Elbow Effusion: Utility and Limitations of Radiography in Pediatric Injuries
Images




This article is accredited for one SA-CME credit. Visit appliedradiology.org/SAM2 for full SA-CME information.
Elbow fractures are common in children and can be extremely subtle on radiographs.1 Most are associated with joint effusion,2 which may suggest occult fracture where none is visible.3-5 Fortunately, effusions can be detected at radiography, the imaging procedure most commonly used to diagnose elbow injuries.
This review article discusses the evidence linking elbow effusion with occult fractures. It also covers the anatomic basis of the fat-pad signs used to diagnose an elbow effusion. Finally, this article reviews the factors and circumstances that can lead to false-positive and false-negative diagnoses of elbow effusions.
Variable Evidence of Predictive Values
Different authors report varying positive predictive values of elbow effusion in the diagnosis of occult elbow fractures. Donnelly, et al, reviewed the follow-up radiographs of 54 children with a history of trauma and elbow effusion without visible fractures on initial radiographs. Nine patients (17%) developed signs of fracture healing, indicating an occult fracture.6 Al-Aubaidi, et al, performed MRI scans in 24 children with effusion and found a fracture in 6 (23%) of these patients.7
In contrast, Skaggs, et al, found an occult fracture in the radiographs of 34 of 45 (76%) children.5 Using follow-up MRI, Major, et al, and Pudas, et al, reported occult fractures in 57% and 89% children, respectively.3,4 Despite the wide variation of these results, it is clear that not all children with effusion on initial presentation have an occult fracture. Most authors also agree that the presence of effusion provides evidence of significant injury and that these children should at least be splinted and clinically followed.8
Radiographic Diagnosis
Al-Aubaidi, et al, found that 5 of the 31 patients in their study were reported to have a positive fat pad sign on their initial radiograph but were deemed to have normal radiographs on subsequent expert review.7 In our experience, inaccurate interpretation of the elbow fat pads is not uncommon and can lead to either a false positive or a false negative diagnosis of elbow effusion. Accurate interpretation of the fat pads requires an understanding of elbow anatomy and optimal positioning for lateral radiographs.
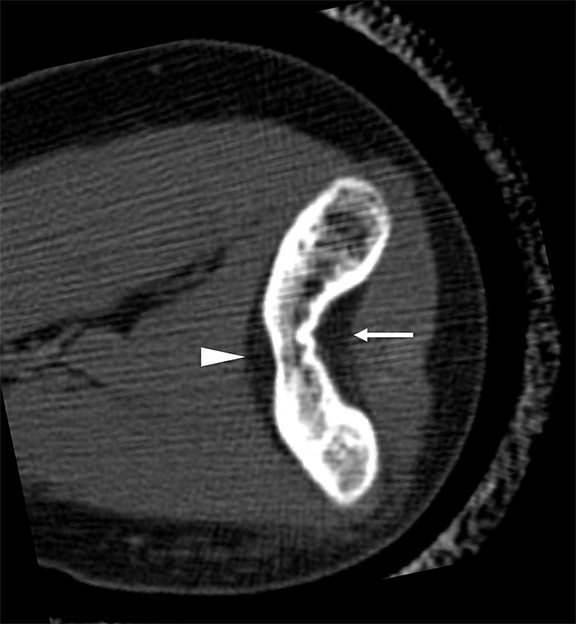
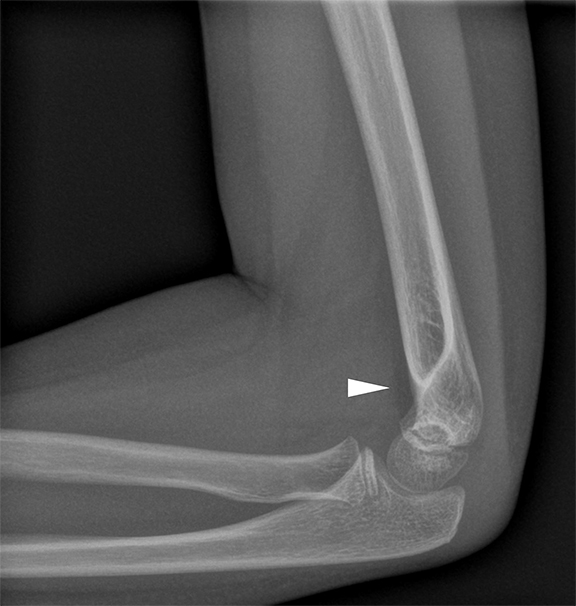
The anterior and posterior fat pads are intracapsular, extrasynovial structures.9 Both the anterior and posterior fat pads are readily visible on CT (Figure 1). The posterior fat pad lies deep within the olecranon fossa and is flanked by bone on three sides. A lateral radiograph in this circumstance would render the posterior fat pad invisible, as it would be obscured by the medial and lateral osseous structures. In contrast, the anterior fat pad is not flanked by bone laterally or medially. Hence, on lateral radiographs the anterior fat pad is normally visible abutting the distal humerus anteriorly (Figure 2).
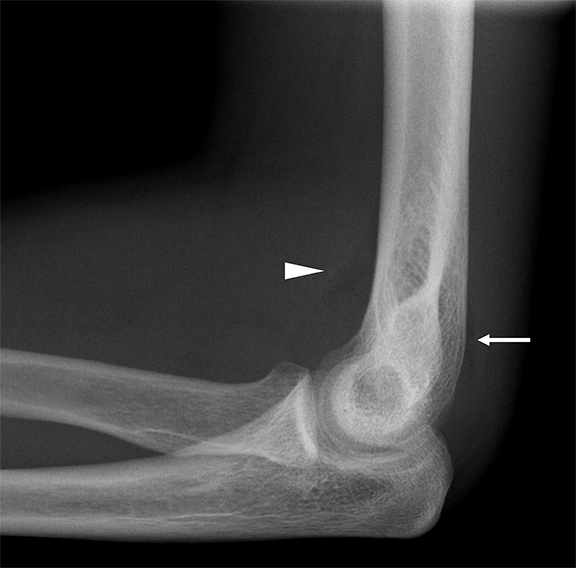
In elbow effusion, the posterior fat pad is displaced dorsally and superiorly by the joint fluid. Thus, bone does not flank the posterior fat pad medially and/or laterally, and it becomes visible on the lateral radiograph (Figure 3). Effusion also displaces the anterior fat pad anteriorly and superiorly. The anterior fat pad, which is normally visible on the lateral radiograph, loses its normal “teardrop’ shape and develops a “sail” shape with a concave inferior margin as it is lifted off the humerus by the joint fluid (Figure 3). Al-Aubaidi, et al, found the anterior fat pad to be more sensitive than the posterior fat pad in detecting effusion, while finding the posterior fat pad to be more specific for underlying osseous injury.7 The negative predictive value of a normal anterior fat pad in ruling out fracture has been reported to be as high as 98.2% in a study of 197 patients with elbow trauma.10
Limitations of Radiography
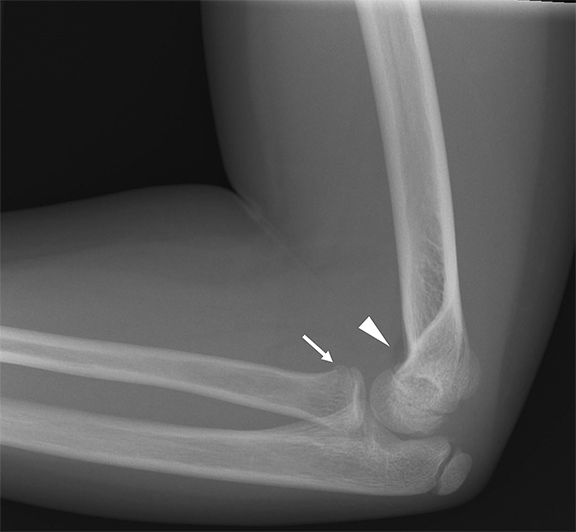
Elbow joint effusion is commonly seen in intra-articular fractures.2 The capsule of the elbow joint attaches to the margins of the trochlea and capitellum, the coronoid process, and the neck of the radius. The olecranon fossa, radiocapitellar joint, ulnotrochlear joint and the proximal radioulnar joint are intracapsular.11 Most fractures involving the intra-articular osseous structures will lead to joint effusion.2 However, intra-articular fractures can be present without joint effusion, with radius neck fractures being the most common such fracture (Figure 4).2 This is because only a small portion of the radius neck is intra-capsular. Fractures involving the bone outside of the capsular attachments, such as avulsion fractures of the medial epicondyle, will not result in an elbow effusion.12 Optimal radiographic technique in obtaining the lateral view of the elbow is important to accurately assessing the fat pads.13 Superimposition of the medial and lateral supracondylar ridges of the distal humerus is a reliable indicator of an adequate lateral radiograph.14 Suboptimal lateral projection can lead to a false-positive or false-negative diagnosis of effusion.13
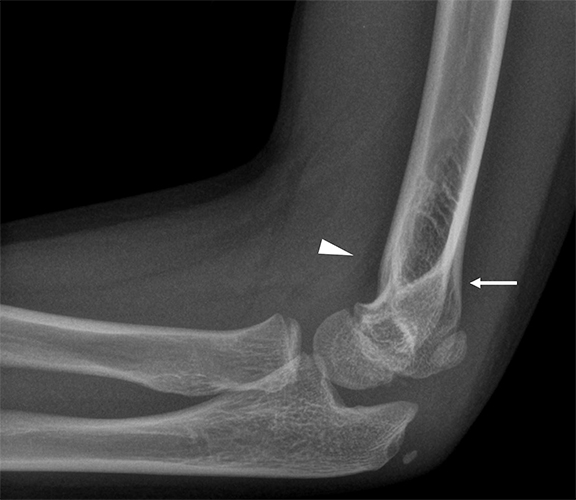
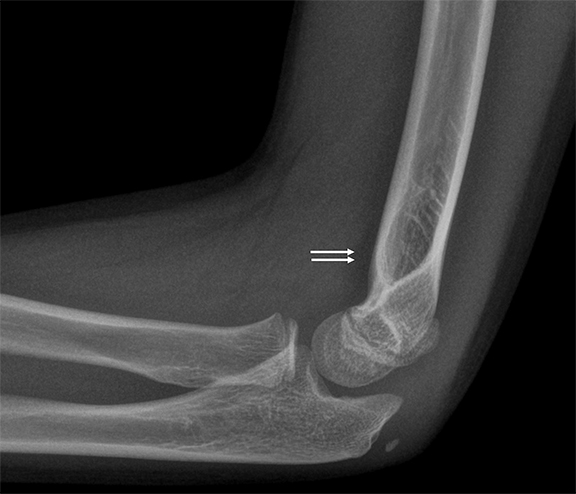
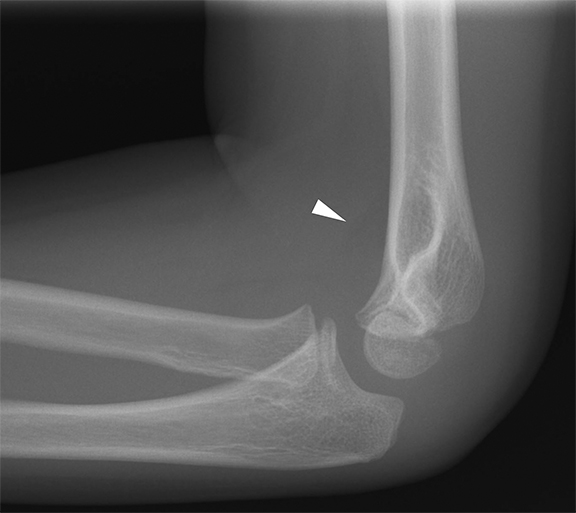
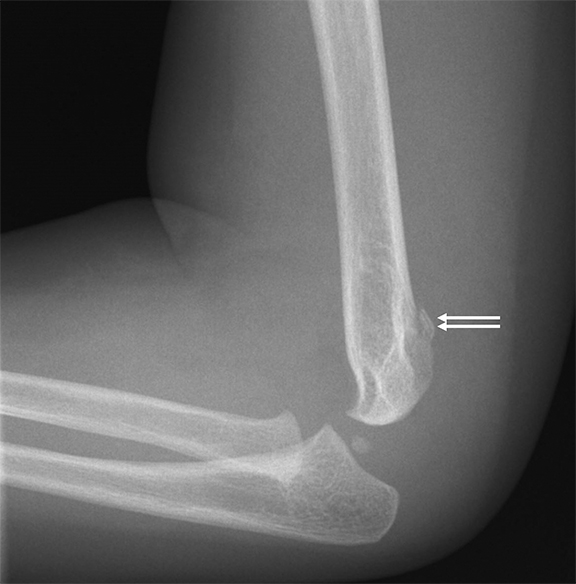
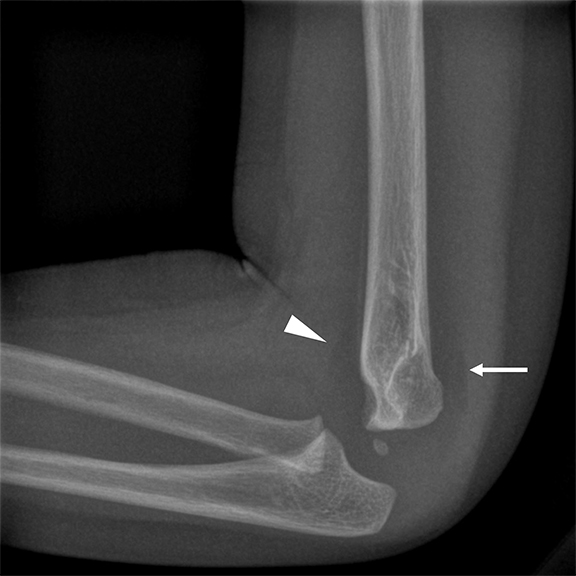
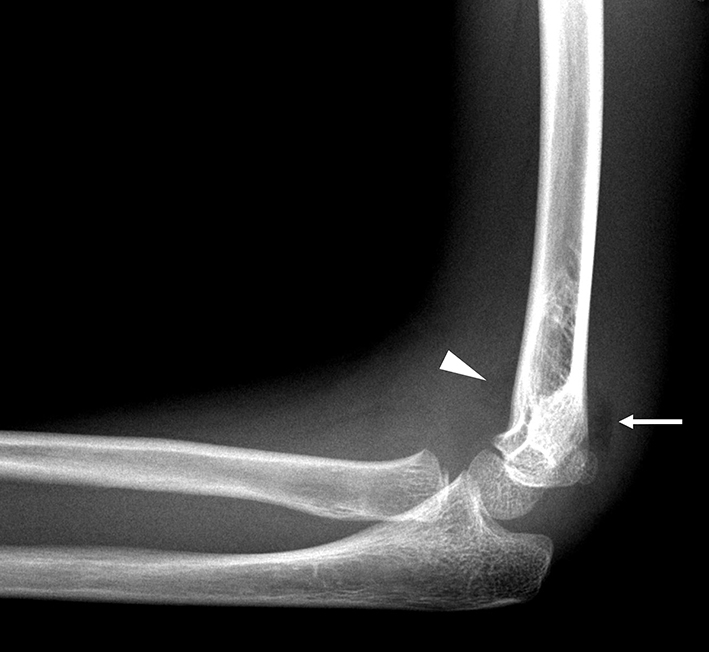
If the lateral projection is not a true lateral, the anterior fat pad may not appear teardrop shaped, but instead may be appear sail-like, leading to a false-positive diagnosis (Figure 5). Conversely, a suboptimal lateral view may lead to obscuring of the posterior fat pad by the medial or lateral supracondylar ridge, leading to a false-negative assessment, even in the presence of an effusion and a potentially elevated posterior fat pad (Figure 6).13 Positioning the upper arm, elbow, and forearm flat on the table during acquisition helps to improve lateral radiograph quality. Adjusting the table or patient-seat height, with the patient’s thumb pointing upward, can help achieve this position. Optimal positioning can also be achieved with the “standing salute” and 90-degree abduction at the shoulder and 90-degree flexion at the elbow.15 The posterior fat pad may be normally visible by obtaining the lateral radiograph in extension, as the olecranon process displaces the fat pad outward in this position (Figure 7).9
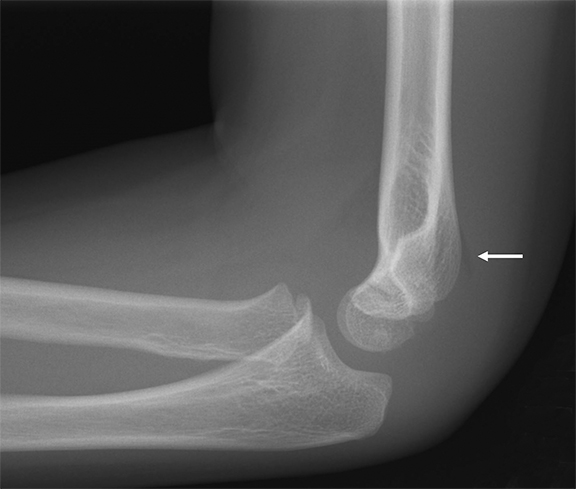
Effusion size also matters with respect to diagnosing elbow effusion from radiographs. A small effusion may elevate only the posterior fat pad, with the anterior fat pad appearing normal (Figure 8).9 At the other end of the spectrum, a very large effusion may efface both the anterior and the posterior fat pads, rendering them invisible on radiographs (Figure 9). Complete lack of visibility of the anterior fat pad may be a clue to the presence of a large effusion in this situation.
A traumatic rupture of the elbow joint capsule may lead to a false-negative fat pad sign, as the capsular tear would allow joint fluid extravasation into the surrounding tissues.16
It is also worth emphasizing that radiographic exposure in the lateral view should be sufficient to differentiate fat from soft-tissue density. An underexposed radiograph may not demonstrate abnormal fat pads even if elbow effusion is present. Similarly, radiologists should be sure to adjust the window width and level while evaluating for elbow effusion, as fat and soft-tissue contrast may not be visible at the default window setting (Figure 10).
Conclusion
Elbow effusion on radiographs may be the only indication of occult fracture in children. Several factors can cause false-positive or false-negative diagnoses of elbow effusion, and knowing these pitfalls is essential to accurately interpret pediatric elbow radiographs.
REFERENCES
- DeFroda SF, Hansen H, Gil JA, et al. Radiographic evaluation of common pediatric elbow injuries. Orthop Rev (Pavia). 2017(1); 9: 7030.
- Emery KH, Zingula SN, Anton CG, et al. Pediatric elbow fractures: a new angle on an old topic. Pediatr Radiol. 2016; 46(1):61-66.
- Major NM, Crawford ST. Elbow effusions in trauma in adults and children: is there an occult fracture? AJR Am J Roentgenol. 2002;178(2): 413-418.
- Pudas T, Hurme T, Mattila K, et al. Magnetic resonance imaging in pediatric elbow fractures. Acta Radiol. 2005; 46(6):636-644.
- Skaggs DL, Mirzayan R. The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Joint Surg Am. 1999;81(10):1429-1433.
- Donnelly LF, Klostermeier TT, Klosterman LA. Traumatic elbow effusions in pediatric patients: are occult fractures the rule? AJR Am J Roentgenol. 1998;171(1):243-245.
- Al-Aubaidi Z, Torfing T. The role of fat pad sign in diagnosing occult elbow fractures in the pediatric patient: a prospective magnetic resonance imaging study. J Pediatr Orthop B. 2012; 21(6): 514-519.
- Donnelly LF. Traumatic elbow effusions in children are not synonymous with occult fracture-even with evaluation by MR imaging. AJR Am J Roentgenol. 2002;179(2):531-532.
- Murphy WA, Siegel MJ. Elbow fat pads with new signs and extended differential diagnosis. Radiology. 1977;124(3): 659-665.
- Blumberg SM, Kunkov S, Crain EF, et al. The predictive value of a normal radiographic anterior fat pad sign following elbow trauma in children. Pediatr Emerg Care. 2011;27(7):596-600.
- Kamineni S, Bachoura A, Sasaki K, et al. Inner synovial membrane footprint of the interior elbow capsule: an arthroscopic boundary. Anat Res Int. 2015:426974.
- Sheehan SE, Dyer GS, Sodickson AD, et al. Traumatic elbow injuries: what the orthopedic surgeon wants to know. Radiographics. 2013;33(3):869-888.
- Kilborn T, Moodley H, Mears S. Elbow your way into reporting paediatric elbow fractures – A simple approach. SA Journal of Radiology. 2015; 19(2):881. doi 10.4102/sajr.v19i2.881.
- Skibo L, Reed MH. A criterion for a true lateral radiograph of the elbow in children. Can Assoc Radiol J. 1994; 45(4): 287-291.
- Eren MB, Asci M, Bilgic E, et al. A practical method for obtaining true lateral elbow X-rays in a pediatric age group: lateral elbow X-ray in the standing salute position. Ind J Ortho. 2020; doi 10.1007/s43465-020-00238-9.
- Bledsoe RC, Izenstark JL. Displacement of fat pads in diseases and injury of the elbow: a new radiographic sign. Radiology. 1959; 73: 717-724.
Citation
SS K.Elbow Effusion: Utility and Limitations of Radiography in Pediatric Injuries. Appl Radiol. 2021; (3):11-16.
May 4, 2021