Exertional rhabdomyolysis
Images


CASE SUMMARY
A 28-year-old female presented to the emergency department with left extremity pain and swelling after recently beginning a workout regimen. She denied fever, chills, or other systemic symptoms. Her only past medical history was hypertension. Physical examination revealed swelling, warmth, and redness of the proximal left upper extremity, with no bruising or deformity. There was no loss of sensation or strength, and her pulses were palpable. Laboratory analysis revealed elevated creatine kinase of 33,912 IU/L (normal <140 IU/L) and elevated urine protein level of 100 mg/dL. The serum creatinine was normal at 0.86 mg/dL. Ultrasound of the left upper extremity veins was performed, which demonstrated no deep venous thrombosis. The patient was admitted to the hospital for intravenous hydration and observation, and MRI of the proximal left upper extremity was performed.
IMAGING FINDINGS
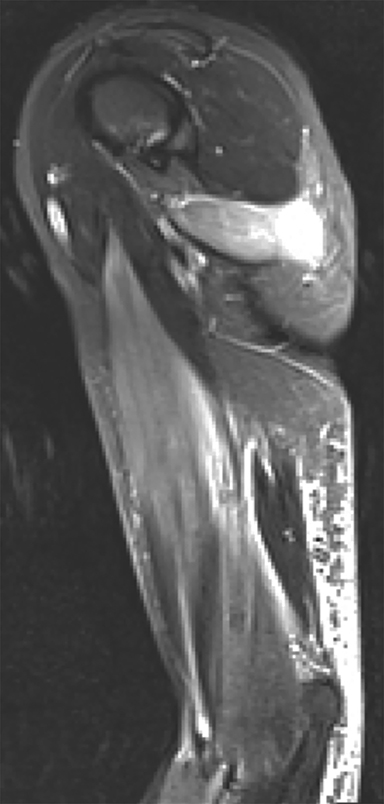
MRI of the left arm demonstrated substantial abnormal signal on STIR and PD sequences in several muscles of the left upper extremity, consistent with muscle edema. Edema was most pronounced in the teres major (Figures 1, 2), short head of the biceps brachii (Figures 1, 3) and brachialis muscles (Figure 3). The overall architecture and size of each of the muscles was preserved, and intact muscle fibers could be seen on all images. There was no discrete muscle tear or area of confluent muscle necrosis. There was no muscle atrophy or fatty infiltration on T1-weighted images.
DIAGNOSIS
Exertional rhabdomyolysis, also known as exercise-induced rhabdomyolysis. Differential diagnosis includes infectious myositis, inflammatory myositis, muscle infarction, acute denervation, and rhabdomyolysis due to other causes (eg, drug-induced, crush injury).
DISCUSSION
Rhabdomyolysis is the rapid breakdown of injured or damaged skeletal muscle.1 This results in the release of muscle breakdown products into the extracellular space and bloodstream. These muscle breakdown products include electrolytes, creatine kinase and myoglobin. Rhabdomyolysis can lead to life-threatening electrolyte imbalances and acute kidney injury that can result in chronic renal failure.
Rhabdomyolysis presents classically as myalgia, weakness and myoglobinuria, although this triad is actually seen in less than 10% of patients.1 The most sensitive laboratory test for rhabdomyolysis is serum creatine kinase (CK). A serum CK level greater than 5 times the upper limit of normal is compatible with the diagnosis of rhabdomyolysis (>975 IU/L).2 The treatment of rhabdomyolysis is largely supportive, including aggressive intravenous hydration in order to preserve renal function.
There are numerous potential causes of rhabdomyolysis, and identification of the cause is important to prevent ongoing muscle damage and disease recurrence. The most common causes of rhabdomyolysis are illicit drugs/alcohol, followed by medicinal drugs, muscle diseases, and trauma.2 Exertional rhabdomyolysis induced by excessive vigorous exercise is a relatively uncommon cause, and has been associated with football, swimming, running and military training.3 CrossFit is a branded physical fitness regimen that includes high-intensity weightlifting, calisthenics and cardiovascular exercise, often with little interval recovery time.4 This form of intense physical exercise has the capacity to result in rhabdomyolysis, as in this case.
Imaging of the affected muscles may be performed in the setting of exertional rhabdomyolysis to assess the extent of muscle involvement, and is best accomplished with MRI. The affected muscles will demonstrate diffuse edema on T2-weighted images.5 The muscles may also be enlarged, with a mild decrease in signal intensity on T1 weighted images due to edema. The muscle architecture,e will be preserved, with identification of intact muscle fibers, and no confluent areas of muscle necrosis. If contrast is administered, there will be diffuse enhancement of the affected muscles. It is important to evaluate for associated muscle and tendon tears that may require orthopedic intervention.
The appearance of muscle edema on MRI is not specific for rhabdomyolysis. Muscle edema is also seen in the settings of inflammatory muscle disease, infection, denervation, and diabetic myonecrosis, all of which can be complicated by rhabdomyolysis.6 Inflammatory muscle disease (including polymyositis, dermatomyositis and inclusion body myositis) most commonly involves the proximal upper and lower extremity muscles in a bilateral symmetric fashion. Pyomyositis will most commonly involve a single muscle or muscle group, and will demonstrate intense edema with an surrounding the muscle, often with abscess formation. Viral myositis may have a more widespread distribution of less intense muscle inflammation. Denervation edema will manifest in muscles corresponding to a particular nerve or nerve root distribution. Diabetic myonecrosis can occur in patients with poorly controlled diabetes, and will demonstrate macroscopic breakdown of the muscle architecture and areas of confluent muscle necrosis.
Delayed onset muscle soreness (DOMS) refers to muscle aching and pain that presents around 24 hours after completion of intense exercise and peaks in 1 to 3 days. DOMS also presents as muscle edema and enlargement in the affected muscle on MRI.7 While the patient may have a mild increase in creatine kinase level, the CK level will not approach that seen with rhabdomyolysis.
The diagnosis of exertional rhabdomyolysis can be made from the imaging findings in a patient with an appropriate clinical history and elevated creatine kinase. Other etiologies for muscle edema should be considered if there is no history of intense exercise or if the laboratory findings do not indicate rhabdomyolysis.
CONCLUSION
Exertional rhabdomyolysis can occur following intense physical exercise (CrossFit in this case). The laboratory gold standard for the diagnosis of rhabdomyolysis is an elevated plasma creatine kinase (CK) level. The clinical history of vigorous activity and elevated plasma CK level are very helpful to the imaging diagnosis. MRI will demonstrate edema throughout the affected muscles. The most serious complication of rhabdomyolysis is acute kidney injury, which is managed by aggressive intravenous hydration. Prompt diagnosis and management of rhabdomyolysis is crucial to prevent severe kidney injury and chronic renal disease.
REFERENCES
- Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: Pathogenesis, diagnosis, and treatment. The Ochsner Journal. 2015; 15:58-69.
- Chaudhry V, Cornblath DR. Rhabdomyolysis: An evaluation of 475 hospitalized patients. Medicine. 2005; 84:377-385.
- Tietze DC, Borchers J. Exertional rhabdomyolysis in the athlete: A clinical review. Sports Health. 2014; 6:336-339.
- Meyer M, Sundaram S, Schafhalter-Zoppoth I. Exertional and CrossFit-Induced Rhabdomyolysis. Clin J Sport Med. 2017 doi: 10.1097/JSM.0000000000000480.
- Moratalla MB, Braun P, Fornas GM. Importance of MRI in the diagnosis and treatment of rhabdomyolysis. Eur J Radiol. 2008; 65:311-315.
- May DA, Disler DG, Jones EA, et al. Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics. 2000; 20: S295-315.
- Agten CA, Buck FM, Dyer L, et al. Delayed-Onset Muscle Soreness: Temporal Assessment With Quantitative MRI and Shear-Wave Ultrasound Elastography. Am J Roentgenol. 2017; 208:402-412.
Citation
RW M, MC J.Exertional rhabdomyolysis. Appl Radiol. 2019; (4):36-37.
July 18, 2019