GIST of the Duodenum and Proximal Jejunum with an Ampullary Neuroendocrine Tumor
Images




CASE SUMMARY
A 58-year-old with a history of neurofibromatosis type 1 (NF-1) and recurrent nephrolithiasis presented to the emergency department with right flank pain.
IMAGING FINDINGS
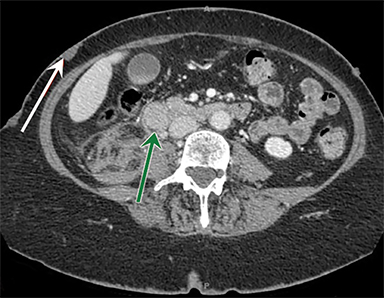
Abdominal radiographs were unremarkable. Contrast-enhanced CT (CECT) of the abdomen revealed a right renal subcapsular hematoma and multiple masses in the duodenum. The largest of these being a 2cm mass in the second portion of the duodenum, along with numerous subcutaneous soft-tissue nodules (Figure 1).
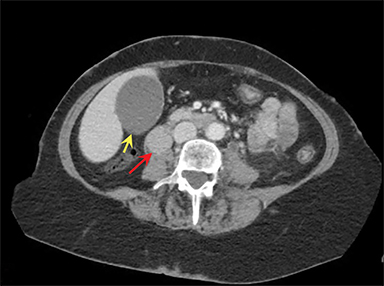
The same patient presented 3.5 years later with diffuse abdominal pain. Repeat CECT of the abdomen revealed pancreaticobiliary obstruction along with findings suggestive of gallbladder hydrops secondary to a 2cm duodenal mass and an obstructing left nephrolith (Figure 2). Surgery revealed a neuroendocrine neoplasm of the ampulla of Vater and five tumors in the duodenum and proximal jejunum, the largest measuring 3.7cm.
DIAGNOSIS
Gastrointestinal stromal tumors (GISTs) of the duodenum and proximal jejunum with an ampullary neuroendocrine tumor (NET).
DISCUSSION
The coexistence of a periampullary/ampullary NETs and multifocal GIST is nearly pathognomonic of NF-1.1 Although intra-abdominal tumors are common in the setting of NF-1, the concurrence of these two entities is rare. A majority of NETs in NF-1 are nonfunctional, even in cases of histologically confirmed somatostatinomas, the most common being periampullary/ampullary NET.2
In most cases, NETs and GISTs are asymptomatic and found incidentally on imaging. Uncommonly, they present with abdominal pain, upper GI bleed, palpable abdominal mass, bowel obstruction, perforation and/or biliary obstruction.3,4 Extremely rare cases of ampullary insulinoma, gastrinoma, gangliocytic paragangliomas, and adenocarcinomas associated with multifocal GISTs have been reported.2 Peripheral nerve sheath tumors commonly occur in NF-1, and 1-3% of patients develop pheochromocytomas.3
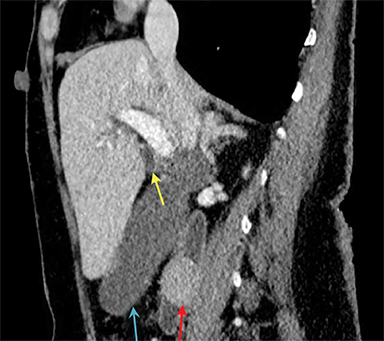
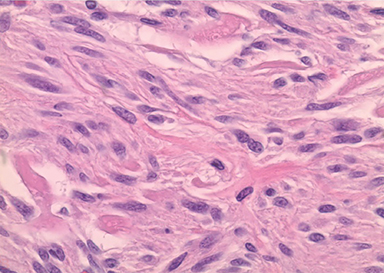
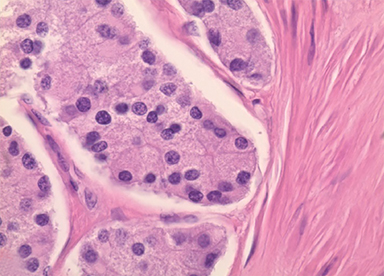
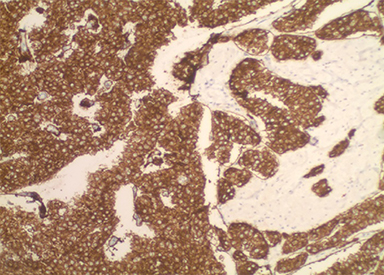
These cases must be differentiated from other hereditary and nonhereditary tumor syndromes, such as multiple endocrine neoplasias, Carny triad, and Carney-Stratakis syndrome, all of which have a propensity to coexist with GIST. In this case, the ampullary tumor was well differentiated and stained positive for synaptophysin and chromogranin confirming the diagnosis of a NET (Figures 3,4). The five additional tumors had spindle cell histology and were positive for c-kit immunohistochemistry, confirming the diagnosis of multifocal GIST.
GISTs are the most common gastrointestinal manifestation of NF-1, with one third of patients found to have GISTs at autopsy.5 While cutaneous manifestations of NF-1 are generally reported earlier, GISTs present with a mean age of 53 years, 8 years earlier than the average presentation of sporadic GIST. In addition, compared to sporadic GIST associated with NF-1 are more commonly occur in the small bowel rather than the stomach, and have a smaller mean diameter, 3.8 cm vs. 7.4 cm.4 Radiographically, the appearance of GIST varies based on size and location. Nonetheless, they appear as homogeneous soft-tissue masses with or without signs of central necrosis.
CONCLUSION
This case illustrates the importance of radiographically recognizing the intra-abdominal manifestations of NF-1. Particularly, NF-1 predisposes to ampullary/periampullary neoplasia and small-bowel GIST formation. In the undiagnosed patient, the coexistence of these two entities is highly suggestive of NF-1. Over time, periampullary tumors can lead to complications such as pancreaticobiliary obstruction, as this case. GI tumors in patients with NF-1 often present earlier than sporadic tumors and imaging studies should be evaluated with this in mind.
REFERENCES
- Agaimy A, Vassos N, Croner RS. Gastrointestinal manifestations of neurofibromatosis type 1 (Recklinghausen’s disease): clinicopathological spectrum with pathogenetic considerations. International Journal of Clinical and Experimental Pathology. 2012;5(9):852-862.
- Costi R, Caruana P, Sarli L, Violi V, Roncoroni L, Bordi C. Ampullary adenocarcinoma in neurofibromatosis type 1. Case report and literature review. Mod Pathol. 2001;14:1169-74.
- Kramer K, Hasel C, Aschoff AJ, Henne-Bruns D, Wuerl P. Multiple gastrointestinal stromal tumors and bilateral pheochromocytoma in neurofibromatosis. World J Gastroenterol.; WJG. 2007;13(24):3384-3387. doi:10.3748/wjg.v13.i24.3384.
- Salvi PF, Lorenzon L, Caterino S, Antolino L, Antonelli MS, Balducci G. Gastrointestinal Stromal Tumors Associated with Neurofibromatosis 1: A Single Centre Experience and Systematic Review of the Literature Including 252 Cases. International Journal of Surgical Oncology. 2013; 2013:398570. doi:10.1155/2013/398570.
- Zoller ME, Rembeck B, Oden A, Samuelsson M, Angervall L. Malignant and benign tumors in patients with neurofibromatosis type 1 in a defined Swedish population. Cancer. 1997;79:2125–2131.
Citation
M M, J B, A T.GIST of the Duodenum and Proximal Jejunum with an Ampullary Neuroendocrine Tumor. Appl Radiol. 2020; (5):49-51.
September 1, 2020