Epidural Hematoma
Although uncommon in the infant population, epidural hematoma is a life-threatening condition that can be treated with timely intervention. The advent of CT scanning has significantly improved outcomes. The Pediatric Emergency Care Applied Research Network guidelines should be used to guide the need for imaging in the setting of pediatric head trauma. If the clinical guidelines are met, a non-contrast head CT should be performed.
Keywords: head trauma, intracranial hemorrhage, Neuroradiology
Case Summary
A toddler presented to the emergency department following a 2-foot fall from an indoor trampoline onto a wooden floor. The baby was drowsy but had no known loss of consciousness. His parents put him to sleep after icing his head. That night, he woke up and had three episodes of emesis and became increasingly irritable. In the emergency department, the initial physical examination was within normal limits, which included a Glasgow Coma Score of 15 and a normal neurologic exam.
Imaging Findings
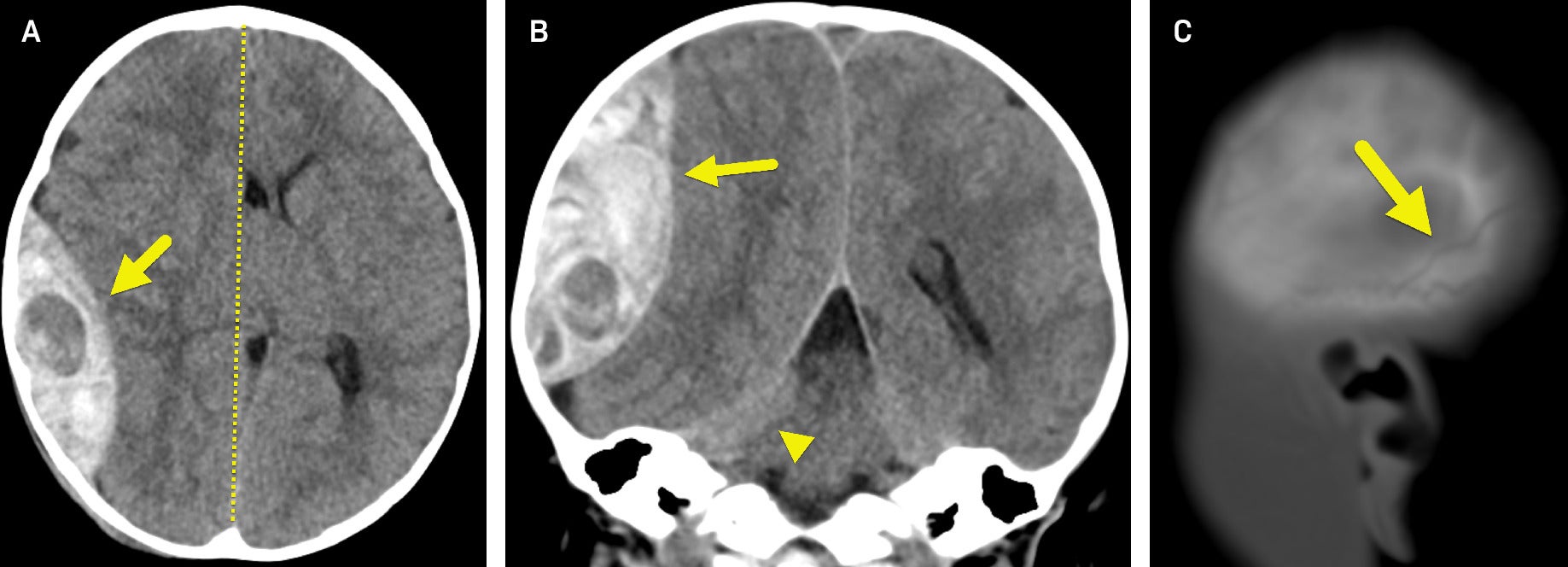
A non-contrast head CT ( Figure 1 ) revealed a large epidural hematoma (EDH) in the right parietal region. There was significant mass effect on the adjacent brain parenchyma with effacement of sulci and the right lateral ventricle, 11-mm right-to-left midline shift, and right uncal herniation. A nondisplaced calvarial fracture was present involving the posterior right parietal bone.
(A) Axial and (B) coronal non-contrast head CT show a large epidural hematoma (arrow) adjacent to the right parietal bone. The hypodense area within the large EH may represent active bleeding. There is a significant mass effect with a right-to-left midline shift (dashed line in A) and a right uncal herniation (arrowhead in B). (C) Sagittal CT image in bone window shows a nondisplaced skull fracture (arrow).
Diagnosis
Epidural hematoma.
Discussion
Epidural hematoma (EDH) is considered an uncommon occurrence in children following head trauma, with an incidence ranging from 1% to 3% of patients who present for care following a head injury.1 Unlike older children and adolescents who generally present with findings of EDH following significant trauma or falls from height greater than 10 feet, infants may present with mechanisms of relatively minor head trauma and falls from less than 5 feet.2 Infants are at an increased risk for significant head trauma compared with adults because of a larger head-to-body ratio, limited head control as a result of weaker neck muscles, and thinner skull bones. Thus, they are more likely to have head-first falls.
The most common symptoms following pediatric head trauma include vomiting and loss of consciousness.3 In infants, additional important symptoms include altered mental status (GCS <15), agitation, lethargy, or caregiver concern for not acting normally.2 Infants who have experienced minor head trauma are generally difficult to evaluate because they cannot describe symptoms and have open cranial sutures and fontanelles. The open sutures and fontanelles permit expansion of intracranial volume and increase the ability to accommodate rises in volume and pressure. Thus, infants may not present with classic signs of loss of consciousness after a lucid interval.1, 3 - 5
An EDH classically occurs as a result of a ruptured blood vessel within the epidural space. In adults, this usually occurs in the setting of a skull fracture and the associated rupture of the middle meningeal artery. In infants and young children, a fracture may or may not be present, and the source of bleeding is more likely to be venous. This is attributed to the plasticity of the skull, the abundance of the vasculature of the dura and growing skull bones, and the relative increase in size of the dural venous sinuses.1 The difference in vascular origin gives rise to more variability in the location of an EDH and the time to presentation, with a decrease in temporal hematomas and a higher incidence of hematomas in the posterior fossa and parieto-occipital regions.1, 6 Additionally, because infants have open fontanelles and sutures, the relative volume of EDHs, especially venous, is generally larger than in adults. This, along with the slower venous bleeds, accounts for the high incidence of concomitant anemia upon presentation.1
Advanced imaging is often not needed in patients presenting with minor head trauma. The Pediatric Emergency Care Applied Research Network (PECARN) has developed a validated clinical decision rule stating that children who are younger than 2 years of age should undergo imaging if they have decreased mental status, a non-frontal scalp hematoma, loss of consciousness greater than 5 seconds, palpable skull fracture, display abnormal behavior according to caregivers, or have a severe mechanism of injury. Infants who do not display one of these signs or symptoms have essentially a 100% negative predictive value for a clinically important traumatic brain injury.2
When needed, non-contrast head CT is the test of choice for imaging patients with suspected significant head trauma. On imaging, EDHs are typically having a biconvex or lentiform shape and do not cross cranial sutures due to the anatomy of dural attachment at the margins of the skull bones.1 This differs from subdural hematomas, which are generally convex in shape and parallel to the inner table of the skull, crossing sutures. It is important to note that EDH can occasionally cross sutural lines, which can occur when a fracture crosses the suture or when there is sutural diastasis.7 Findings related to mass effect may be present as the EDH increases in size and mass effect. Increasing mass effect may result in new onset of seizures, changes in vision, lethargy, and speech. In severe cases, impending downward herniation presenting as decreasing mental status, abnormal pupil size, worsening headache, nausea, and vomiting can occur. Once herniation has occurred, the Cushing triad of bradycardia, irregular respirations, and hypotension will be seen. Without timely decompression, death can result.
Definitive management with neurosurgical decompression and evacuation of the hematoma is almost always required for patients with EDH on imaging with altered mental status or focal neurologic signs. Early detection on CT and prompt surgical evaluation and treatment of EDH have led to improved outcomes.3, 5 Some children who are neurologically intact with small EDHs may be managed non-operatively with regular observation for neurological changes.8, 9
Conclusion
Although uncommon in the infant population, EDH is a life-threatening condition that can be treated with timely intervention. The advent of CT scanning has significantly improved outcomes. The PECARN guidelines should be used to guide the need for imaging in the setting of pediatric head trauma. If the clinical guidelines are met, a non-contrast head CT should be performed.
References
Citation
Mackner JH, Towbin ;RB, Schaefer ;CM, Morgan ;D, Towbin ;AJ, ;3,4*. Epidural Hematoma. Appl Radiol. 2025;(1):.
doi:10.37549/JPCR-25-0009
September 1, 2025