Ectopic Parathyroid Adenoma in the Pyriform Sinus: Case Report
Images

CASE SUMMARY
A 55-year-old presented with persistent, mildly elevated calcium levels ranging from 10.6 to 11.4 mg/dL over 5 years. Further lab work revealed elevated parathyroid hormone (PTH) of 129 pg/mL and ionized calcium at 1.63 mmol/L.
On nasopharyngolaryngoscopy, a beefy red, jelly bean-shaped mass covered by a thin layer of mucosa with hypervascularity in the left pyriform sinus was found and surgically excised. Intraoperative pathology demonstrated parathyroid tissue and that intraoperative PTH levels dropped from 160 to 13 pg/mL 15 minutes’ post-resection.
Final pathology was consistent with parathyroid adenoma. Calcium levels returned to normal on postoperative follow-up.
IMAGING FINDINGS
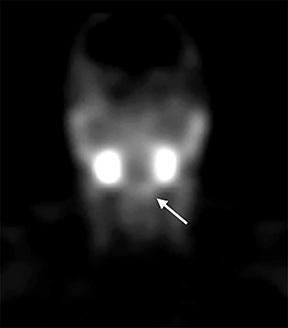
A technetium-99m-labeled sestamibi parathyroid scan was performed to evaluate for a parathyroid adenoma. The scan was interpreted as absent for scintigraphic evidence for parathyroid adenoma (Figure 1).
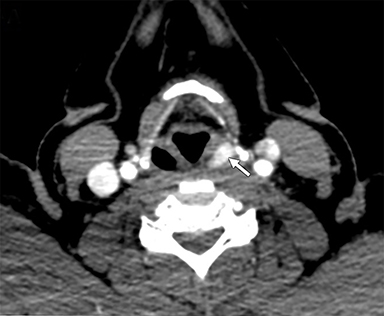
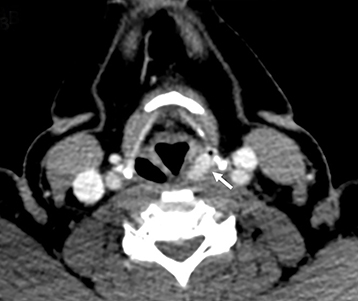
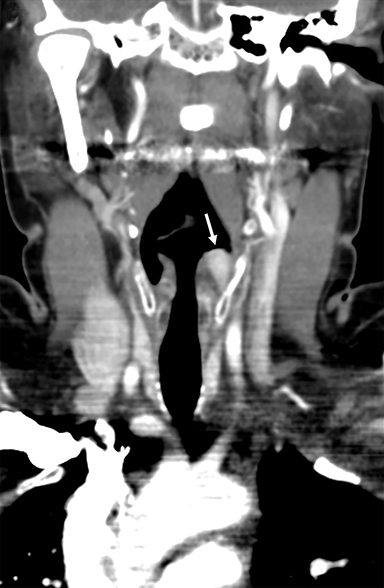
A two-phase contrast-enhanced CT scan of the neck was then performed, demonstrating an enhancing ovoid mass measuring 1.2 x 0.7 cm in the left pyriform sinus (Figure 2). The mass demonstrated avid enhancement during the arterial phase with washout on the venous phase. Retrospective review of the sestamibi parathyroid scan showed subtle asymmetric radiotracer uptake in this region (Figure 1).
DIAGNOSIS
Ectopic parathyroid adenoma in the pyriform sinus
DISCUSSION
Primary hyperparathyroidism is the most common cause of hypercalcemia in otherwise healthy patients. This is usually found incidentally on lab work as most patients are asymptomatic. Nonspecific symptoms such as weakness, depression, and anorexia can be seen and long-term untreated hyperparathyroidism can lead to osteoporosis and renal calculi. Approximately 90% of cases are caused by a single parathyroid adenoma.1 Resection of the adenoma(s) is the definitive treatment, with cure rates as high as 98%. Intraoperative PTH is expected to fall by at least 50% or to normal range10-15 minutes after excision. Failure to drop indicates that the adenoma is in a different location or that multiple adenomas may be present.2
Parathyroid glands contain chief cells (which secrete PTH) and oxyphil cells (which contain high amounts of mitochondria). Standard anatomy consists of four parathyroid glands (paired superior and inferior glands), but it is not uncommon for a patient to have more than 4 glands; a range of 2 to 12 glands has been described.3
In a large study of surgery for hyperparathyroidism, 22% had ectopic adenomas. Ectopic locations included thymus (38%), retro/paraesophageal region (31%), intrathyroidal (18%), mediastinal (6%), undescended (4%), and carotid sheath (3%).4
Knowledge of the embryology of the parathyroid glands is crucial to understanding the variability in parathyroid number and location. The superior parathyroid glands arise from the paired fourth pharyngeal pouches along with the lateral thyroid gland. The inferior parathyroid glands arise from the third pharyngeal pouches along with the thymus. The longer descent of the inferior glands likely explains the increased ectopy relative to the superior glands, as well as large range of parathyroid locations. An inferior parathyroid gland with prematurely arrested migration can be located above the thyroid at the level of the third pharyngeal pouch or it can descend with the thymus to the mediastinum.3,5
A parathyroid in the pyriform sinus is exceedingly rare, with 10 cases identified in the literature.6 The third and fourth pharyngeal pouches also give rise to the pyriform fossa.7 Early in embryogenesis, the parathyroid glands separate from the pharyngeal wall prior to their descent. Early arrest of the descent of the parathyroid tissue and implantation into the pharyngeal wall is the proposed cause of pyriform sinus parathyroid ectopy.6 Though undescended parathyroids account for a small amount of ectopic parathyroids, they constitute a significantly higher percentage of adenomas with negative initial imaging workup and failed cervical exploration.8
Owing to anatomic variability, localization imaging is an important part of the preoperative workup. The most common initial study when primary hyperparathyroidism is suspected is a nuclear medicine parathyroid scan with a single isotope, dual-phase Tc-99m sestamibi scan being most common. Sestamibi concentrates in cells rich in mitochondria, such as the previously mentioned oxyphil cells.1 Normal sestamibi distribution includes the salivary glands, thyroid, heart, and liver, with mild uptake seen in marrow, brown fat, and the thymus (in young patients). Normal parathyroid glands are typically not visualized. Parathyroid adenomas demonstrate radiotracer uptake that does not wash out on delayed imaging. This is distinguished from normal thyroid that does wash out through obtaining an early acquisition (10-20 minutes’ post injection) and delayed acquisition (1.5-3 hours post injection). The addition of single-photon emission computerized tomography (SPECT/CT) to a sestamibi scan increases sensitivity and improves localization.1 Ultrasound can also be useful when done after a positive sestamibi scan with a meta-analysis demonstrating improved sensitivity from 78% to 88% in the case of single adenoma, 16 to 30% in double adenomas, and from 35 to 44% in multi-gland hyperplasia.1
Multi-phase CT provides an alternative method of preoperative localization and an additional modality when imaging is inconclusive or when surgery is unsuccessful. Four-dimensional (4D) CT is tailored for identifying parathyroid adenomas, with the time dimension allowing for assessment of contrast dynamics, specifically contrast washout in the case of parathyroid adenomas. 4D CT has been described consisting of two, three, and four phases with varying degrees of accuracy reported in the literature. Parathyroid adenomas typically demonstrate avid enhancement (138-150 hounsfield units (HU)) on arterial phase and washout on delayed phase (hypodense relative to thyroid). This contrasts with normal lymph nodes, which show progressive enhancement from arterial to venous phase.3 Parathyroid tissue is hypodense compared to thyroid tissue on precontrast images because of normal thyroid iodine content, further aiding in differentiation.
CONCLUSION
Although the pyriform sinus is a very uncommon ectopic location for a parathyroid adenoma, parathyroid ectopy is common and extremely variable in location. This can have a large impact on successful surgical treatment of primary hyperparathyroidism. Knowledge of the embryologic formation and migration of parathyroid glands, and therefore, their potential locations, is crucial for preoperative evaluation by radiologists to assist operative management by surgeons.
REFERENCES
- Eslamy HK, Ziessman HA. Parathyroid Scintigraphy in Patients with Primary Hyperparathyroidism: 99mTc Sestamibi SPECT and SPECT/CT. RadioGraphics. Volume 28, Issue 5 Sep 1 2008.
- Weigel RJ (2017) Minimally Invasive Parathyroidectomy with Intraoperative PTH Testing. In: Howe J. (eds) Endocrine and Neuroendocrine Surgery. Springer Surgery Atlas Series. Springer, Berlin, Heidelberg.
- Policeni BA, Smoker WRK, Reede DL. Anatomy and Embryology of the Thyroid and Parathyroid Glands. Seminars in Ultrasound, CT and MRI. Volume 33, Issue 2, 2012, Pages 104-114, ISSN 0887-2171.
- Roy M, Mazeh H, Chen H, Sippel R. Incidence and Localization of Ectopic Parathyroid Adenomas in Previously Unexplored Patients. World Journal of Surgery. (2013) 37: 102.
- Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. The American Journal of Surgery. Volume 191, Issue 3, 2006.
- Helman SN, Moubayed SP, Ho BT, Din-Lovinescu C, Urken ML. Parathyroid Adenoma of the Piriform SInus: Case Series, Embryologic Basis, and Review of the Literature. AACE Clinical Case Reports. Autumn 2017, Vol. 3, No. 4, pp. e379-e383.
- Adams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights into Imaging. 2016;7(1):69-76. doi:10.1007/s13244-015-0454-5.
- Kanack MD, Maawy AA, Oh DK, Bouvet M. Undescended parathyroid adenoma. BMJ Case Reports. 2015; 2015:bcr2014208277. doi:10.1136/bcr-2014-208277.
Citation
S M, S P, J W, B G.Ectopic Parathyroid Adenoma in the Pyriform Sinus: Case Report . Appl Radiol. 2020; (3):48J-48L.
May 5, 2020