Exploring the potential use of holographic imaging in radiology
Images
Holography is a process that creates three-dimensional images called holograms using laser beams, the properties of interference and diffraction, light intensity recording, and illumination of the recording.1 The images change according to the relative position of the individual viewer as if the objects displayed are actually present.
Two types of holography are available: Conventional and dynamic. Conventional holography represents static images of 3D objects whereby a change in viewing angle of the viewer results in a change of perspective of the holographic object. Dynamic holograph, meanwhile, adds motion to the 2D or 3D object.2
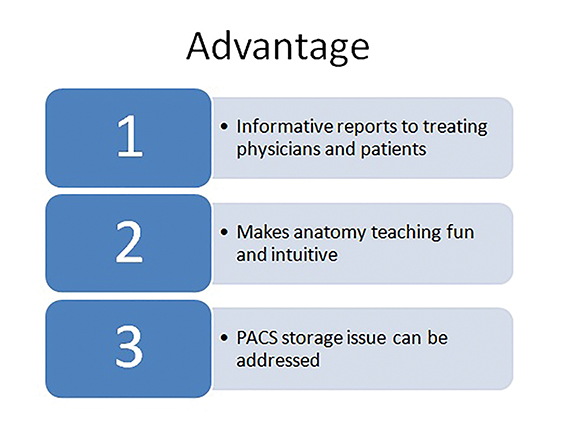
This addition of motion represents a significant advancement to current 3D displays, which can only show 3D static images. It also opens the door to three major potential uses of holography in radiology: teaching anatomy, PACS storage, and displaying more complex anatomic images that can be used to present more informative reports to treating physicians and their patients (Figure 1). This article explores these potential uses of holography in radiology.
Background of holography
The term “holography” was first coined by Dennis Gabor, who discovered the process accidentally while performing research into improving electron microscopes in 1948; Gabor subsequently was honored with the Nobel Prize for this work.3,4 In 1962, the development of lasers led to holograms that recorded 3D objects. Until recently, holographic display technology only allowed for the display of static objects, but research into this field has led to the development of holographic volumetric displays, which can render dynamic images at two frames per second.5 Improvements in this technology can lead to applications in medicine. Current digital holograms can allow us to see objects in three dimensions without using 3D glasses, as they are auto stereoscopic.
Definition and process of digital holography
Holography permits a light field, which generally results from a light source scattered off objects, to be recorded and later reconstructed when the original light field and original object is no longer present.6 Digital holograms are made up of holographic elements (hogels) rather than pixels or voxels. In contrast to normal pixels used in photography, hogels contain 3D information from multiple perspectives.7
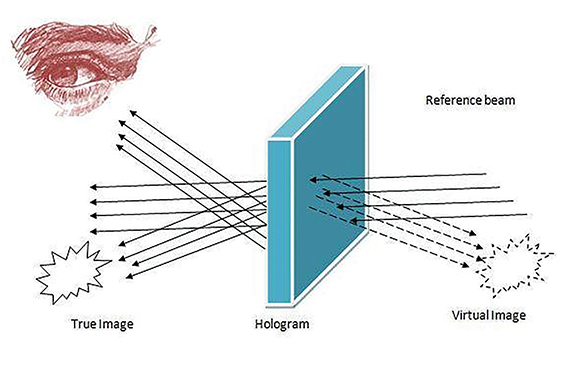
Digital holography is a two-step process. Step one involves recording the hologram where the radiographic image is transformed into a photographic record. Step two consists of reconstruction, in which the hologram is transformed into a virtual image. This process occurs due to interference between two waves. A hologram can be made by shining one part of the light beam directly onto the recording medium, and the other part onto the object in such a way that some of the scattered light falls onto the recording medium. When the two laser beams reach the recording medium, their light waves intersect and interfere with each other. It is this interference pattern that is imprinted (Figure 2). The digital hologram created contains a grid of holographic pixels, also known as holopixels or the aforementioned hogels. Holopixels are diminishing in scale, currently around 0.8 mm and now reducing to 0.5 mm or even 0.25 mm.
Any type of 3D medical dataset, such as CT and MR images, can be converted to a digital hologram.
Such data can also be available in the form of a physical scan of an object, a mathematical description of the images, molecular data, or even a series of stills or video.8 For example, a 200 × 300 mm page-sized hologram with 0.8 mm hogel requires the creation of approximately 90,000 2D images.8 This target can be reached by using a combination of advanced computer modeling software with graphics rendering as well as specific proprietary algorithms, customized hardware engines can run a series of mathematical processes to generate the image data.9
Potential applications in radiology
As noted previously, there are three potential uses of holography in radiology: teaching radiologic anatomy, as a potential candidate for PACS storage and for image display. We will now explore these uses in greater detail.
Teaching anatomy
The medical hologram, particularly in radiology, presents a performance boost over traditional textbook images. It brings in the “charm and has the potential to generate curiosity.”10 This can be achieved by using static holographic images of anatomical structures in textbooks, which can then easily display the relation of body structures with respect to each other in three dimensions.
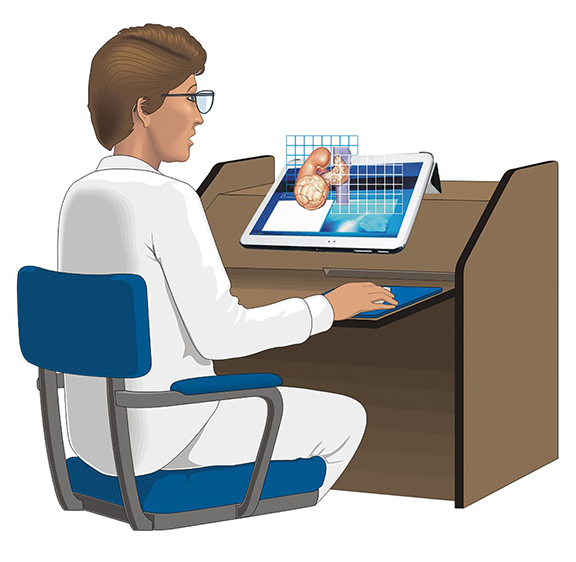
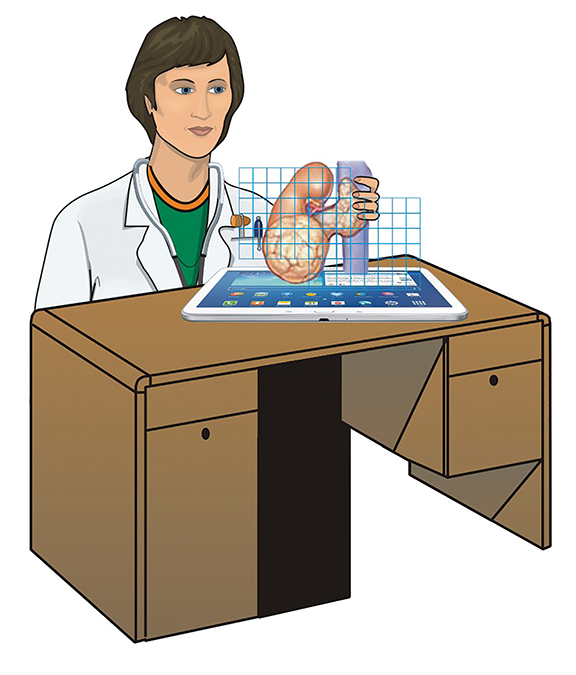
The 3D nature of the image generated provides superior visual capabilities. In a routine two-dimensional image many anatomical structures are difficult to conceptualize, such as the spatial relationships between various blood vessels. The normal and pathological structures can be easily understood by gauging such depth relationships. This can potentially be used in assessing mediastinal, vascular anatomy, the skull base, cranial nerves, and the renal, pelvic anatomy on CT or MRI images (Figures 3 and 4). The concept of optical composition suggests that the 3D concept relies on grouping visual subcomponents based on textures, color grade, and linking of structures.11
Holoxica worked with the Clinical Research Imaging Centre (CRIC) at Edinburgh University on a full-color digital hologram of a pair of lungs from a CT scan.8 This technique enabled the intricate detail of the anatomical structures to be visualized. It has also been documented to be used to image the liver from ultrasound scans. Complex holograms containing information layers from images of the musculoskeletal system, vascular and nervous system are now possible.
PACS storage
There has been renewed interest in holography due to the recent propagation of 3D content and availability of 3D data from CT, MRI and ultrasound scanners, low-cost depth scanners, cinema/TV and 3D printing. Holographic storage and retrieval systems can be looked upon as a solution to calls for greater storage capacity, rapid retrieval, and smaller physical storage footprints.12
Current radiology study image sizes vary from 10 megabytes (MB) to 90 MB in size per test. By adopting PACS, there has been a turnaround in radiology productivity by channeling radiology workflow.13 Holographic media can be used specifically for data storage due to their unique ability to store information in three dimensions, in contrast to standard optical disks, which manage to store data only on the surface. In the near future there is a high probability that this technology can eventually replace magnetic, single-layer storage by optical, 3-dimensional holograms.14 Radiology units depend on PACS to achieve their goals of high-speed access to images, steadfastness and efficacy.
Due to the unique ability of holograms to store data as a volumetric density and read it quickly, they are likely to become the storage medium of choice in the future. A DVD or optical disc player can read data at a rate which is exponentially slower compared to holography. Holographic recording and storage, therefore, can help significantly in intelligent PACS management.15 With advancements in computer technology this “new age” technology is now economically feasible for mass production. Holography is gradually making the transition from the research stage of the 1970s to its present potential as a commercial product. PACS currently requires excessive amounts of data storage, which can have up to 1000 times greater storage capacity using holographic technology compared to current methods.14,16,17
A rough estimate shows that high-resolution and specialized CT scans may occupy around 30 MB of data per scan. Over the last decade the quality of investigations has changed. Scans are now more focused, are of higher resolution and more detailed due to thinner sections and dynamic studies which are possible under both CT and MRI studies’ ability to create huge amounts of data. The current estimate suggests that for every 100,000 examinations performed, there will be a need to book approximately 3.1 terabytes of storage.14,18
The advantages of holography for data storage also include its ability to perform massive parallel recording and reading of data, unlike traditional optical disc, thus enabling significantly faster data transfer speeds in comparison to traditional optical discs.19 Another advantage is its ability to use the entire thickness of the recording media instead of just the surface.14 Holographic media are sensitive to light; using lasers, data can be recorded in 3-dimensional spaces. With holography, we can record 1 million bits of data with a single flash of light.20
Comparative data suggests that the cost for the new holographic media will probably be somewhere in the neighborhood of $0.06-$0.20 per gigabyte (GB) compared to data tape, which costs between $0.25 and $1, and videotape which costs between $1 and $3 per GB.14 Significant research over hard disk drives has presently taken the cost to an average of about $0.2 per GB, however, further reduction in cost is likely going to require newer technologies. Holographic storage is one of the most promising solutions in this regard.
Holography is currently facing challenges in finding the right “medium” to capture holograms. Failure of a well-accepted standard for recording holograms is another issue. With advances in the realm of material science this problem can be overcome.14,21,22
Image display
The use of holographic displays in radiology is still in research, but they can soon find their way into commercial use and become economically viable.23 A holographic screen can be created using a specially coated glass media for the projection surface of a video projector, therefore creating a free-space display, as the image bearer appears very transparent. In addition, by controlling the beam with special lenses, the image can be made to appear to be floating in front of or behind the glass, rather than directly on it. These views can be particularly advantageous in radiology, as computers will send the 3D CT data to a projector, which will beam it to a computer screen. The radiologist, by touching the screen, will create a series of electrical impulses which will be sent to the computer. The computer will interpret the signal and modulate the projected image according to the information, thereby eliminating the use of the mouse. Furthermore, 3D reconstruction of 2D images from sectional imaging can lead to detailed 3D models of body structures, which can then be holographically displayed. This approach may be especially useful to surgeons, who are not used to viewing the body in sectional images, thus helping them in planning different approaches to, and guiding interventions during, surgery.
Holographic displays are presently insufficient with respect to giving good spatial resolution for general radiological interpretation. However, holography as a novel idea has been tried with very encouraging results in various other medical applications, such as echocardiography,24 guided invasive procedures,25 depicting pelvic fractures,26 measurement of motion of the tympanic membrane,27 depiction of bone fractures28 and forensics.29 Recently developed display technology is now able to project 3D images in free space, with the ability of the clinician to reach into the object to manipulate and apply markings to it.30
Limitations of holography
The current limitations of holography are fairly significant. Holography requires relatively complicated methods to record holographic images, making them costly and less accessible. Further, displaying holographic images requires elaborate machinery. Currently, holographic display technology lies far behind commercially available 2D and 3D displays. The most advanced volumetric displays currently have very poor spatial resolution, and can display images at only about two frames per second. Significant research is required to improve these displays to make them truly useful to the practicing doctor rather than the novel technological preview which they are currently.
Holographic images are also inherently poor at visualizing subtle tissue contrast differences. They are thus more useful at showing areas of interest to people unfamiliar with radiological sectional images than for actual radiological diagnosis.
Storage solutions based on holography are facing significant challenges at bringing the technology into the market. A significant problem in holographic recording is destructive readout. In the process of accessing the holographic data, the reading laser disturbs the recording in a way that leads to its gradual erasure. Another challenge is growing crystals with the required optical quality at sufficient speeds to enable widespread application of the technology. Such challenges have limited the adoption of holographic storage, despite significant research into the field in the 1970s.31
Conclusion
Holography has the potential to transform radiology and make it truly virtual. It can provide radiologists with the freedom to take radiology workflow beyond the high-resolution monitors into free space. It can also potentially help radiologists abandon the usual 2D workflow of a conventional monitor and mouse to process the images, thereby changing the ergonomics of radiology practice. Radiology reports can become more informative as the associations between complex lesions and adjacent vessels can be studied in their true dimensions. Holography can help address the complex issue of image storage and retrieval. As imaging databases increase, the available electronic storage within hospitals will be more rapidly depleted, requiring significant costs to maintain adequate memory capacity. Holographic storage media can provide a cost-efficient bridge to maintain vast amounts of information until the next major leap in memory technology.
References
- Tung H. Jeong. Basic principles and applications of holography. Lake Forest College, Lake Forest Illinois. https://spie.org/Documents/Publications/00%20STEP%20Module%2010.pdf. Accessed Nov. 30, 2016.
- Hunziker P, Smith S, Scherrer-Crosbie M, et al. Dynamic holographic imaging of the beating human heart. Circulation. 1999(5); 99:1-6.
- The Nobel Prize in physics 1971. Available from: http://www.nobelprize.org/nobel_prizes/physics/laureates/1971. Accessed Nov. 30, 2016.
- Gabor D. A new microscopic principle. Nature. 1948; 161(4098): 777-778.
- Blanche PA, Bablumian A, Voorakaranam R, et al. Holographic three-dimensional telepresence using large-area photorefractive polymer. Nature. 2010; 468: 80–83(letter).
- Hariharan. In: Hariharan P, ed. Optical holography: principles, techniques, and applications. 2nd ed. New York: Cambridge University Press; 1996:4-5.
- Plesniak W, Pappu R, Underkoffler J, et al. In: Benton SA, Bove VM, eds. Holographic Imaging. 1st ed. Hoboken, New Jersey: Wiley-Interscience; 2008: 207-229.
- Khan J. Biomedical imaging: 3D digital holograms visualize biomedical applications (2013). Available from: http://www.laserfocusworld.com/articles/print/volume-49/issue-07/features/biomedical-imaging-3d-digital-holograms-visualize-biomedical-applications.html. Accessed Nov. 29, 2016.
- Bjelkhagen HI, Brotherton-Ratcliff D. Ultra-realistic imaging: advanced techniques in analogue and digital color holography. Taylor & Francis Group, London. England. 2013.
- Hackett M. Medical holography for basic anatomy training. Interservice/Industry Training, Simulation, and Education Conference (I/ITSEC) 2013. Paper No. 13207.
- Buhmann JM, Malik J, Perona P. Image recognition: Visual grouping, recognition, and learning. Proc Natl Acad Sci. 1999; 96(25): 14203-14204.
- John E. Holographic technology for PACS storage: An emerging technology. Available from: http://www.eradimaging.com/site/article.cfm?ID=339#.U8yVFNyZ3oB. Accessed Nov. 29. 2016.
- Lepanto L, Para G, Aubry D, et al. Impact of PACS on dictation turnaround time and productivity. J Digit Imaging. 2006;19(1):92-97.
- Colang J, Johnston J. PACS storage technology update: holographic storage. Radiol Manage. 2006;28(3):38-46.
- InPhase Technologies. What is holographic storage? 2005. Available from: http://www.inphase-technologies.com/technology/default.asp?subn=2_1. Accessed Oct. 1, 2014.
- Nagy P, Farmer J. Demystifying data storage: archiving options for PACS. Appl Radiol. 2004; 33(5):18-22.
- Smith E. What’s in storage? ADVANCE Imaging Oncol Adm. 2004:27-30.
- Frejlich J, de Oliveira I, Arizmendi L, et al. Fixed holograms in iron-doped lithium niobate: simultaneous self-stabilized recording and compensation. Appl Opt. 2007; 46(2):227-233.
- Holographic Data Storage Technology. IBM Journal of Research and Development. 2000:44(3). doi:10.1147/rd.443.0341.
- Liu Y, Kitamura K, Ravi G, et al. Growth and two-color holographic storage properties in Mn-doped lithium niobate crystals with carrying Li/Nb ratio. J Appl Phys. 2004; 96(11):5996-6001.
- Konkachbaev AI, Elmaghraby AS. Interface for digital medical image databases. 4th International IEEE EMBS Special Topic Conference on Information Technology Applications in Biomedicine 2003. Piscataway, NJ: Computer Society Press.; 2003:238-241.
- Service R. Putting the infrared heat on X-rays. Science. 1998; 279(5347):33.
- Bove VM. Display holography’s digital second act. Proc. IEEE. 2012; 100 (4): 918–928.
- Pinto FJ, Veiga F, Lopes MG, et al. Dynamic three-dimensional echocardiography: a new era in ultrasound technology. Rev Port Cardiol. 1997;16(10):787–795; 745–746.
- Galeotti JM, Siegel M, Stetten G. Real-time tomographic holography for augmented reality. Opt Lett. 2010;35(14):2352–2354.
- Robertson DD, Sutherland CJ, Chan BW, et al. Depiction of pelvic fractures using 3D volumetric holography: comparison of plain X-ray and CT. J Comput Assist Tomogr. 1995;19(6):967–974.
- Del Socorro Hernández-Montes M, Furlong C, Rosowski JJ, et al. Optoelectronic holographic otoscope for measurement of nano-displacements in tympanic membranes. J Biomed Opt. 2009;14(3):034023.
- Robertson DD, Sutherland CJ, Chan BW, et al. Depiction of pelvic fractures using 3D volumetric holography: comparison of plain X-ray and CT. J Comput Assist Tomogr. 1995;19(6):967–974.
- Biwasaka H, Saigusa K, Aoki Y. The applicability of holography in forensic identification: a fusion of the traditional optical technique and digital technique. J Forensic Sci. 2005;50(2):393–399.
- Live 3D holographic imaging for use in interventional cardiology assessed. Available from: http://www.medimaging.net/radiography/articles/294748950/live_3d_holographic_imaging_for_use_in_interventional_cardiology_assessed.html. Accessed Nov. 30, 2016.
- Future of computing (optical & biological possibilities). Available from: http://www.doc.ic.ac.uk/~nd/surprise_97/journal/vol1/ary/#problems. Accessed Nov. 29, 2016.
Citation
AT K, R K, A S, A S.Exploring the potential use of holographic imaging in radiology. Appl Radiol. 2016; (12):19-22.
December 9, 2016