Imaging focal nodular hyperplasia
Images




The primary purpose of this brief review is to discuss the basic features of typical and atypical focal nodular hyperplasia, and its complications. his article demonstrates the full spectrum of findings and features of focal nodular hyperplasia (FNH) on different diagnostic radiological modalities. During the past few years, technical advances in CT and MR imaging have led to a marked increase in detection and characterization of FNH. MR imaging is an ideal modality to work up lesions in relatively young women with suspected FNH because radiation and iodine-based contrast media are not used in these patients. Focal nodular hyperplasia is benign, with no malignant potential and a very small risk of complications (rupture, hemorrhage); thus, it is usually treated conservatively.
Background on focal nodular hyperplasia
Focal nodular hyperplasia is defined as a nodule composed of benign-appearing hepatocytes occurring in a normal or nearly normal liver. It has a reported prevalence of 0.9% and is the second-most common benign liver tumor after hemangioma. It is more common in young females, with a male-to-female ratio of 1:8.1 Most FNHs (80 %) are solitary, smaller than 5 cm in diameter, and occur near the liver surface.2 They are usually incidental findings at imaging. Distinguishing FNH and other hypervascular liver lesions, such as hepatic adenomas, hepatocellular carcinomas (HCC) and hypervascular metastases is critical, as their management differs considerably.
Most patients are asymptomatic and no treatment is necessary. Some patients may present with abdominal pain or a palpable mass. They typically follow a benign course and on follow-up examination remain stable or the mass decreases in size.3 Contraceptive agents have not been involved in the pathogenesis but they are associated with an increased risk of complications for patients with FNH. In symptomatic females, hemorrhagic foci or infarctions may occur within the FNH; these are aggravated by administration of contraceptive agents. Spontaneous rupture into the peritoneum is a rare complication associated with contraceptive use. FNH may be associated with hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease) and congenital absence of the portal vein.4
Focal nodular hyperplasia is subdivided into 2 types: classic (80%) and non-classic (20%). In classic FNH, all 3 characteristic features, including abnormal nodular architecture, malformed vessels and cholangiolar proliferation are present. In non-classic FNH, 2 of the 3 characteristic features are present; bile duct proliferation is always present.5 The classic and non-classic types contain variable amounts of Kupffer cells.6
Diagnostic imaging of FNH
On imaging studies, morphology, vascularity, appearance and surrounding liver architecture help to distinguish between typical and atypical lesions. They have no clinical significance, but their recognition is necessary to avoid surgery, biopsy and follow-up imaging.7 - 9
Ultrasound
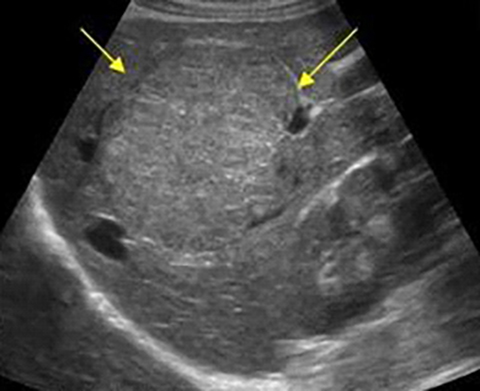
On sonography, the lesion usually appears homogenous, with variable echogenicity, mostly isoechoic, however may be hypo/ hyperechoic. (Figure 1).The center of the lesion shows a scar as an echogenic and linear structure. Lesion shows a characteristic Doppler vascular pattern, including hypervascularity, centrifugal arterial flow radiating peripherally from a central vessel10 as shown in (Figure 2). On real-time contrast-enhanced ultrasound, it shows a typical spoke-wheel pattern followed by complete enhancement in the arterial phase and remains hyper/iso vascular in the portal and late phases. In general, this typical pattern has been observed in 74% to 100% of cases.11
Computed tomography
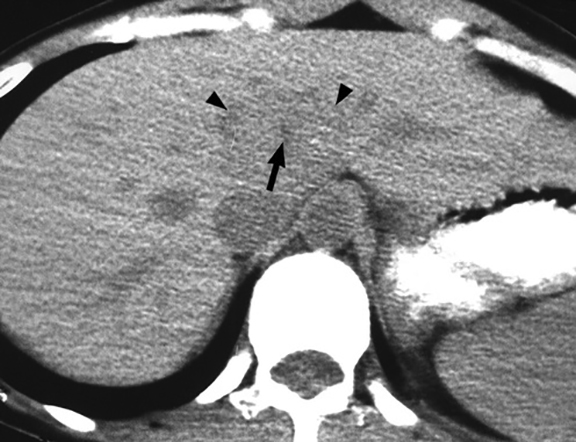
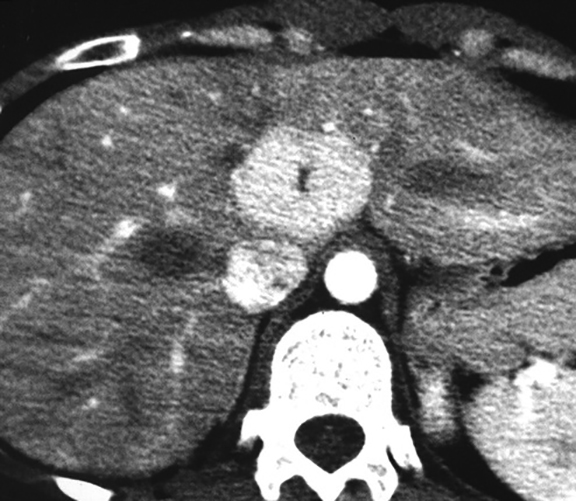
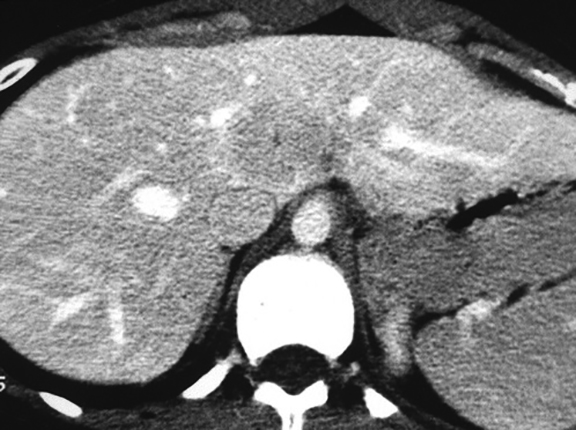
A helical CT scan, 4-phase study should be mandatory for the definitive diagnosis of FNH. This evaluation should include unenhanced, hepatic arterial, portal venous and delayed-phase examinations. At CT, typical FNH may have lobulated contours.7-9 In the unenhanced phase, it is either hypoattenuating or isoattenuating to the surrounding liver. In the arterial phase, due to the homogeneous intense enhancement of the entire lesion, it becomes hyperattenuating except for the central scar. In the portal and later phases, it becomes more isoattenuating; however, the central scar may show some enhancement (Figure 3).
Magnetic resonance imaging
Compared to CT and US, MRI has higher sensitivity (70%) and specificity (98%) for detecting FNH.9 MRI is also more accurate in detecting the central scar than CT, with a sensitivity of 78% and 60%, respectively. The reason for the higher sensitivity and specificity of MRI may be because it not only provides information regarding the soft-tissue characteristics, but also the vascularity of the lesions.
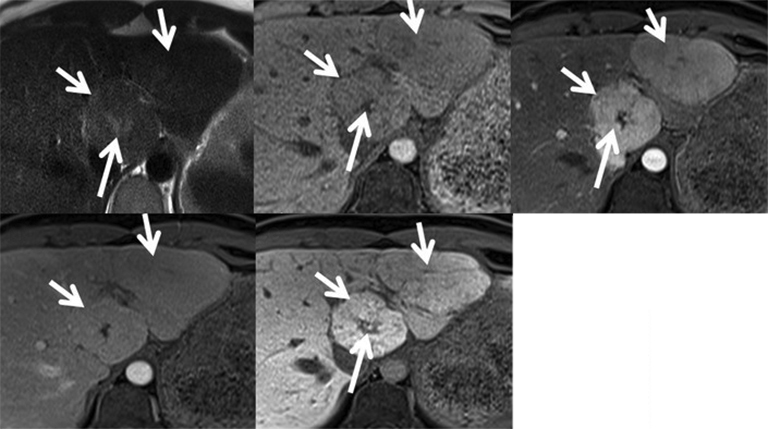
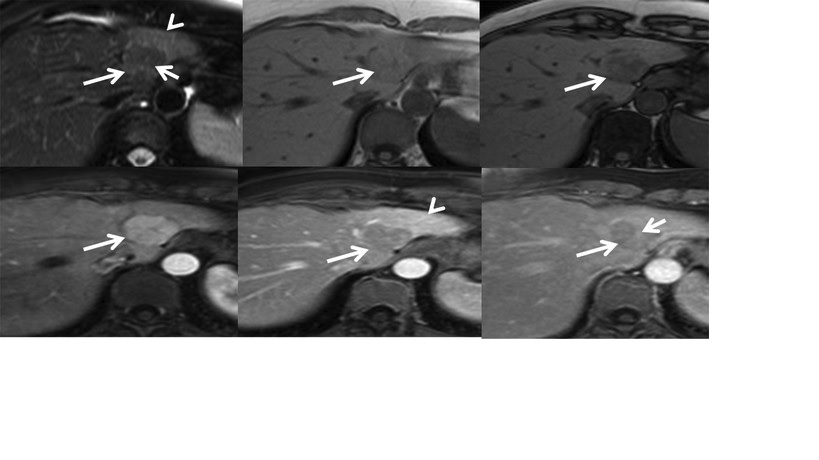
They typically appear homogeneous on MR imaging, with iso- to hypointense signal on T1-weighted images and slightly hyper- to isointense on T2-weighted images. A central hyperintense scar is seen in only 9% to 50% of cases on T2-weighted images.12,13 On contrast-enhanced MRI, it shows intense homogeneous enhancement in the arterial phase and enhancement of the central scar in the later phases (Figure 4). In contrast, hepatocellular adenomas show less intense enhancement and lack a central scar.
Specific super-paramagnetic iron oxide-based (eg, ferucarbotran [Resovist; Schering, Berlin, Germany]) and manganese-based (ie, mangafodipirtrisodium [Tesla-scan; Nycomed Amersham, Oslo, Norway]) contrast media are targeted at the Kupffer cells and hepatocytes, respectively.14- 17 These help to demonstrate the hepatocellular origin of the lesions. The Kupffer cells show uptake of ferucarbotran and lower the signal intensity of the lesions as well as the surrounding liver on T2- and T2∗-weighted images.
A central scar is present at imaging in most patients with FNH.9 The size and amount of scar tissue may vary. The central scar is typically high in signal intensity on T2-weighted images and low on T1-weighted images. It shows visible enhancement on delayed contrast-enhanced images. High signal intensity of the central scar may be caused by the inflammatory reaction around the ductular proliferation as well as the vessels within the septa and central scar. The central scar is not specific for FNH and can be seen in different lesions of the liver, such as giant hemangiomas and hepatocellular carcinomas.
Various atypical features of FNH on MRI have been described, including:18
Appearing heterogeneous on both T1- and T2-weighted sequences due to the presence of small hemorrhagic foci, sinusoidal dilatation or fatty infiltration. High protein concentrations, blood degradation products or copper accumulation may result in T1 hyperintensity.
An extremely small or undetectable scar on CT (16% to 40%) and MRI (22%). The central scar may mimic a collagenous scar seen in fibrolamellar carcinoma, hepatic adenoma, HCC or cholangiocarcinoma due to obliterative vascular hyperplasia of the central scar.
The presence of a pseudo-capsule due to compressed adjacent hepatic parenchyma, and the presence of dilated vessels and sinusoids around the lesion. FNH rarely shows intra-lesional steatosis (Figure 5).
Telangiectatic FNH, an uncommon entity but the most common among non-classic FNHs. These lesions often show heterogeneity on pre- and post-contrast CT and MRI, and they are strongly hyperintense on T1- and T2-weighted images, often with an absent central scar. Intense arterial enhancement with persistent enhancement during the hepatic venous and equilibrium phases are seen.
Multiple lesions, which are found in 20% of cases and are mostly atypical. Multiple FNH syndrome is defined as consisting of two or more FNHs in combination with hepatic liver hemangioma or vascular malformations or intracranial tumors (Figure 6).
Nuclear medicine
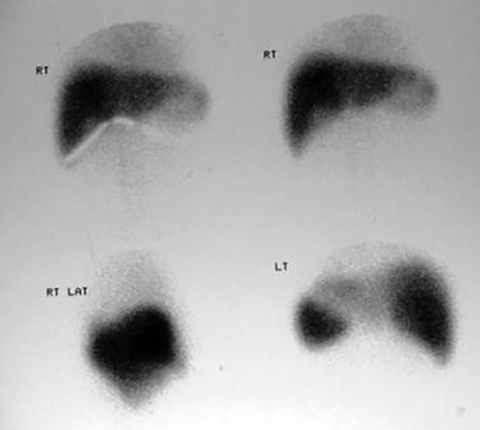
Radionuclide scans best demonstrate Kupffer cell activity. They historically have used technetium-99m (99mTc) sulfur colloid; normal or increased uptake of99mTc sulfur colloid is seen in 60% to 70% of patients (Figure 7). In 30% to 40% of patients, Kupffer cells are not sufficiently concentrated and it may appear photon deficient.19
FNH Management
Focal nodular hyperplasia with typical imaging features is usually managed conservatively and does not require surgical intervention. Symptomatic lesions, likely from compression of adjacent structures or hepatic capsular stretching, may warrant surgical excision. FNH with atypical imaging features requires further evaluation with additional imaging, percutaneous guided biopsy and follow-up. Suspicious lesions could be followed up or surgically excised.20
Conclusion
This article demonstrates the full spectrum of findings and features of focal nodular hyperplasia in different diagnostic imaging modalities. FNH usually presents with classical imaging features, however, atypical features are important for radiologists to recognize and understand. MR imaging is an ideal modality for work-up of atypical lesions.
References
- Vilgrain V. Focal nodular hyperplasia.Eur J Radiol. 2006; 58(2):236–245.
- Mathieu D, Vilgrain V, Mahfouz AE, et al. Benign liver tumors. Magn Reson Imaging Clin N Am. 1997; 5(2):255–288.
- Cherqui D, Rahmouni A, Charlotte F, et al. Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology. 1995; 22(6):1674–1681.
- Rebouissou S, Bioulac-Sage P, Zucman-Rossi J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J Hepatol. 2008; 48(1):163–170.
- Nguyen BN, Fléjou JF, Terris B, et al. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J SurgPathol. 1999; 23(12):1441-1454.
- Hussain SM, van den Bos IC, Dwarkasing RS, et al. Hepatocellular adenoma: findings at state-of-the-art magnetic resonance imaging, ultrasound, computed tomography and pathologic analysis. EurRadiol. 2006; 16(9):1873–1886.
- Shirkhoda A, Farah MC, Bernacki E, et al. Hepatic focal nodular hyperplasia: CT and sonographic spectrum. Abdom Imaging. 1994; 19(1):34-38.
- Carlson SK, Johnson CD, Bender CE, et al. CT of focal nodular hyperplasia of the liver. AJR Am J Roentgenol. 2000; 174(3):705-712.
- Mortelé KJ, Praet M, Van Vlierberghe H, et al. CT and MR imaging findings in focal nodular hyperplasia of the liver: radiologic-pathologic correlation. AJR Am J Roentgenol. 2000; 175(3):687-692.
- Parulekar G, Bree LR. Liver In: Goldberg BB, McGahan GP eds. Diagnostic Ultrasound: Logical Approach. 2nded. New York: Lippincott Williams & Wilkins 2008:367-368.
- Kim MJ et al. Evaluation of hepatic focal nodular hyperplasia with contrast-enhanced gray scale harmonic Sonography: initial experience. J Ultasound Med. 2004;23:297-305.
- Mattison GR, Glazer GM, Quint LE, et al. MR imaging of hepatic focal nodular hyperplasia: characterization and distinction from primary malignant hepatic tumors. AJR Am J Roentgenol. 1987;148(4):711–715.
- Lee MJ, Saini S, Hamm B, et al. Focal nodular hyperplasia of the liver: MR findings in 35 proved cases. AJR Am J Roentgenol. 1991;156(2):317-320.
- Hussain SM, Semelka RC, Mitchell DG. MR imaging of hepatocellular carcinoma.Magn Reson Imaging Clin N Am. 2002; 10(1):31-51.
- Hussain SM, Bijl MS, Zondervan PE, et al. Benign versus malignant hepatic nodules: findings at MR imaging with histopathologic correlation.RadioGraphics. 2002; 22(5):1023-1039.
- Wang YX, Hussain SM, Krestin GP. Superparamagnetic iron oxide contrast agents: physiochemical characteristics and applications in MR imaging. EurRadiol. 2001;11(11):2319-2331.
- Ros PR, Freeny PC, Harms SE, et al. Hepatic MR imaging with ferumoxides: a multicenter clinical trial of safety and efficacy in the detection of focal hepatic lesions. Radiology. 1995;196(2):481-488.
- Ba-Ssalamah A, Schima W, Schmook MT, et al. Atypical focal nodular hyperplasia of the liver: imaging features of nonspecific and liver-specific MR contrast agents. AJR Am J Roentgenol. 2002; 179(6):1447–1456.
- Dähnert W. Disorders of liver, biliary tract and spleen. In: Radiology Review Manual. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007: 714-715.
- Shanbhogue AK, Prasad SR, Takahashi N, et al. Recent advances in cytogenetics and molecular biology of adult hepatocellular tumors: implications for imaging and management. Radiology. 2011;258(3):673–693.
Citation
S I. Imaging focal nodular hyperplasia. Appl Radiol. 2017; (2):26-30.
February 8, 2017