Giant right gastroepiploic artery pseudoaneurysm with an IVC fistula
Images


CASE SUMMARY
An 81-year-old Caucasian woman presented to the emergency department (ED) for evaluation of abdominal pain. She reported sharp epigastric pain that radiated to her back, along with intermittent abdominal pain for 5 days. She stated the pain was 10 out of 10 in severity and denied any other symptoms. Upon physical examination, the patient had superior epigastric abdominal tenderness to palpation with guarding. A computed tomography angiogram (CTA) of the thorax, abdomen, and pelvis was performed for concerns of an aortic dissection. This demonstrated a giant pseudoaneurysm measuring 10 cm x 4.8 cm within the gastroduodenal artery distribution with associated active extravasation secondary to pancreatitis.
IMAGING FINDINGS
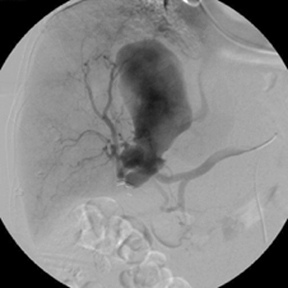
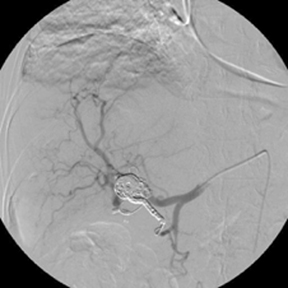
The CTA demonstrated a multi-lobulated, large, sub-hepatic pseudoaneurysm measuring 10 cm x 4.8 cm arising from the gastroduodenal artery/right gastroepiploic artery distribution with adjacent active extravasation (Figure 1). These findings were secondary to pancreatitis. Interventional radiology was consulted for further evaluation. Catheter-directed angiography of the gastroduodenal artery demonstrated a giant pseudoaneurysm with active extravasation arising from the right gastroepiploic artery with fistulous communication with the inferior vena cava (IVC) (Figure 2). Postembolization angiogram of the common hepatic artery demonstrated resolution of the pseudoaneurysm and active extravasation (Figure 2).
DIAGNOSIS
Giant right gastroepiploic artery pseudoaneurysm with an IVC fistula
DISCUSSION
A pseudoaneurysm of the right gastroepiploic artery (RGEA) is rare and potentially life threatening due to risk of rupture. This can occur from pancreatitis. RGEA pseudo-aneurysms, although uncommon, are three times more common in men than in women, occurring at an average age of 65 years. They account for fewer than 4% of all aneurysms involving the splanchnic arteries.1,2 Visceral pseudoaneurysms are more commonly seen due to atherosclerosis and trauma, and less commonly observed with an inflammatory process such as pancreatitis.3
Due to their proximity to the pancreas, the arteries of the celiac axis render the risk of pseudoaneurysm formation by adjacent periarterial inflammation from pancreatitis.3 The process and products of inflammation, along with the high-pressure flow from arteries, weakens the vessel walls resulting in pseudoaneurysm formation. In even rarer instances, a fistula from the pseudoaneurysm to the IVC can occur, as in our patient. The greatest risk of this condition is rupture of the pseudoaneurysm, which increases with size. In our patient, the pseudoaneurysm measured 10 cm. The most common symptom patients experience is vague abdominal pain. If rupture occurs, then presentation of shock will be appreciated.4,5
Computed tomography angiography can help make a diagnosis; however, definitive diagnosis must be made with catheter angiography.5 Treatment options include surgery and endovascular procedures. The appropriate treatment option depends on measurements, whether the pseudoaneurysm has ruptured, and vital signs of the patient. In our patient, hemodynamic stability was assessed. Together with the initial CTA and diagnosis, we felt that coil embolization was the best treatment option, given the size and high probability of frank rupture. Also, treatment with liquid embolic or glue could have resulted in non-target embolization of the pulmonary arteries through the fistula with the IVC. Endovascular treatment with coil embolization not only resolved the giant pseudoaneurysm, but prevented a more invasive treatment option such as laparotomy.
CONCLUSION
Right gastroepiploic artery pseudoaneurysms are rare, and even rarer in the development of a venous fistula. Nonetheless, it is a complication of pancreatitis. Its characteristic presentation of vague abdominal pain requires further investigation with CT imaging. Treatment should promptly follow diagnosis due to the high risk of rupture. Depending on size, rupture, and physical presentation of the patient, several treatment options are available. Coil embolization of the giant pseudoaneurysm was successful in this patient with no further complications.
REFERENCES
- Stanley JC, Thompson NM, Fry WJ. Splanchnic artery aneurysms. Archives of Surgery 1970; 838-839. 101:689-97.
- Stanley JC, Whitehouse Jr WM. Splanchnic artery aneurysms. Journal of Vascular surgery 1984; 798-813.
- Pattanshetty D, Bhat P. Left gastric artery pseudoaneurysm as a sequelae of chronic pancreatitis: recognizing a life-threatening complication. Central European Journal of Medicine. 2014; 9(3) 370-373. doi: 10.2478/s11536-013-0302-2.
- Jauhari A, Shrivastava, A, Soni RK, Darbari, A. pseudoaneurysm of aberrant right gastroepiploic artery mimicking pseudocyst of pancreas – a rare case report. Journal of Clinical and Diagnostic Research 2017; 11(4) 9-10. doi: 10.7860/JCDR/2017/25314.9651.
- Murakami Y, Saito H, Shimizu S, Kono Y, Kurodo H, et al. A Case of unruptured right gastroepiploic artery aneurysm successfully resected by laparoscopic surgery. Yonago Acta Medica 2017; 60(1) 56-58.
Citation
J S, D P, A R, CC Z.Giant right gastroepiploic artery pseudoaneurysm with an IVC fistula. Appl Radiol. 2018; (11):32-33.
November 8, 2018