Hepatic Peliosis
Case Summary
A middle-aged patient presented with complaints of general malaise, loss of appetite, and weight loss of about 20 pounds during the prior 6 months. The past clinical history was unremarkable, except for alcohol use disorder treatment 5 years earlier. Physical examination revealed moderate hepatosplenomegaly, and blood tests showed moderately elevated liver enzymes. The provisional diagnosis was cirrhosis or hepatitis. Contrast-enhanced CT of the abdomen demonstrated a diffuse abnormality of the liver parenchyma. A hepatic arteriogram was performed, and a percutaneous liver biopsy was subsequently obtained.
Imaging Findings
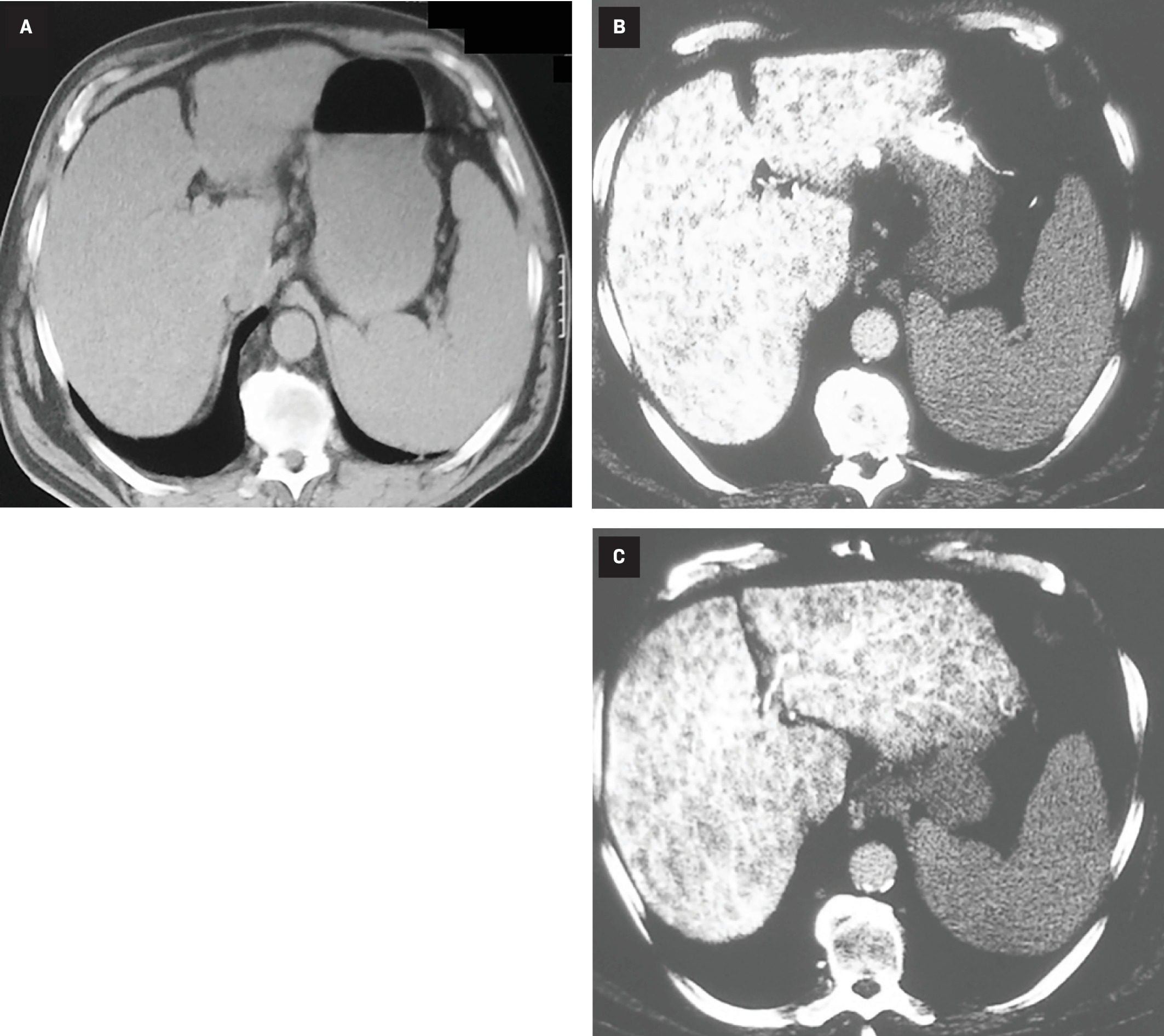
Noncontrast images of the abdomen showed hepatomegaly with a slightly mottled appearance and associated splenomegaly. Arterial phase imaging disclosed diffuse involvement of the liver with low-attenuation foci that produced a fenestrated sponge-like or “Swiss cheese” appearance of the hepatic parenchyma. These foci gradually filled with contrast material and became isodense with the liver on the delayed phase of the examination ( Figure 1 ).
CT features of hepatic peliosis. Noncontrast axial image of the upper abdomen ( A ) shows a slightly mottled liver with coexistent splenomegaly. Arterial phase ( B ) reveals diffuse involvement of the liver by numerous hypodense lesions causing sponge-like or “Swiss cheese” appearance of the hepatic parenchyma when viewed on a bone-window setting. Delayed venous phase ( C ) demonstrates opacification of these structures within the hyperattenuated liver.
A catheter hepatic arteriogram demonstrated that the liver contained numerous small vascular structures that filled with contrast in the arterial phase and retained them during the venous phase ( Figure 2 ). There was no arterioportal shunting or extravasation of the injected contrast material.
Radiographs from the selective hepatic arteriography. Arterial phase ( A ) demonstrates opacification of many small and irregularly shaped lesions of the liver. Delayed image ( B ) shows retained contrast material within dilated sinusoids, a characteristic feature of hepatic peliosis.

Liver biopsy disclosed dilated sinusoids of the liver containing intraluminal red cells within otherwise normal tissue.
Diagnosis
Hepatic peliosis.
Differential diagnosis includes bacillary peliosis, hemangiomatosis of the liver, biliary hamartomas, microabscesses, diffuse metastases, and regenerative nodules.
Discussion
The hepatic sinusoids are vascular spaces lined by endothelial and Kupffer cells that interconnect the distal branches of the hepatic artery with the portal vein since the usual capillaries do not exist in the liver. With hepatic peliosis, a marked dilatation of these sinusoids involve part of or the entire liver.1 These irregularly shaped blood-filled cavities cause sponge-like transformation of the hepatic parenchyma, which can be visible on the pathological specimens as well as on cross-sectional imaging modalities.2 - 6 The dilated sinusoids in peliosis may be 1 to 2 mm to several centimeters in diameter, while larger lesions may have a “pseudotumor” appearance and be complicated by intrahepatic rupture and hemorrhage, and may ultimately require liver transplantation.2, 7
During a contrast-enhanced CT or hepatic angiography, the dilated sinusoids gradually fill with injected contrast material, retain it in the delayed phase of the study, and eventually become isodense throughout the liver ( Figures 1 , 2 ). MRI of hepatic peliosis showed a mottled appearance of the liver, with dilated sinusoids being hypointense on T1, hyperintense on T2, and markedly enhancing after intravenous gadolinium-based contrast agent administration.2, 3, 5 The sonographic features of dilated sinusoids are heterogeneously hypoechoic lesions with irregular shapes and well-defined margins.4
The exact pathogenesis of peliosis has not been ascertained, and about 50% of cases are considered idiopathic. However, an association with the use of anabolic hormones, oral contraceptives, other medications such as tamoxifen, and chronic debilitating diseases like tuberculosis and cancer has been reported.1 - 3
A similar condition called bacillary peliosis occurs in patients with acquired immune deficiency syndrome who are infected by Bartonella henselae or Bartonella quintana, the gram-negative bacteria causing cat scratch disease. These patients present with concurrent involvement of the liver, spleen, and lymph nodes, and can be treated with antibiotics such as erythromycin.2, 8
Hepatic peliosis is usually asymptomatic and discovered incidentally in patients undergoing imaging studies for unrelated medical reasons.2 - 6 Its rare occurrence in infants and children has been reported, but the vast majority of cases involve middle-aged adults and show no gender preference. The observed findings can occasionally diminish or resolve following discontinuation of the responsible medications or causal agents.1, 2 However, many patients eventually develop complications owing to liver failure, portal hypertension, intrahepatic hemorrhage, and ascites. Conservative treatment of this patient did not prove beneficial, and the persistent findings on follow-up imaging studies prompted referral for liver transplant as the recommended treatment for diffuse hepatic peliosis.9
Conclusion
Hepatic peliosis is a distinct pathological entity, manifested by dilated sinusoids due to various etiological factors. These blood-filled cavities present a Swiss cheese appearance of the liver on CT images. Correct diagnosis is important since this disease may culminate in spontaneous intrahepatic rupture and the eventual need for a liver transplant.
References
Citation
Ghahremani GG, Naimi DR.Hepatic Peliosis. Appl Radiol. 2024; (5):42 - 44.
doi:10.37549/AR-D-24-0009
October 1, 2024