Evaluating a 3D ultrasound imaging scoliosis assessment system
Children with adolescent idiopathic scoliosis (AIS) undergo repeated x-ray exams to monitor their condition. Repeated radiation exposure from radiographs has been shown that the risk of these young patients developing breast cancer, prostate cancer, and leukemia later in adulthood increases. Imaging systems using 3D ultrasound technology are being developed to provide a radiation-free alternative.
One 3D ultrasound imaging system in commercial development is the Scolioscan (Talefield Medical Imaging, Hong Kong, China). The system that consists of an ultrasound scanner with a linear probe, a frame structure, an electromagnetic spatial sensing device. It utilizes proprietary software for image acquisition, data collection, analysis, and assessment. It is designed to accurately assess scoliosis in three dimensions. The system can assess a patient’s spine in the standing posture and generate coronal images of spinal curvature for measurement to determine the severity of the scoliosis. The technology captures the spine’s 3D profile using identified bony landmarks to measure spinal rotation and deformity along different planes.
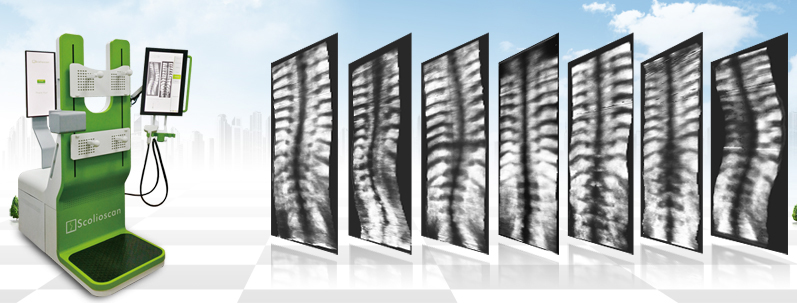
Scolioscan and typical VPI images with spine with different deformities.
Researchers at the Hong Kong Polytechnic University conducted a formal study to test the reliability of spine deformity measurement of Scolioscan and its validity compared to the gold standard Cobb angle measurements from radiography. Detailed findings reported in an open access article in Scoliosis and Spinal Disorders demonstrated that measurements were very reliable. Good to excellent correlation was also noted in comparison to the conventional radiographic Cobb’s method.
In its current configuration, the system includes a rigid frame with two movable supporting boards and four supporters to maintain the patient’s stable posture during the examination. The system can be used for much more frequent imaging for the spine. Its ability to maintain a consistent posture for examination is important for longitudinal monitoring.
The 3D ultrasound imaging of the spine is achieved through freehand scanning of a custom-designed linear ultrasound probe that contains an electromagnetic spatial sensor to detect the position and orientation of the probe. Lead author Yong-Ping Zheng, PhD, of the Interdisciplinary Division of Biomedical Engineering, and colleagues explained that a range of boundaries in the spine are established. A moving probe is shown in an interface to indicate the location of the ultrasound probe in relation to the upper and lower boundaries to guide scanning.
After images are acquired, 3D image reconstruction and volume project imaging are used to form coronal view images of the spine for further analysis. A non-planar reslicing technique is used to enhance the spinal profile in the coronal image by using the skin surface as a reference for selecting the required voxels. Spinal deformity angles are measured using the curve found approximately near the mid-line of the volume projection image.1
For the study, patients being treated in the Department of Orthopaedics and Traumatology of the Chinese University of Hong Kong were recruited. The patients received conventional standing x-rays within 90 days before the Scolioscan assessment. These were used to calculate the Cobb angle measurement. Twenty patients participated in the inter/intraoperator reliability portion of the study and 49 patients participated in the portion of the study correlating the Cobb angle from radiographs and the spinal curve angle from the Scolioscan.
A team of three researchers acquired and reviewed 24 sets of images for the reliability test. For the correlation test, a single measurement was obtained using the Scolioscan. The single Cobb measurement was measured by an orthopedic physician experienced in interpreting x-rays of scoliosis patients. They compared the Scolioscan angles and the radiographic Cobb angles using linear correlation for thoracic curves alone, lumbar curves alone, and combined results.
The coronal image of the spine was successfully obtained for all the patients. Researchers discovered that the Scolioscan angle slightly underestimated the deformity in comparison with Cobb angle for both the thoracic and lumbar regions. The authors explain that this underestimation was due to the fact that ultrasound images are taken posteriorly and provide anatomical features of vertebra posterior elements rather than the vertebral bodies used in Cobb angle measurement.
The authors are in the process of reducing the size of the system with the goal of creating a portable configuration. They plan to investigate the potential of axial rotation and sagittal measurement using Scolioscan and to determine the feasibility of automated angles measurement. They stated that additional studies are needed to demonstrate clinical values with a larger patient cohort with different types of spinal curvature.
Clinical Study
A prospective single arm clinical trial is underway at the Prince of Wales Hospital in Hong Kong to investigate the validity of Scolioscan for quantitative assessment of spinal deformity and curve severity in scoliosis using radiography as the gold standard for comparison. Curve deformity measurement in terms of Cobb angles assessed by Scolioscan will be correlated comparing mild and severe curves, thoracic and lumbar curves, and findings of patients with low and high body mass indexes (BMI).
One thousand patients between the ages of 8 and 40 are currently being recruited by principal investigator Tsz Ping Lam, MD, of the Chinese University of Hong Kong. The study (NCT02581358) is expected to be completed in September 2017.
REFERENCES
- Cheung CW, Zhou GQ, Law SW, et al. Ultrasound volume projection imaging for assessment of scoliosis. IEEE Trans Med Imaging. 2015 34;8: 1760-1768.
- Zheng YP, Lee TTY, Lai KKL, et al. A reliability and validity study for Scolioscan: a radiation-free scoliosis assessment system using 3D ultrasound imaging. Scoliosis Spinal Disord. Published online May 31, 2016. 11:13. doi: 10.1186/s13013-016-0074-y.