How to Diagnose Intussusception in Children
Images




Abdominal pain is a frequent complaint in the pediatric emergency department. One of the top diagnostic considerations is intussusception, particularly in patients between 3 months and 3 years of age. An intussusception is a loop of bowel telescoping into an adjacent loop of bowel. There are two subtypes of intussusception, ileocolic and small bowel-small bowel. The receiving loop of bowel is called the intussuscipiens and the inner bowel is called the intussusceptum. Both Ileocolic and small bowel-small bowel intussusceptions can occur in children. An ileocolic intussusception is the most common type of intussusception in children and requires urgent treatment. Patients can present with lethargy, vomiting or decreased appetite, with fewer than 50% of patients presenting with the classic triad of red-currant jelly stool, colicky abdominal pain, and palpable abdominal mass.1 Delay in diagnosis increases morbidity, including bowel ischemia and perforation, as well as mortality.
Small bowel-small bowel intussusceptions are frequent incidental findings as more cross-sectional imaging is performed in children. Most of these occur in the left upper quadrant in the jejunum and less often require additional workup or intervention. As small bowel-small bowel intussusceptions are incidental findings, children are usually asymptomatic. Symptomatic cases of small bowel intussusception can occur in a subset of children with predisposing underlying conditions.
In this article, we review the typical findings of intussusception in various imaging modalities used to diagnose ileocolic and small bowel intussusceptions and briefly discuss intussusception reduction. Key points regarding the lead points and ultrasound features of possible non-reducibility are highlighted, as they can be potential challenges to reducing an intussusception.
Imaging Modalities Used To Diagnose Intussusception
Radiography
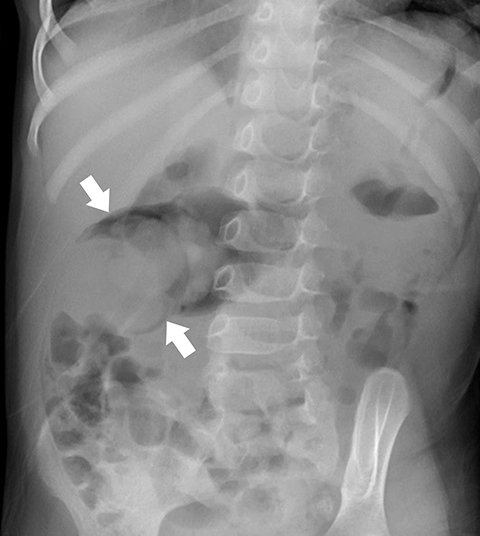
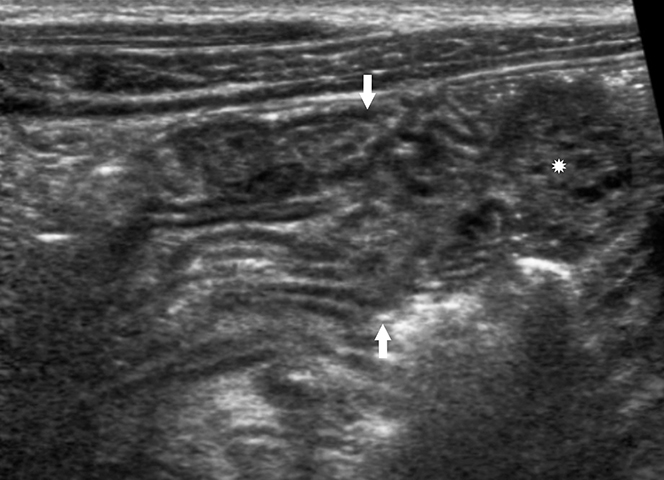
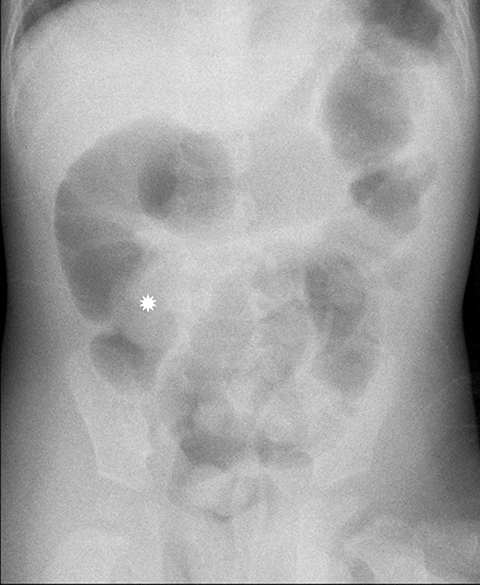
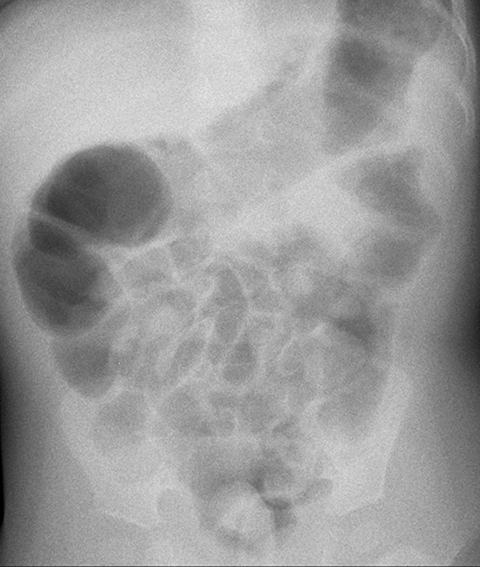
Radiography is neither diagnostic nor sensitive for intussusception detection, with a wide range of documented sensitivities that correspond to the number of views obtained. Two-view radiographs, including a supine view with a lateral decubitus or upright view, demonstrate a sensitivity of 62%.2 There are findings that raise the concern for intussusception and would warrant further imaging. The most specific finding on radiography is a round, soft-tissue mass within the upper abdomen that can be seen in up to 60% of X-rays (Figure 1).3 Surrounding regions of fat density corresponding to mesentery within the intussuscipiens may be identified. The crescent sign, a curvilinear area of air surrounding the soft tissue mass, may also be seen (Figure 1).3
A paucity of bowel gas and stool within the region of the cecum could also raise concern for an intussusception but does not exclude diagnosis because a stool-filled sigmoid colon may be located within the right lower quadrant and be mistaken for the cecum.1 Depending on the duration of symptoms, the abdominal radiograph may demonstrate a wide variety of bowel gas patterns ranging from normal to signs of a small-bowel obstruction. Radiographs are useful to exclude other diagnoses such as foreign body ingestion or pneumoperitoneum from a perforated viscus. If an ileocolic intussusception is present, a radiograph should be performed prior to reduction to exclude free air, as the presence of free air would preclude reduction.
Overall, radiography has poor diagnostic performance in intussusception and should not be considered first-line imaging.2 The recommended imaging algorithm is always to perform ultrasound first in a child with suspected intussusception.
Ultrasound
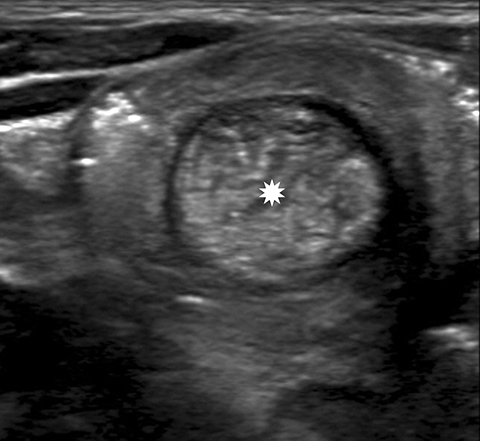
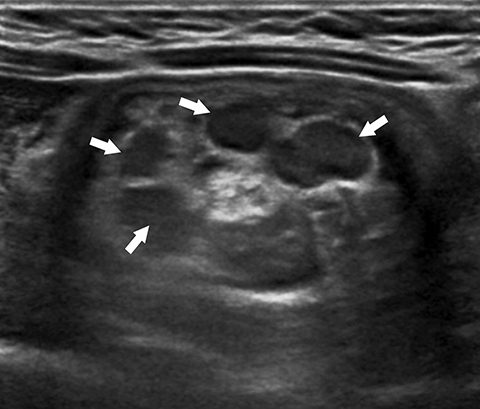
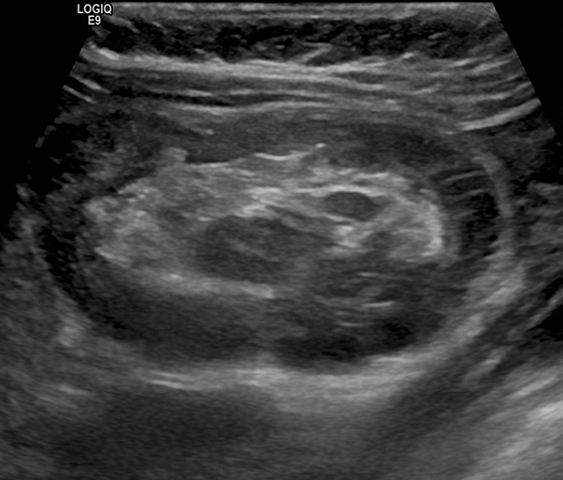
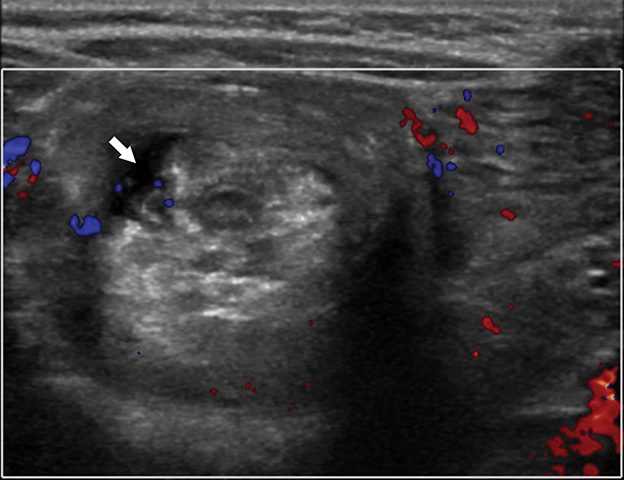
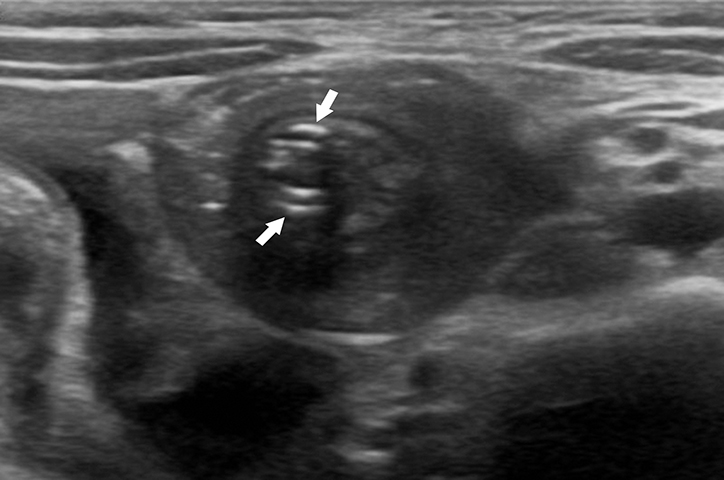
With a sensitivity of 97.9%, specificity of 97.8%, positive predictive value of 86.6%, and negative predictive value of 99.7%, ultrasound (US) is the gold standard for evaluating a suspected intussusception.4 An intussusception presents as a round mass with a target bowel-in-bowel appearance in the transverse plane, the classic finding on ultrasound (Figure 2). The features are unique in that they consist of concentric rings of bowel wall and internal hyperechoic mesenteric fat. Lymph nodes or the appendix may also be noted within the intussusceptum (Figure 3).
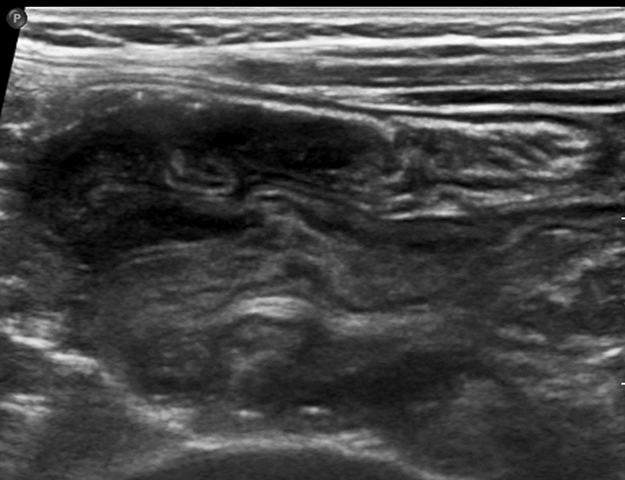
The diameter of an ileocolic intussusception can range from 1.4 cm to 4 cm, with a mean diameter of 2.6 cm.5,6 This is larger than the mean diameter of small bowel-small bowel intussusceptions, which is 1.4 cm.5,6 The target-appearing mass may be located anywhere in the abdomen depending on the site and length of the intussusception. In the longitudinal plane, the intussusceptum can be seen extending into the intussuscipiens and demonstrating multiple alternating hypoechoic and hyperechoic lines known as the “sandwich” sign (Figure 4). The “pseudo-kidney” sign can be seen on longitudinal scans depicted by a thickened intussusceptum bowel wall mimicking a reniform shape, with the internal echogenic mesentery of the intussusception representing the central echogenic fat complex of a normal adult kidney (Figure 5).7 Concomitant intraperitoneal free fluid can be seen in greater than 50% of cases.8
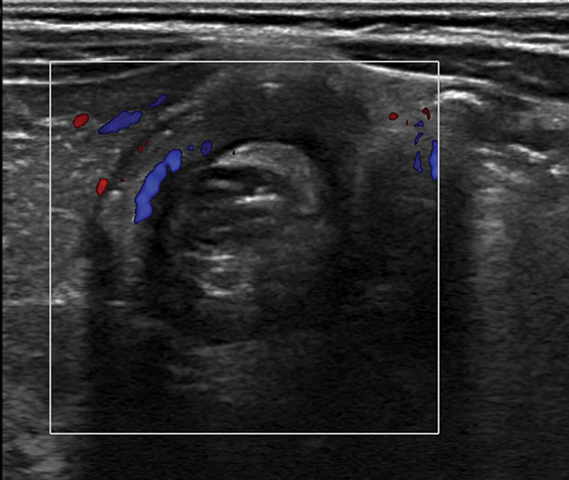
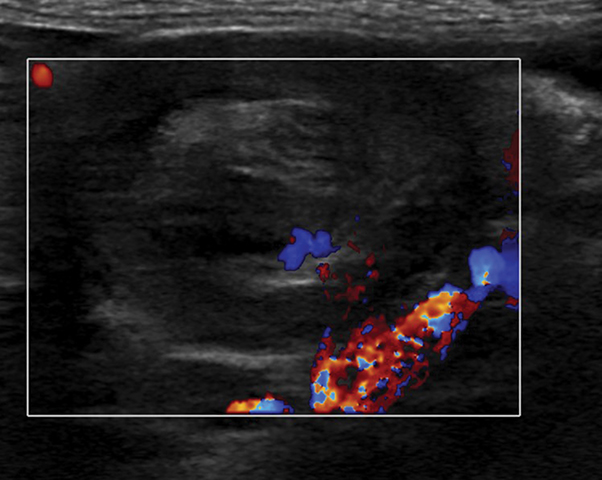
Specific findings on US can also assess the reducibility and potential complications related to reduction. Fluid trapped within the intussuscipiens and a lack of internal vascular flow on Doppler within the intussusceptum may indicate ischemia or necrosis and a potentially increased risk of enema reduction failure. However, this is not a contraindication; 26% of cases with trapped fluid and 31% cases without internal vascular flow result in a successful reduction (Figures 6,7).9-11 Irregular bowel wall or decreased bowel wall vascularity also suggests friable mucosa, a risk for perforation (Figure 8). Recognizing these features are important prior to performing any type of reduction because they can indicate potential procedural difficulty, predict non-reducibility, and alert the radiologist to have surgery on standby, owing to a higher-than-normal risk of perforation. All of these factors need to be considered in the decision process whether to pursue reduction.
One diagnostic limitation of US is the presence of extensive bowel gas, which can obscure evaluation. Also, a small bowel-small bowel intussusception can erroneously be diagnosed as an ileocolic intussusception owing to the overlap in size ranges of the targetoid mass.5,6 Perforated appendicitis can be mistaken for an intussusception if it is contained due to internal debris or if an appendicolith is inaccurately interpreted as mesenteric fat within an intussucepiens.12 Despite these limitations, ultrasound still has a very low false-negative rate of less than 1% and a low false-positive rate of 13%.4
MRI and CT
Magnetic resonance imaging (MRI) and computed tomography (CT) are not the conventional first-line imaging modalities for diagnosing intussusception. Unlike in children, intussusceptions are more commonly identified on CT and MRI in adults. There are no dedicated studies, only case reports, in the pediatric literature on the use of CT and MRI for intussusception. Radiologists should be aware of the MRI and CT appearances of intussusception, however, as they may be seen in children undergoing studies for other possible conditions. Small-bowel-small bowel intussusceptions are incidentally identified on CT and MRI more often than the ileocolic subtype. Whether an ileocolic or small bowel intussusception, these entities may involve a short or long segment and be seen anywhere in the abdomen.
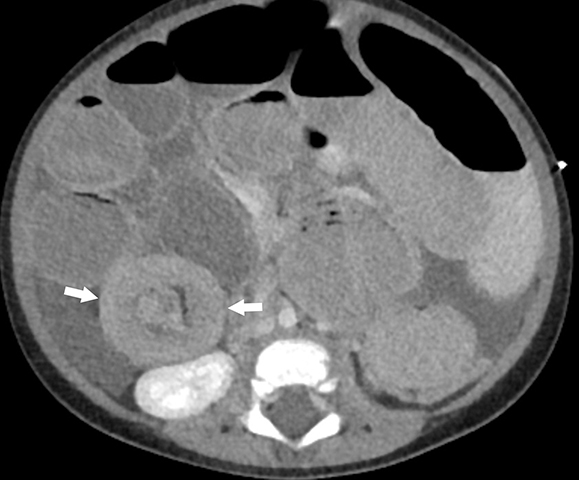
On CT, the typical target appearance of bowel within bowel will be seen with high-attenuation bowel wall, a concentric ring of hypodense mesenteric fat, and an additional internal region of higher-attenuation bowel (Figure 9). Intussusceptions of longer duration can appear more elongated and “sausage shaped” owing to associated edema.3 If administered, oral contrast can extend into the intussuscipiens. Computed tomography can also demonstrate sequelae of intussusception, such as small-bowel obstruction, as well as lead points in older children.
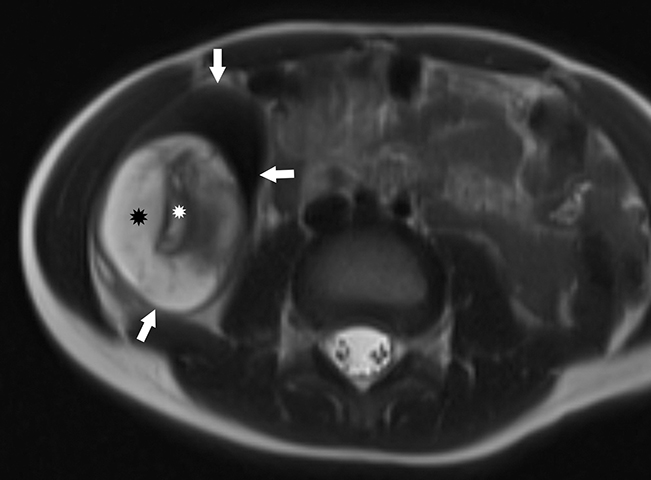
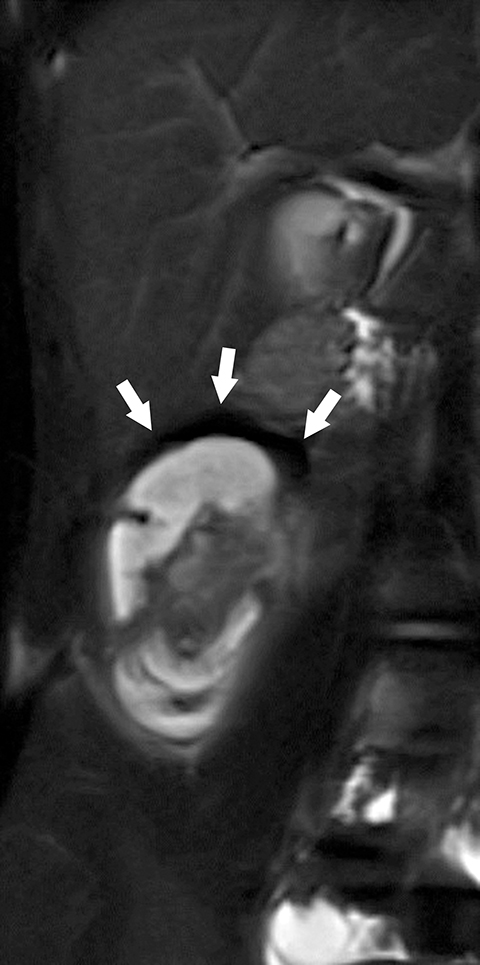
On MRI, an intussusception can best be visualized on a fluid sensitive sequence, which would demonstrate hyperintense intraluminal fluid with low-to-intermediate signal intensity of the bowel wall (Figure 10).3 Surrounding perienteric edema would also be present, as soft-tissue contrast is greater on MRI than on CT. Magnetic resonance imaging, like CT, can also readily visualize lead points such as duplication cysts, solid masses, or polyps.
Small bowel-Small bowel Intussusception
Small bowel-small bowel intussusceptions are often incidentally seen on US, CT, and MRI, and are typically self-limiting; therefore, they do not typically require follow-up imaging to document resolution. They are distinguished by location, often in the left upper quadrant, and by size, usually less than 2.5 cm.5 Many times when performing an US in real time, a small bowel-small bowel intussusception visualized at the beginning of the examination is resolved by the end of the examination and is reported as being transient. While the majority of small bowel-to-small bowel intussusceptions do not require intervention, ascites, small-bowel obstruction, or an intussusception length greater than 3.5 cm may require follow-up and possible surgical intervention. 13
Small bowel-small bowel intussusceptions are seen in specific conditions such as celiac disease and Henoch-Schonlein Purpura and can be visualized along the jejunal arm of a G-J tube (Figure 11). Radiologists should scrutinize for this when performing studies in this subset of pediatric patients. These small-bowel intussusceptions should be reported when interpreting US, CT, or MRI scans. We report location, size, associated findings, and the presence/absence of lead points, as well as whether they are persistent or transient throughout the examination.
Lead Points
While most ileocolic intussusceptions are idiopathic owing to lymphoid hypertrophy, 1.5-12% have a pathologic lead point.14 In contrast, intussusceptions in adults are rare; about 90% are caused by a definite lead point, such as neoplasm, or secondary to a postoperative condition.15 The most common pathologic lead point in a child is a Meckel diverticulum, with other etiologies including duplication cysts, polyps, or malignancies such as lymphoma.-14,16,17 Although most intussusceptions occur within the first year of life, the percentage of those with pathologic lead points increases with age.14,18
Pathologic lead points can cause small bowel-small bowel, ileocolic, or even colocolonic intussusceptions.19 Intussusceptions may also result from a preexisting condition with predisposition such as Henoch-Schönlein Purpura, Peutz-Jeghers syndrome, and cystic fibrosis.-14,16,17 A pathologic lead point may be seen on US; up to 66% of lead points are detected with the modality (Figure 12).16 A pathologic lead point is not a contraindication to enema reduction; however, while the intussusception can be reduced, there is an increased incidence of recurrence, with a recent study by Lin et al finding a recurrent intussusception rate of 78.5%.17 Ultimately, whether the intussusception is reduced, the pathologic lead point will require surgical treatment.
Techniques To Reduce Ileocolic Intussusception
Intussusception reduction can be performed under fluoroscopic guidance with either air or liquid contrast, or under ultrasound-guided hydrostatic reduction. The choice can be based on one’s training, experience, and available resources. However, a 2015 meta-analysis found air reduction superior to liquid, with no differences in perforation rates in either group.20 There is also significant contrast dose saving with air reduction; air reduction requires 2.7 times less contrast than liquid reduction.21 Prior to beginning the procedure, it is imperative to secure intravenous access, an abdominal radiograph excluding free air, all necessary equipment, and a pediatric surgeon to be available in the event of a complication such as a perforation.
Contraindications to the procedure include pneumoperitoneum or signs of peritonitis. The equipment required for reduction include a rectal tube and either a sphygmomanometer with a pressure release valve for pneumatic reduction, or a choice of contrast if performing a liquid reduction. The child should be accompanied by a nurse and monitored for the duration of the study. In addition, to prepare for possible perforation, a surgeon should be on standby and a large-gauge intravenous catheter should be available for decompression of the abdomen in the setting of a perforation with pneumatic reduction.
Formal, signed consent is not routinely obtained or required before intussusception reduction at many pediatric radiology practices. A more informal consent process occurs in the radiology suite, where the details and risks of the procedure are discussed with the parent(s)/guardian. The reduction does not start until the child’s guardian fully acknowledges these details and verbally agree to the procedure.
Fluoroscopically Guided Air Reduction
A tight air seal using taping, manually squeezing the buttocks, or inflating a balloon is required for fluoroscopically guided air reduction. The patient can be placed in the prone or supine position. The advantage of prone positioning is that it permits access to the child’s buttocks to acquire a tight rectal seal. It is also important not to exceed a maximum pressure of 120 mmHg and to employ a pop off valve as a safety precaution. The endpoint of air reduction is to see air flood the small bowel (Figure 13). If there is concern that the intussusception has not reduced completely—an edematous ileocecal valve (ICV) can mimic residual intussusception—a targeted US can be performed immediately in the fluoroscopy suite for confirmation. Some may feel that bowel air in the aftermath of reduction can impair identification of a residual intussusception; however, this has not been true in our experience.
Fluoroscopically Guided Liquid Reduction
Liquid reduction is usually performed with an iso-osmolar, water-soluble contrast agent to ensure the highest level of safety, although recent surveys have found that 25% of pediatric radiologists use Gastrografin, and 16% report using barium, as their liquid contrast of choice.22 Gastrografin is hyperosmolar and must be used with great caution; in our experience this agent should be avoided owing to its risk of causing electrolyte imbalance and possibly shock.
The general rule for using liquid contrast is to hold the enema bag three feet above the table and to make three attempts to reduce the intussusception. However, situations may arise where this rule may be modified and the reduction attempt may be longer. The radiologist may consider this in the interest of the patient to attempt a longer reduction to avoid surgery. Again, all safety precautions should be maintained throughout the procedure.
Ultrasound-guided Reduction
Ultrasound-guided reduction is employed by few pediatric radiologists. Based on 2015 data, only 4% of surveyed pediatric radiologists reported using US-guided hydrostatic reduction. In this method, a saline enema is hung and an US probe is used to follow the flow of saline as it pushes the intussusception to the ICV. The termination point occurs when the saline is seen traversing the ICV and flooding the small bowel. Ultrasound-guided hydrostatic reduction is advantageous in that no ionizing radiation is employed and any residual or incomplete reduction can be readily recognized.
Traditionally, a balloon has not been used during enema reduction—its use is controversial—but recent literature has shown a balloon can be effective.23,24 Proponents have argued the likelihood of successful reduction may increase with a balloon inflation; however, a higher rate of perforation has been found in children younger than 9 months.24 Overall, balloon inflation should be performed with caution and only by experienced radiologists.
Signs of unsuccessful reduction have been described on diagnostic US; however, two important signs must be recognized. The first is frank perforation with free intraperitoneal air during reduction, or frank spillage of contrast or saline into the abdomen during liquid reduction. Free air is recognized as air outlining the bowel wall between loops of bowel, rapidly increasing abdominal girth, and lucency over the liver and spleen. Regardless of liquid or pneumatic reduction, the procedure should immediately be terminated and the pediatric surgeon notified in the event of perforation. A large amount of air identified within the abdomen and causing vascular compromise may require emergent needle decompression of the abdomen in the fluoroscopy suite.
The second important sign of unsuccessful reduction is the “dissection sign,” in which air traverses the intussusception and fills the small bowel as an air lock without generating sufficient pressure to retrogradely reduce the intussusception further.25 As a result, air bypasses the intussusception and impedes further reduction. Reduction in this case is more likely to be unsuccessful, but some experienced radiologists may still be able to complete reduction.
Unsuccessful reduction does not always require surgery. Some radiologists will wait less than 30 minutes to a few hours after the first reduction and attempt a delayed reduction, as long as the patient remains stable. There are no guidelines on how long to wait, but significant success rates after a wait-and-watch period have been reported.26, 27
Conclusion
Intussusception is common in children and can be readily diagnosed by a combination of clinical symptoms and ultrasound findings. Upon diagnosis of ileocolic intussusception, several safe and effective radiologic methods of reduction are available. Small bowel-small bowel intussusceptions are often incidental and cannot be reduced, but they are typically self-limiting and resolve spontaneously. Identifying lead points can be challenging but is required in older children presenting with either ileocolic or small-bowel intussusception. Finally, delayed reduction should be considered, as it can lead to greater success in avoiding unnecessary surgery.
References
- Daneman A, Navarro O. Intussusception. Part 1: a review of diagnostic approaches. Pediatr Radiol. 2003;33(2):79-85.
- Henderson AA, Anupindi SA, Servaes S, et al. Comparison of 2-view abdominal radiographs with ultrasound in children with suspected intussusception. Pediatr Emerg Care. 2013;29(2):145-150.
- Byrne AT, Geoghegan T, Govender P, et al. The imaging of intussusception. Clin Radiol. 2005;60(1):39-46.
- Hryhorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009;39(10):1075-1079.
- Park NH, Park SI, Park CS, et al. Ultrasonographic findings of small bowel intussusception, focusing on differentiation from ileocolic intussusception. Br J Radiol. 2007;80(958):798-802.
- Lioubashevsky N, Hiller N, Rozovsky K, et al. Ileocolic versus small-bowel intussusception in children: can US enable reliable differentiation? Radiology. 2013;269(1):266-271.
- Anderson DR. The pseudokidney sign. Radiology. 1999;211(2):395-397.
- Feinstein KA, Myers M, Fernbach SK, et al. Peritoneal fluid in children with intussusception: its sonographic detection and relationship to successful reduction. Abdom Imaging. 1993;18(3):277-279.
- del-Pozo G, Gonzalez-Spinola J, Gomez-Anson B, et al. Intussusception: trapped peritoneal fluid detected with US--relationship to reducibility and ischemia. Radiology. 1996;201(2):379-383.
- Lim HK, Bae SH, Lee KH, et al. Assessment of reducibility of ileocolic intussusception in children: usefulness of color Doppler sonography. Radiology. 1994;191(3):781-785.
- Kong MS, Wong HF, Lin SL, et al. Factors related to detection of blood flow by color Doppler ultrasonography in intussusception. J Ultrasound Med. 1997;16(2):141-144.
- Newman B, Schmitz M, Gawande R, et al. Perforated appendicitis: an underappreciated mimic of intussusception on ultrasound. Pediatr Radiol. 2014;44(5):535-541.
- Munden MM, Bruzzi JF, Coley BD, et al. Sonography of Pediatric Small-Bowel Intussusception: Differentiating Surgical from Nonsurgical Cases. AJR Am J Roentgenol. 2007;188(1):275-279.
- Blakelock RT, Beasley SW. The clinical implications of non-idiopathic intussusception. Pediatr Surg Int. 1998;14(3):163-167.
- Choi SH, Han JK, Kim SH, et al. Intussusception in adults: from stomach to rectum. AJR Am J Roentgenol. 2004;183(3):691-8.
- Navarro O, Dugougeat F, Kornecki A, et al. The impact of imaging in the management of intussusception owing to pathologic lead points in children. A review of 43 cases. Pediatr Radiol. 2000;30(9):594-603.
- Lin XK, Xia QZ, Huang XZ, et al. Clinical characteristics of intussusception secondary to pathologic lead points in children: a single-center experience with 65 cases. Pediatr Surg Int. 2017;33(7):793-797.
- Ong NT, Beasley SW. The leadpoint in intussusception. J Pediatr Surg. 1990;25(6):640-643.
- Devita R, Towbin RB, Towbin AJ. Burkitt lymphoma causing colocolonic intussusception. Appl Radiol. 2019;48(1):48A-48C
- Sadigh G, Zou KH, Razavi SA, et al. Meta-analysis of Air Versus Liquid Enema for Intussusception Reduction in Children. AJR Am J Roentgenol. 2015;205(5):W542-549.
- Kaplan SL, Magill D, Felice MA, et al. Intussusception reduction: Effect of air vs. liquid enema on radiation dose. Pediatr Radiol. 2017;47(11):1471-1476.
- Stein-Wexler R, O’Connor R, Daldrup-Link H, et al. Current methods for reducing intussusception: survey results. Pediatr Radiol. 2015;45(5):667-674.
- Betz BW, Hagedorn JE, Guikema JS, et al. Therapeutic enema for pediatric ileocolic intussusception: using a balloon catheter improves efficacy. Emerg Radiol. 2013;20(5):385-391.
- Golriz F, Cassady CI, Bales B, et al. Comparative safety and efficacy of balloon use in air enema reduction for pediatric intussusception. Pediatr Radiol. 2018;48(10):1423-1431.
- Fishman MC, Borden S, Cooper A. The dissection sign of nonreducible ileocolic intussusception. AJR Am J Roentgenol. 1984;143(1):5-8.
- Gorenstein A, Raucher A, Serour F, et al. Intussusception in children: reduction with repeated, delayed air enema. Radiology. 1998;206(3):721-724.
- Navarro OM, Daneman A, Chae A. Intussusception: the use of delayed, repeated reduction attempts and the management of intussusceptions due to pathologic lead points in pediatric patients. AJR Am J Roentgenol. 2004;182(5):1169-76.
Citation
R D, S A, A K.How to Diagnose Intussusception in Children. Appl Radiol. 2021; (1):19-27.
January 19, 2021