas. Urology. 1976;8(2):101-107. doi:10.1016/0090-4295(76)90330-7
- Gandhi SP, Patel K, Pandya V, Raval M. Renal arteriovenous malformation presenting with massive hematuria. Radiol Case Rep. 2015;10(1):1068. doi:10.2484/rcr.v10i1.1068
- Brown JG, Folpe AL, Rao P, et al. Primary vascular tumors and tumor-like lesions of the kidney: a clinicopathologic analysis of 25 cases. Am J Surg Pathol. 2010;34(7):942-949. doi:10.1097/PAS.0b013e3181e4f32a
- McAllister KA, Grogg KM, Johnson DW, et al. Endoglin, a TGF-β binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat Genet. 1994;8(4):345-351. doi:10.1038/ng1294-345
- Hatzidakis A, Rossi M, Mamoulakis C, et al. Management of renal arteriovenous malformations: a pictorial review. Insights Imaging. 2014;5(4):523-530. doi:10.1007/s13244-014-0342-4
- Brown DB, Brandes SB. Radiofrequency ablation of a recanalized renal arteriovenous malformation. J Vasc Interv Radiol. 2005; 16(3):403-406. doi:10.1097/01.RVI.0000147073.24646.31
Citation
O D, N S, D K, A S.Incidental Renal Arteriovenous Malformation. Appl Radiol. 2021; (3):47-49.
May 4, 2021