Evolving Technology: Distributed Diagnosis
Dr. Siegel is a Professor of Diagnostic Radiology and the Radiology Associate Vice Chairman for Informatics, Diagnostic Imaging, University of Maryland Medical Center, and the Director, Baltimore Veterans Affairs Medical Center, Baltimore, MD. He is also a member of the editorial board of Applied Radiology.
As the Chief of the first filmless hospital in the United States, I have been asked many times about our motivation, goals, and objectives when we made the decision in 1989 to build a new hospital and radiology department without film. In addition to the allure of the cutting-edge technology and potential to improve image quality, a major goal was to eliminate lost film. In fact, the Chairman of Medicine made the cheeky observation after we went filmless in 1993 that the Baltimore VA �has always been filmless, because you could never find any of your films.� However, our most important goal in the transition from analog to digital was to use the PACS to reinvent our workflow.
In 1989, we performed a study with the help of an engineering firm that documented the 59 steps required to order, perform, report, and review an inpatient chest radiograph. The transition to filmless operation with a commercial PACS eliminated only 11 of those steps. We analyzed the results and concluded that, in order to achieve maximum efficiency and productivity, we would need to use the PACS as a tool to re-engineer our workflow rather than merely as a substitute for film. We were able to do this with a variety of different approaches, including eliminating paper by using a radiologist-specific PACSworklist, integrating our PACS with the hospital and radiology information systems, using the DICOM modality worklist capability to allow the automatictransfer of patient information to our imaging modalities, and, more recently, by making the transition to a speech recognition system. This has allowed us to eliminate all but 8 steps of our original 59 and to achieve substantial gains in radiologist and technologist productivity and elimination or redeploymentof the majority of our clerical and film room personnel.
Despite our success with integration and workflow optimization within our own enterprise, our faculty practice, which covers multiple inpatient and outpatient facilities in addition to the VA and University of Maryland Medical System, has been increasingly challenged by the inefficiencies inherent to a geographically disseminated practice that uses multiple PACS, hospital and radiology information, and reporting systems. We have struggled to find solutionsthat address our need to use multiple applications on different workstations for our daily tasks as radiologists, our need for multiple worklists, the limitations of bandwidth across our practice, and other related issues.
In this supplement, Dr. Sean Casey, CEO of Virtual Radiologic Corp., discusses the importance of workflow analysis and optimization in a distributed practice and 8 pitfalls that can impair a practice�s efficiency. His widely distributed practice, like those of other large distributed groups, has worked very hard to address and overcome these issues that are especially critical to the success of a teleradiology company. His advice applies, however, not only to teleradiology practices but also to the majority of current radiology practices that now have multiple information systems spread across multiple locations.
Dr. Howard Kessler, Director of Technology Development and Chief Operating Officer of Radiology Solutions, discusses the technology, but also the philosophic, business, and socioeconomic aspects and the potential associated with a distributed imaging practice. He also addresses the benefits of such a practice and lists the risks associated with implementing a distributed imaging system. Finally, Dr. Kessler provides practical advice and questions to consider when planningto expand a practice�s services.
Dr. Casey is the CEO and Co-Founder of Virtual Radiologic Corporation, Minnetonka, MN.
While most radiologists today have made the transition from ï¬lm-based analog interpretations to digital interpretations using a picture archiving communication system (PACS), most of us are still remarkably far from reaping the potential efï¬ciency beneï¬ts of this digital transition. Some may even ï¬nd themselves in a less efï¬cient practice environment than in the ��good old days�� of ï¬lm-based reads. Back in those days, analog reading workï¬'ows had evolved to maximum efï¬ciencies over a period of several decades. While great technology advances have been made over the past decade with the widespread introduction of PACS, radiology information systems (RIS), and voice recognition, there has, unfortunately, been much less thought put into developing efï¬cient digital workï¬'ows. Many of us actually faced a setback in efï¬ciency when we transitioned to the use of PACS and/or voice recognition.
Case volumes are growing yearly because of the aging population and the advancement of imaging technologies. Declining per-study reimbursements require efï¬ciency gains to make up the per-unit losses with higher volume. In order for a practice to succeed in recruit-ment and retention, salaries must be competitive. If the workï¬'ow is not efï¬cient, a practice will have trouble maintaining market-competitive radiologist salaries.
Workï¬'ow is driven by worklists
In order to address deï¬ciencies, it is important to analyze what is driving the workï¬'ow in a given practice. Typically, this is obvious from the main worklist used by the practice to choose the next case. Practices generally fall into several categories of workï¬'ow:
PACS-centric workï¬'ow : Radiologists work primarily from the PACS worklist.
RIS-centric workï¬'ow: Radiologists work primarily from the RIS worklist.
Dictation-centric workï¬'ow: Radiologists work primarily from the voice-recognition system worklist.
Each of these workï¬'ows has its loyal supporters. The problem with these conventional workï¬'ows is that they are typically driven by ��dumb�� worklists. These are retrospectively and passively sorted lists that are prioritized by time, modality, location, or a combination of these factors. The main problem with these worklists is that they do not offer real-time feedback and, as such, concepts such as active load balancing of studies and prioritization of cases according to speciï¬c turnaround time (TAT) needs are not considered. Because of these inï¬'exibilities and a lack of systems integration, many practices actually continue to work from paper lists.
Paper-based workï¬'ow
Despite having successfully made the transition from analog ï¬lm-based reading to digital PACS-based reading, many practices persist in using stacks of papers as their worklists. These are typically control sheets printed from the RIS. For teleradiology practices, these are typically stacks of inbound fax orders. The appeal of the paper worklist is that it can be shufï¬'ed in a much more ï¬'exible fashion than most dumb digital worklists. Emergency cases can easily be pulled right to the top of the stack. Furthermore, a barcode on the sheet can overcome the lack of system integration: it serves as an analog-to-digital interface between the PACS, RIS, and dictation system. Problems occur when the stack of papers is too large to divide among a sizable practice across multiple facilities. Furthermore, sheets are prone to being lost, and the TAT on the case could be severely delayed.
Custom workï¬'ow driven by a workï¬'ow engine software
A new type of customizable worklist is the workï¬'ow engine. This takes into account the unique requirements of a practice, including multiple-case TAT requirements, various subspecialty assignments, and the overall size of the group. This software can be built into the PACS, the RIS, or the dictation system but can also exist as an independent software application. One can think of it as yet another work-list, but it is an active real-time worklist that is focused only on workï¬'ow. It drives case assignments on the basis of many factors such as license, credentials, subspecialty, TAT requirements of the case, and load balancing of workloads across radiologists in the practice. Assignment by license and credential is particularly critical to a multistate teleradiology practice as a protection against radiologists doing unauthorized interpretations. Each radiologist can actually have an individual worklist, which, on a Web-based system, will be available wherever he or she chooses to read. As compared with a passive worklist that changes only as new patients are added or as existing cases are read, an active worklist on a workï¬'ow engine can dynamically rearrange the assignments of cases to a given radiologist; eg, an emergency brain MRI will go to the top of the neuroradiologist��s worklist even if older, but less critical, cases are present.
Eight imaging workï¬'ow pitfalls
Regardless of which type of worklist your practice uses, you will improve your workï¬'ows by avoiding as many of the following pitfalls to efï¬cient workï¬'ow as possible.
1.The ��dumb�� worklist
The use of a dumb worklist results in frequent interruptions and radiologist cherry-picking. The nonprioritization of cases by TAT on a nonintelligent worklist or the loss of cases (due to accidental sign-off on a digital worklist or a lost sheet on a paper worklist) results in a greater chance of an interruption, such as a clinician inquiry.
Furthermore, the simplest of the dumb worklists (such as used on a PACS) allows for radiologists to arbitrarily choose whichever cases they will read. Nearly all currently used worklists allow radiologists to jump ahead to grab cases out of order. When this is done for self-serving reasons, such as to skip a difï¬cult case or to grab an easy case, it is called cherry-picking. The downsides of cherry-picking are obvious: this is antiteam behavior that dumps work on one��s colleagues, and it hurts patient care by delaying the TAT on complex cases.
While some cherry-picking probably exists to various degrees in any mid-size to large practice, distributed practices are even more prone to this workï¬'ow vice, as it cannot be policed merely by a disapproving stare from across the reading room.
Furthermore, a dumb worklist may assign cases to a single radiologist in a single location, and then case turnaround performance will be dependent on that radiologist��s availability. If the chosen radiologist is busy doing a procedure or is on a lunch break, the TAT on the case will be delayed. Load balancing across radiologists and locations accesses a larger pool of potential readers and eliminates dependence on the availability of a single radiologist.
Many radiologists perform teleradiology with case assignments on older-architecture point-to-point digital imaging and communications in medicine (DICOM) teleradiology systems, and this limits the ability to load balance studies across multiple radiologists and multiple locations. More modern Web server architectures tend to better support such load balancing, as they permit simultaneous downloads to multiple locations and radiologists.
The best way to avoid the pitfall of the dumb worklist is to switch to a workï¬'ow driven by an intelligent worklist, which will minimize interruptions and cherry-picking and will allow load balancing to provide the greatest consistency of TAT performance.
2. Vision-dependent workï¬'ow navigation
This is a very common pitfall. It is perhaps often overlooked because it costs only a second here and a second there. But if you add up the seconds over the entire work day, and it amounts to real time and resistance to stress-free workï¬'ow.
This should be a very simple concept: since image interpretation can be condensed down to the radiologist looking at images, anything that requires the radiologist to remove his or her eyes from the PACS images is potentially unnecessary and thus a potential impairment to workï¬'ow efï¬ciency. The common culprits that require the radiologist to remove his or her focus from the PACS images are: worklists, computer menus, toolbar icons, keyboards, and dictation screens. Ideally, a radiologist should use as much ��eyes-free�� navigation of the reading platform as possible. If possible, right-click mouse menus and toolbars should be avoided in favor of keyboard shortcuts, especially if they can be mapped to supplementary mouse buttons or some other human interface device (such as a dictation microphone, grip, jog dial, or foot pedals). Nearly every common PACS function should be able to be navigated while dictating, without having to stop scrolling or to take one��s eyes off the images. Furthermore, it is ideal to minimize the time spent looking at the voice-recognition screen.
3. Comparison cases on ï¬lm or disk
One of the most frustrating experiences in workï¬'ow is having to compare a case on your current PACS with the patient��s relevant prior examination on ï¬lm, on an older PACS system, or on an outside CD/DVD. This entails mental and physical strain, since the light-box or accessory viewing monitor is often not within easy reach. Furthermore, the controls on the viewer from the external CD/DVD are likely unfamiliar and frustrating to use.
To avoid this pitfall, the ï¬lms or old PACS data can be imported into the new PACS system, but this is certainly an added cost. One can consider building an old case archive within the new PACS over a period of time before going live with the new system. Ideally, external CD/DVD data should be able to be imported into the PACS system. This is particularly important in a distributed practice, in which it helps to avoid shipping ï¬lms and disks between reading sites. Unfortunately, some systems are not ï¬'exible enough to allow this without risking data corruptions, and, furthermore, some of the CD/DVD cases are not in an importable DICOMDIR format.
4. Working from multiple worklists on multiple computers
Although every practice has to choose a primary worklist from which to drive its workï¬'ow, many practices persist in the use of multiple worklists because of the lack of integration among applications. Ideally, the primary worklist is all that is needed. It should launch the PACS images and open the RIS study information and the dictation window.
The use of ��2 computers creates user confusion, as the radiologist typically needs to shift back and forth between multiple keyboards and multiple mice. To get past this mess, a practice needs to achieve not only desktop-level integration but also application-level integration.
Desktop-level integration�� Desktop-level integration gets all of a radiologist��s work applications onto a single computer (although it can still have multiple viewing monitors).
Application-level integration�� Application-level integration is an even higher level of integration that gets the individual software applications (such as the PACS, the RIS, and the dictation system) to behave as a single functional unit on 1 computer. This level of integration results in a single worklist that launches all of the software components needed for case viewing and dictation. There is no need to select patients from separate worklists, and this eliminates the risk of human error in selecting a wrong patient match on the secondary worklist. Integration of PACS, RIS, and dictation systems is one of the biggest safety improvements that informatics can contribute to radiology.
Such levels of integration are perhaps easier said than done. Unfortunately, PACS�CRIS integration may require cooperation between competing software vendors. More modern Web-based PACS systems tend to make integration easier by means of URL integration: the PACS images can be launched by any worklist that is able to predict the Web address of the images from the known patient demographics.
5. Inadequate bandwidth, network bottlenecks, and/or poor caching
Many hospitals have an inadequate hosting environment or suboptimal connections to the Internet. Applications hosted on servers from within the hospital or within its data center might work ï¬ne within the hospital local-area network (LAN) but often are suboptimal for use over a wide-area network (WAN) such as the Internet. Many hospitals have low-capacity encryption devices (virtual private networks [VPNs] or Secure Sockets Layer [SSL] accelerators), which essentially place a cap on the available bandwidth to those outside the ï¬rewall. Do not skimp on information technology (IT) hardware and bandwidth. You will pay the price in radiologist efï¬ciency.
It is amazing how tolerant radiologists can be when using teleradiology systems. On the old telephone-based teleradiology systems, radiologists became accustomed to waiting for cases to download. In the modern era, it should be unacceptable for a radiologist to have to wait for data to transmit after a case is launched. All data transfers should occur before the case is viewed. Such predelivery of data is termed caching or precaching . Certainly, even over high-speed Internet connections, cases take time to transmit, especially in the era of large multidetector CT studies. If a workï¬'ow engine can predict the cases that are the next most likely to be viewed, however, then all of the transfer time can occur in the background while the radiologist is reading the current case. On a well-designed system, the radiologist should perceive no performance degradation or delay between cases when using a PACS onsite on the LAN versus using the same PACS as a teleradiology system over the Internet. On a poorly designed system, one can wait seconds to minutes between cases for data to download. If this takes 2 minutes on average per case, over a 120-case workload, this will add up to 4 hours of wasted time! Poor bandwidth or poor caching impairs efï¬ciency and can destroy the economics of a distributed practice.
6. Multiple disparate PACS, RIS, and dictation systems in multiple locations
This problem plagues mid-size to large groups with multiple locations. Often, the locations are not part of the same healthcare system and do not use the same brand of software applications. As such, these groups work from multiple different workï¬'ows, which is inherently inefï¬cient.
Each system comes with a different workï¬'ow along with a different username and password (and these change at all too frequent intervals). Each different brand of system has its own unique software user interface. Not all PACS even use the same keyboard shortcuts or navigational controls. As such, when rotating to a new facility, radiologists spend some time working at a lower efï¬ciency because they are not familiar with the system.
In a distributed practice, it is challenging to work on multiple different systems. This can result in radiologists working in a ��war room���Clike environment that is ï¬lled with computers among which they need to rotate to do their reads. At best, these practices use a paper worklist composed of faxes. At worst, they don��t have a real master worklist between applications and instead work on individual disjointed worklists.
The conventional alternative is even worse: driving between facilities or working in isolation from the rest of the group in a single facility. This results in wasteful travel time, poor ability to balance workloads, and poor degrees of subspecialization and intrapractice consultations, even for large groups.
Such a heterogeneous set of workï¬'ows is not scalable as a practice grows. If your group wishes to grow and to improve efï¬ciency, it is critical to minimize the number of different systems from which you read. While it might not be possible to remove the multiple systems on which the afï¬liated hospitals depend, it is possible to aggregate one��s work (or at least one��s interfacility load-balancing work) across your facilities onto a single reading platform. Such a reading platform can be the one and only reading platform for a practice that overlies all of the heterogeneous facility systems. In this way, a distributed practice can use a single worklist to drive a uniï¬ed workï¬'ow.
7. Physicians performing nonphysician work
To improve workï¬'ow, it is critical that doctors not perform nonphysician work. In any organization, the staff member who is paid the most should be limited to doing what only he or she can do. Radiologists are more expensive than phone operators; therefore, radiologists should not be working the phones. They should indeed be available for phone consultation but should not be trying to track the whereabouts or phone numbers of the ordering or on-call clinician. Most radiologists can interpret a head CT faster than they can manually fax its report! Radiologists are more expensive than automated fax servers and should not waste time operating fax machines.
One of the most common causes of malpractice suits involves the miscommunication of results��particularly the failure to notify clinicians of important ï¬ndings. In a typical practice, a radiologist might waste precious time trying to track down a clinician. Such nonphysician work can be an obstacle course that frustrates and distracts the radiologist. After multiple attempts, a radiologist might forget about the notiï¬cation task altogether. This can inadvertently lead to serious patient care issues.
In my practice, we have set up a call center whose staff does the behind-the-scenes, nonphysician work of tracking down clinicians and technologists. Furthermore, we have built its functionality into our workï¬'ow engine/reporting software. Once a radiologist sees a critical ï¬nding on an image, a single mouse-click can trigger a critical-ï¬nding call request to our call center. The exact time of the request is stored in our software as an audit trail. As soon as the clinician is located and on the phone line, the radiologist is connected to the phone call. Removing this nonphysician receptionist activity allows a radiologist to stay focused on what he or she does best: reading images. This type of system can be a major efï¬ciency gain for almost every practice.
8. Outdated, nonupdatable systems
This problem is created by legacy systems that required substantial up-front capital to install but then remain relatively stagnant throughout their life cycle. A hospital will seek a return on investment (ROI) on the software and likely will not have planned for major software upgrades in its tight annual budget. As a result, a practice may be stuck with outdated software for years even if the larger multidetector data sets are already bringing it to its knees.
This is perhaps the most serious workï¬'ow problem, since it limits a practice��s ability to maintain state-of-the-art technology. Unless it is possible to customize or integrate the existing applications, a practice is relatively powerless to improve its workï¬'ows.
Improvements to efï¬ciency via a distributed reading platform
One way to escape most, if not all, of these workï¬'ow traps, is to consider investing in an overlying distributed reading platform. Fortunately, such Web-based systems are more affordable than the legacy systems with their old school ��big iron�� workstations. Application Service Provider (ASP) and Software as a Service (SaaS) offerings allow you to avoid large upfront capital purchases and are typically available for a subscription or per-case fee. These systems are usually hosted by the software provider, which saves signiï¬cant data center and IT personnel costs. Instead, these costs are shared across the customer base, and your share is charged to you within the subscription fee. Such software is integrated, deployed, and frequently updated over the Internet such that it is always state of the art. It runs on inexpensive PC hardware.
Load balancing in a distributed practice
A distributed reading platform can provide an intelligent worklist, which will be able to determine the ideal reader for a given case at any moment in time. Such an intelligent worklist assigns cases to radiologists on the basis of the radiologist��s credentials, subspecialty, and current workload. This case assignment feature serves to load balance studies across multiple radiologists and facilities. For example, if all other factors are equal, a simple case assignment algorithm will give a new case to the radiologist with the shortest worklist. This tends to prevent situations in which one radiologist is bogged down with a large worklist while another may have an empty list with no work to perform.
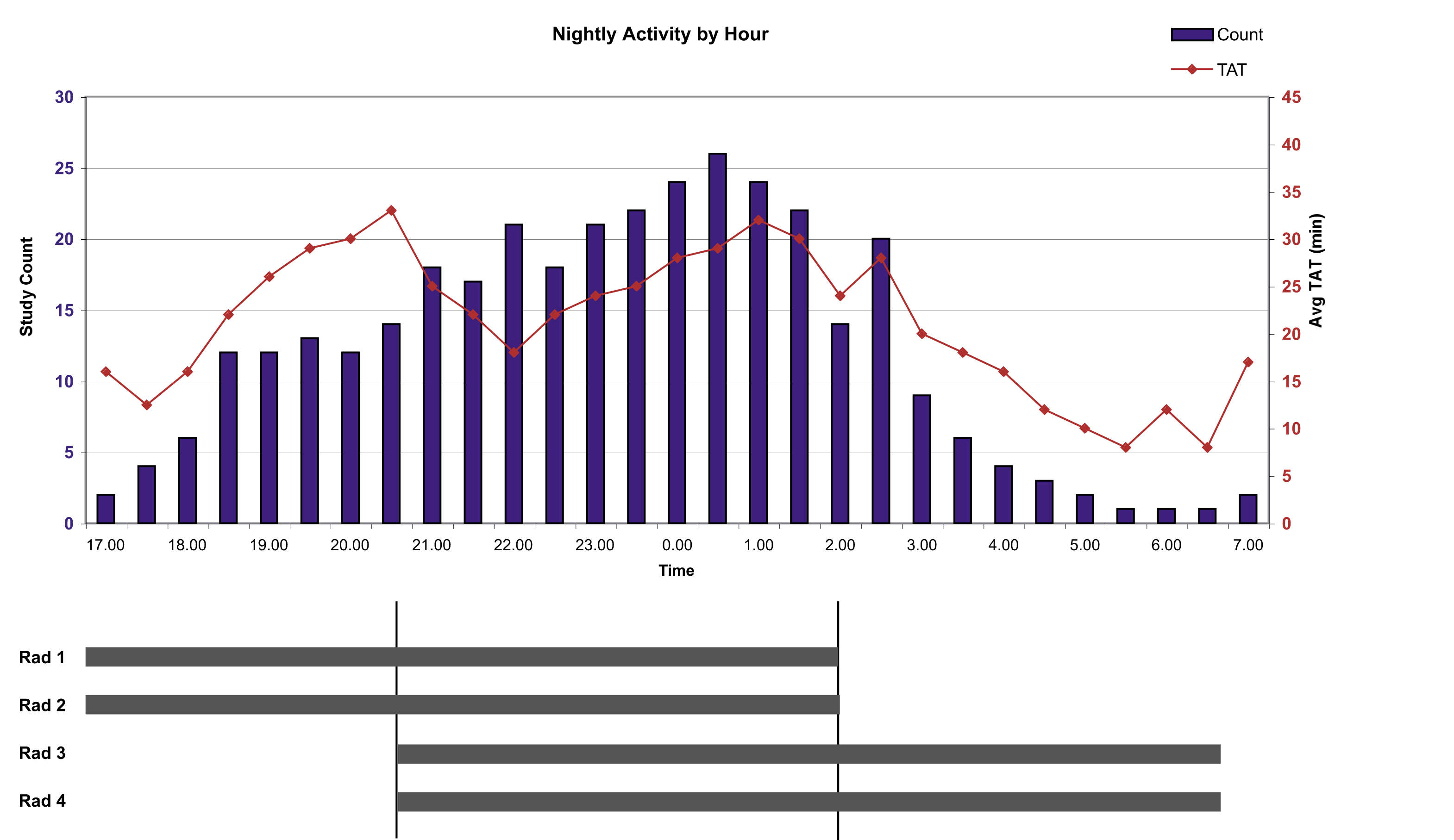
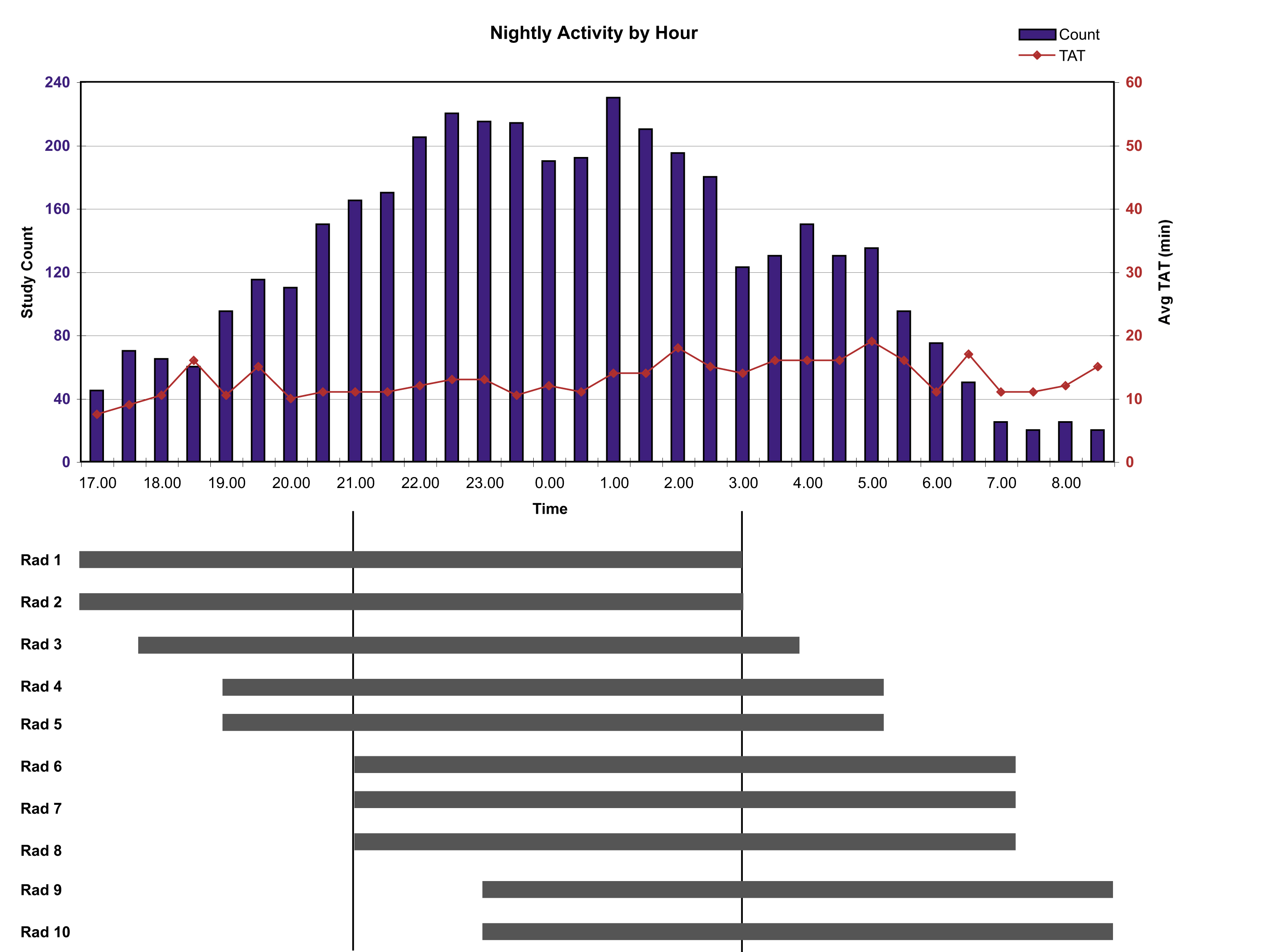
A larger distributed practice can better take advantage of load balancing across its reading locations while also leveraging overlapping shifts to maintain the greatest consistency of TATs. In a non-distributed smaller practice, there is no load balancing across facilities, and thus there is limited ability to leverage overlapping shifts. The level stafï¬ng of such a facility during a shift results in TATs that are relatively proportional to the hourly case volume at any given hour. The smaller the practice, the more the case TAT is held hostage to the health, availability, and mood of a single radiologist. In larger practices, variances in daily performance or the availability of radiologists will tend to be masked by the overall pool of radiologist capacity. In my own practice, we have made great improvements in the consistency of our TAT by leveraging the entire size of the distributed practice with load balancing and overlapping shifts (Figures 1 and 2).
Conclusion
Because attention has not been paid to workï¬'ow, the expected efï¬ciency gains of the digital era have not yet been fully delivered to radiologists. Analyzing a practice��s workï¬'ow and avoiding a host of workï¬'ow pitfalls can provide signiï¬cant improvements in efï¬ciency. Most of the solutions to the pitfalls require investment in upgraded or new systems, custom integrations, or IT infrastructure. Given that the legacy systems that force the workï¬'ow pitfalls upon radiologists are provided by facilities to radiology groups for ��free,�� there is an expected reluctance to invest in an IT infrastructure or a common reading platform for a practice. What is often overlooked is that there is a cost to the ��free�� legacy software that is paid dearly with decreased radiologist productivity. Major efï¬ciency gains among your practice��s radiologists can not only pay for the new distributed workï¬'ow technologies but can also be your best way to defend against the never-ending trend of declining reimbursements.
Dr. Kessler is the Director of Technology Development and Chief Operating Ofï¬cer, Radiology Solutions, Wayne, PA.
The world hates change, yet it is the only thing that has brought progress.
Charles Kettering (1876�C1958)
In diagnostic imaging, distributed diagnosis is the prospective allocation of imaging studies from a central location (hospital, imaging center) to radiologists with requisite training and expertise to interpret the examination. The best example is the outsourcing of studies by modality (eg, MRI, CT) or body system (eg, orthopedics, central nervous system) to those best qualified to interpret the examination by virtue of training and/or experience.
Technology: Which tools are available?
The availability of low-cost, high-speed Internet access has created an affordable infrastructure on which large data sets composed of digital imaging and communications in medicine (DICOM) images (radiology studies and the accompanying relevant information) can move from a local-area network (LAN) to a more disseminated audience on a wide-area network (WAN).
The development of affordable picture archiving and communication systems (PACS) has further reduced the cost of implementing distributed diagnosis. Presently, there are scores of small companies providing off-site preliminary and final reads, and there is a general acceptance among radiology groups, imaging centers, and hospitals that the future of professional radiology service will likely be based on off-site interpretation of studies.
Inherent in the process are standards to exchange medical information through secure WANs. The universal standard commonly used to communicate medical healthcare-related transactions within a medical enterprise, Health Level 7 (HL7) comprises one of the necessary bridges to move information from a hospital or imaging center enterprise to remote sites. DICOM represents a standard for the communication and archival of medical images and related information about an imaging study such as slice thickness, imaging modality, and imaging technique. Using these standards, an off-site interpreting radiologist has access to the same information that was previously confined to a LAN in the pre-PACS era when vendors used proprietary methods to exchange image and patient information.
The role of speech recognition
Speech recognition has emerged as a powerful tool in the armamentarium of radiologists, regardless of practicing venue. Originally confined to a local venue, thin-client solutions permit radiologists to create an immediate interpretation remotely while making the report available to all persons authorized to access it with status updates and allow the report itself to be communicated from the speech recognition server to a radiology and/or hospital information system using the HL7 standard. The obvious advantage is the ability for immediate receipt of results upon completion of the interpretation into the radiology information system and instantaneous dissemination of a finalized report to healthcare professionals.
Changes in radiology practices
Why the sudden push toward technology as an enabling device for change in the existing model for the provision of radiology services? At various levels within the healthcare system, there is an understanding that the present system of providing care is both inefficient andcostly. Radiology practice today exemplifies both the dilemma and the opportunity. The growth of imaging procedures is far exceeding thecapacity to render meaningful and timely diagnosis. There are many factors contributing to this:
- Growth in indications for a given technology;
- The complexity of the procedures and increasing size of data sets to be analyzed; and
- Aging population consuming an in creasing share of medical imaging resources.
Once the technology hurdles were overcome, the next piece to fall into place was the professional component. This appears to be a work-in-progress; however, there are clearly evolving trends in the direction of virtual radiologists operating in nontraditional venues.Flexibility in hours and life-style issues has created opportunities for distributed diagnosis. Increasingly, independent contractors are available to provide services outside the confines of the traditional hospital-based, partnership-track radiology practices.
Directed diagnosis: Business and practical aspects
At the practice level, a fundamental shift is required prior to implementing the concept of distributed diagnosis. Practices must recognize both the need and the value of the proposition. Although well intentioned, many of these practices fail to grasp the rudimentary concepts of the business of directing imaging studies to those best qualified to interpret the examination. Acceptance of the concept is the first step. The potential of distributed interpretation to achieve higher-quality interpretations and faster turnaround time must strike a resonant chord withthe practice. Although the initial costs of implementing distributed diagnosis are reasonable and the impetus may be one of necessity rather than profitability, there are many factors to consider prior to committing to the concept.
What are the benefits of distributed diagnosis and who are the beneficiaries?
The benefits of distributed diagnosis accrue to the stakeholders in the process. Patients benefit from dissemination of case work to the radiologists who are best qualified to interpret a case regardless of the type of examination. For example, a case could be sent to a reader with expertise in the orthopedic imaging of the central and peripheral nervous system, if that is appropriate to the case. Alternatively, the same case could be sent to a radiologist with an expertise in the particular modality in which the study was performed (eg, ultrasound, nuclear medicine, and positron emission tomography). Practices and hospitals must decide which is the better of the 2 routes. Hospitals and practices benefit from higher-quality care and service, improved turnaround times, access to higher-quality interpretations, and a decline in ordering and performing additional studies because of improper or conjectural interpretations. Referring physicians benefit from higher-quality interpretations, easing the diagnosis and treatment of disease.
There is a continuum of beneficiaries from a financial perspective as well. These extend from those who pay for care to those who receive care. For example, at the payor level, higher-quality interpretations provide a more accurate diagnosis, fewer ambiguous reports, fewer recommendations for alternative imaging to resolve a clinical dilemma, and fewer follow-up examinations. The distribution of work to those best qualified to interpret studies is consistent with Medicare initiatives that are generally referred to as pay-for-performance. There is a downstream effect to those who embrace this methodology, including patients and referring and consulting physicians.
Radiologists benefit from the implementation of distributed diagnosis at several levels. They can maintain good relationships with the providers of imaging services and improve relations that may have suffered as a result of suboptimal service (poor turnaround time), suboptimal quality (based on study interpretation from less-qualified radiologists), or the inability to match enterprise growth into new programs or modalities). Protection of turf can be eased when the full armamentarium of imaging services is matched to the radiologists who are interpreting studies.
On an ongoing basis, there is value in a flexible employment opportunity. This type of candidate includes radiologists on personal or medical leave, those responsible for the care of family members, those looking for life-style changes that might come about because of the venue where work is performed and the flexibility of work hours, and those who desire the virtual-style practice of a locum tenens.
Within the radiology group, at the level of the individual physician, interpreting physicians may benefit from this model, provided there are incentive-based compensation models that reward high-quality services, rapid turnaround, and high productivity. If there is consensus that change is inevitable and that the future of radiology is based, in part, on leveraging technology as an enabling agent, those who fail to take advantage are at risk.
What are the risks of implementing distributed diagnosis?
Practices may be at increasing risk if they cannot provide the service commensurate with contractual obligations and expectations madepossible by distributed diagnosis. The technology necessary to provide distributed diagnosis for the benefit of the radiology practice could alternatively be used by the hospital to contract with other providers if services and obligations cannot be met under the existing traditional contract model. The factors required for a successful local practice may be different from those required to manage a distributed process,including different strategies for communication and flexibility in scheduling. A more sophisticated information technology (IT) infrastructure is required for a distributed diagnostic imaging practice that may be of a higher level of sophistication than the current IT personnel can provide and may be substantially more expensive and resource-intensive.
The prerequisites for establishing a distributed diagnosis program include the following:
- Within the existing practice, there is value in directing work to the radiologist who is best qualified to interpret the study.
- The cost of entry can be readily absorbed or budgeted for.
- The technology exists within the practice to provide directed interpretations with a cost-efficient model.
- Tools exist within the practice to improve efficiency and productivity.
- It is possible to assess the cost savings provided by and the profitability of the use of off-site radiology services.
- Business enterprises that will provide the off-site services (acute care facilities, imaging centers) understand the concept and a rereceptive to the model.
- There is an identified market for radiologists who are interested in providing off-site reads, whether through employment or independent-contractor models.
Conversion from traditional to technology-enabled practice
Converting from a traditional practice requires organization and a methodology for assessing the needs and understanding the capabilities and limitations of existing technology and workflow. There are conceptual considerations:
- Is there a need within my practice?
- Can my practice arrive at consensus on the concept?
- How do I organize existing re sources to assess and implement technology and to ensure ongoing operations?
- Is this a necessity or merely a diversion of time and resources?
- Is the model designed for growth based on the needs of the existing practice?
- Is the model configured for growth in new opportunities?
- What is the triggering event?
- Is the impetus based on failed recruitment and retention initiatives?
- What are the roles of employees, partners, and independent contractors willing to provide services?
Conclusion
The concept of distributed diagnosis is, in some ways, the Holy Grail of radiology, and the challenges are both philosophicand practical. Technology exists to support the collection and subsequent dissemination of diagnostic imaging studies. Understanding the benefits at multiple levels is a prerequisite. A commitment to quality represents the foundation on which tobuild in a process that should be considered to be evolutionary. The starting points for practices are variable; however, they can be distilled to the challenge to leverage technology to improve efficiencies while providing the highest quality of care attainable.
