Emphysematous Osteomyelitis
Images

CASE SUMMARY
A 77-year-old with a history of diabetes presented to the emergency department with a chief complaint of low back pain after a ground-level fall. On physical exam, the patient was not alert, oriented, or responding to commands. Pertinent laboratory values included markedly elevated glucose of 967, low sodium of 121, and elevated white blood cell count of 12.6. Blood cultures were positive for Klebsiella pneumonia without a known source.
IMAGING FINDINGS
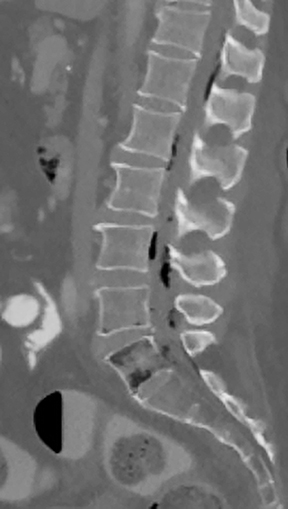
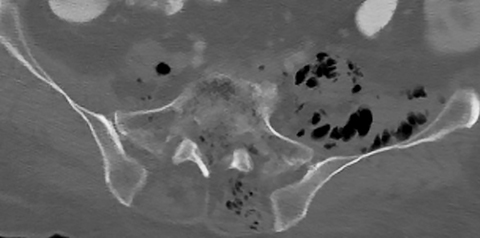
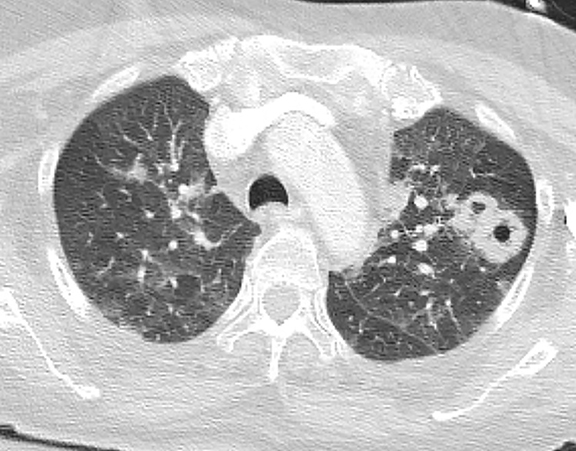
An anteroposterior radiograph of the pelvis demonstrated gas within the paraspinous musculature (Figure 1). Subsequent CT of the lumbar spine revealed intraosseous gas within the L5, S1, and S2 vertebral bodies, with extension of gas into the epidural space and the paraspinal musculature (Figure 2). Lumbar spine MRI demonstrated heterogeneous bone marrow signal related to the intraosseous gas without significant osseous edema or abnormal contrast enhancement. Epidural fluid and gas centered at the L5 level were noted). CT of the chest demonstrated multifocal cavitary lung lesions worrisome for septic emboli (Figure 3).
DIAGNOSIS
Emphysematous osteomyelitis
DISCUSSION
Emphysematous osteomyelitis (EO) is rare, with few cases reported in the literature. Ram et al first described the entity in 1981;1 while the first described case within the spine was in 1982. The condition is most commonly seen in diabetic patients without gender or age predilection and its mortality is reported to be as high as 35%.2 Most cases are monomicrobial, related to bacteremia with gas-forming organisms, with fusibacterium being most common.3 Hematogeneous dissemination is the most common route of spread; however, it has also been noted to develop from spinal surgery, an intra-abdominal source, or from skin or soft-tissue infections.4
Intraosseous gas within the appendicular skeleton is pathognomonic for EO in the absence of recent procedure/intervention.5 However, intraosseous gas seen within a vertebral body is more commonly related to non-infectious causes, such as degenerative or post-procedural changes, neoplasia, or osteonecrosis.2-4 Clinical history and imaging findings elsewhere (ie, septic emboli, as in our case) suggest EO as the underlying diagnosis. Excluding other causes such as recent biopsy/surgery, penetrating trauma, or open fracture, is important before making a diagnosis of EO.
Prior case studies have demonstrated the limited role of radiography in diagnosing EO.4 Traditional imaging features of pyogenic osteomyelitis on MRI such as osseous edema and contrast enhancement are not typically dominant features of EO. Computed tomography is superior to MRI in identifying intraosseous gas; thus, CT is the gold standard for diagnosing this entity. Radiologists may be the first to physicians to suggest the diagnosis, facilitating prompt intravenous antibiotic therapy. However, early surgical intervention should be considered.
CONCLUSION
Emphysematous osteomyelitis is a rare entity that should be included in the differential diagnosis of intraosseous gas, especially in the setting of a diabetic patient with clinical or other imaging features suggestive of systemic infection. It is important to note that radiography should play a limited role in diagnosis, given its high rate of false negative findings. Computed tomography is the gold standard for identifying intraosseous gas, the key imaging feature of EO.
REFERENCES
- Ram PC, Martinez S, Korobkin M, Breiman RS, Gallis HR, Harrelson JM. CT detection of intraosseous gas: A new sign of osteomyelitis. Am J Roentgenol. 1981;137:721.
- Mujer, M. Rai, M. Emphysematous osteomyelitis. BMJ case rep. 2018. doi:10.1136.
- Aiyappan SK, Ranga U, Veeraiyan S. Spontaneous emphysematous osteomyelitis of spine detected by computed tomography: Report of two cases. Craniovertebr Junction Spine. 2014;5:90–92
- Khanduri S, Singh M. Emphysematous osteomyelitis: Report of two cases and review of literature. Indian J Radiology Imaging. 2018; 28(1) 78-80.
- Luey C, Tooley D, Briggs S. Emphysematous osteomyelitis: A case report and review of the literature. Int J Infect Dis. 2012;16:e216–220.
Citation
EM C, C C, N M, J H.Emphysematous Osteomyelitis. Appl Radiol. 2021; (3):56A-56B.
May 4, 2021