Dural Arteriovenous Fistula
Images

Case Summary
An adult presented to the emergency department with vertigo, headache, and a four-day history of vision changes. Previous medical history included transient ischemic attack, right internal carotid aneurysm, remote stroke, chronic sinusitis, hypertension, diabetes, and remote traumatic brain injury.
Imaging Findings
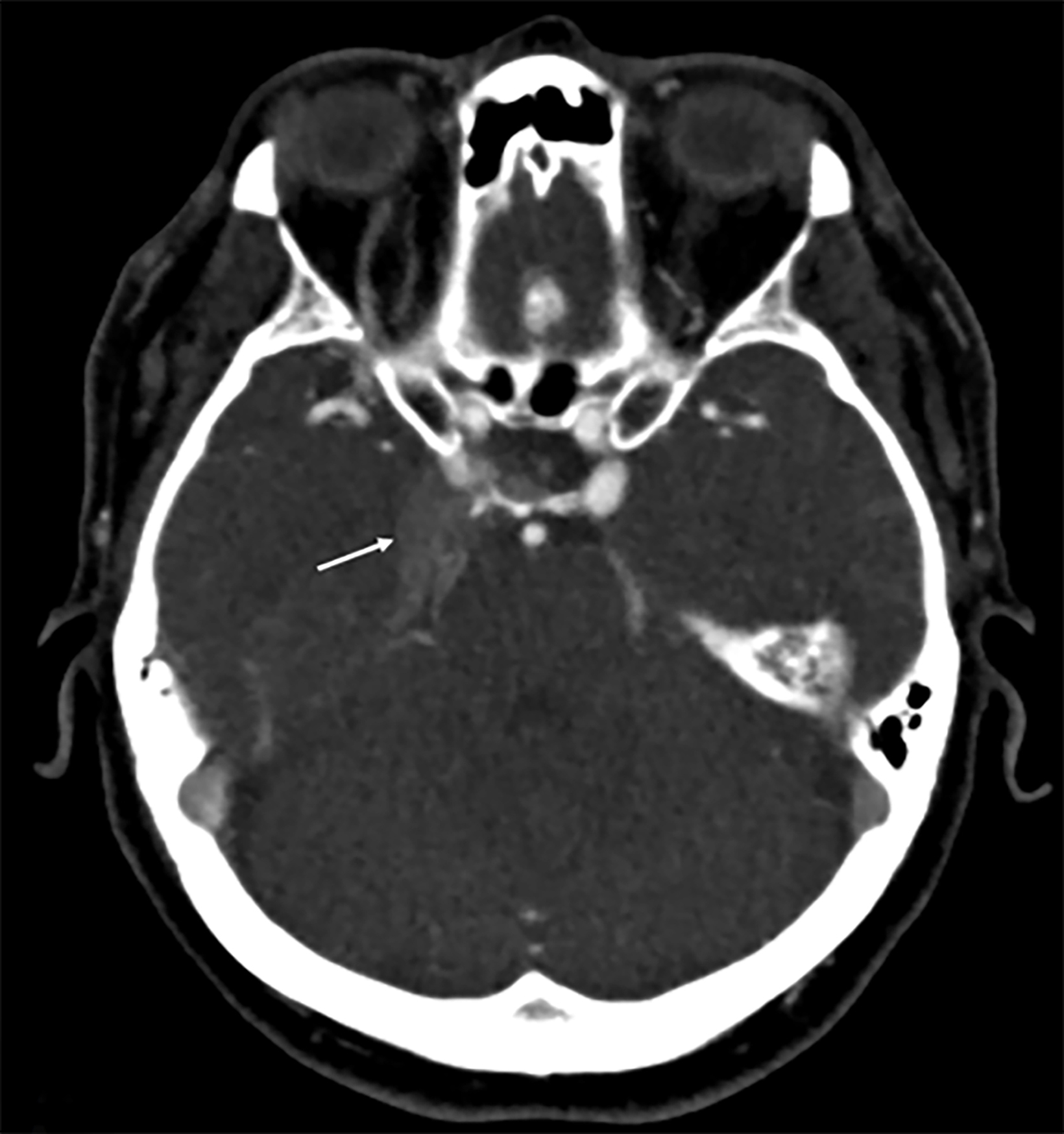
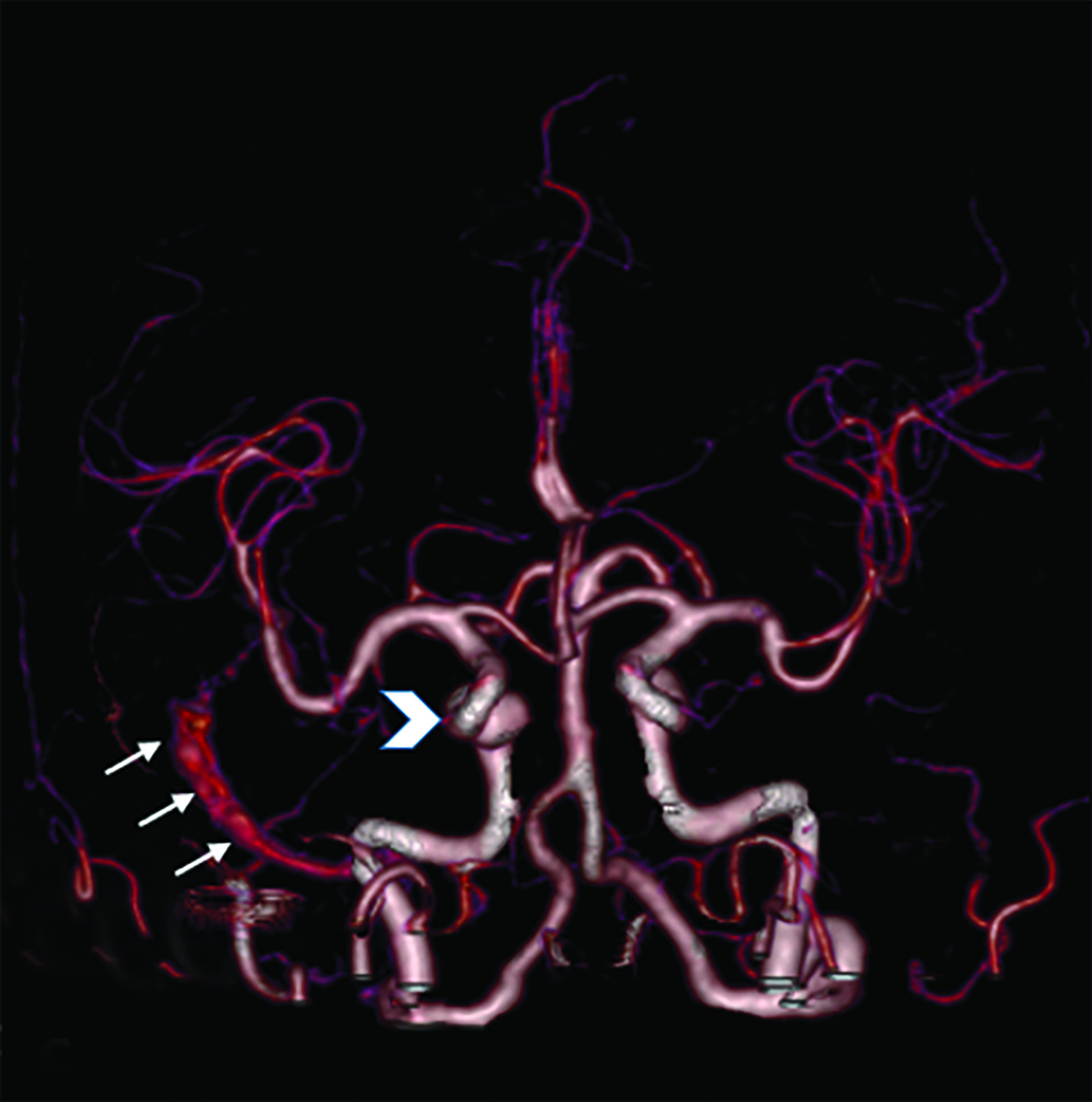
Computed tomography angiography (CTA) demonstrated expansion and arterial phase enhancement of the right cavernous sinus and retrograde filling of the right superior ophthalmic vein. A 3D reconstruction revealed early filling of the right sigmoid sinus on the arterial phase (Figure 1).
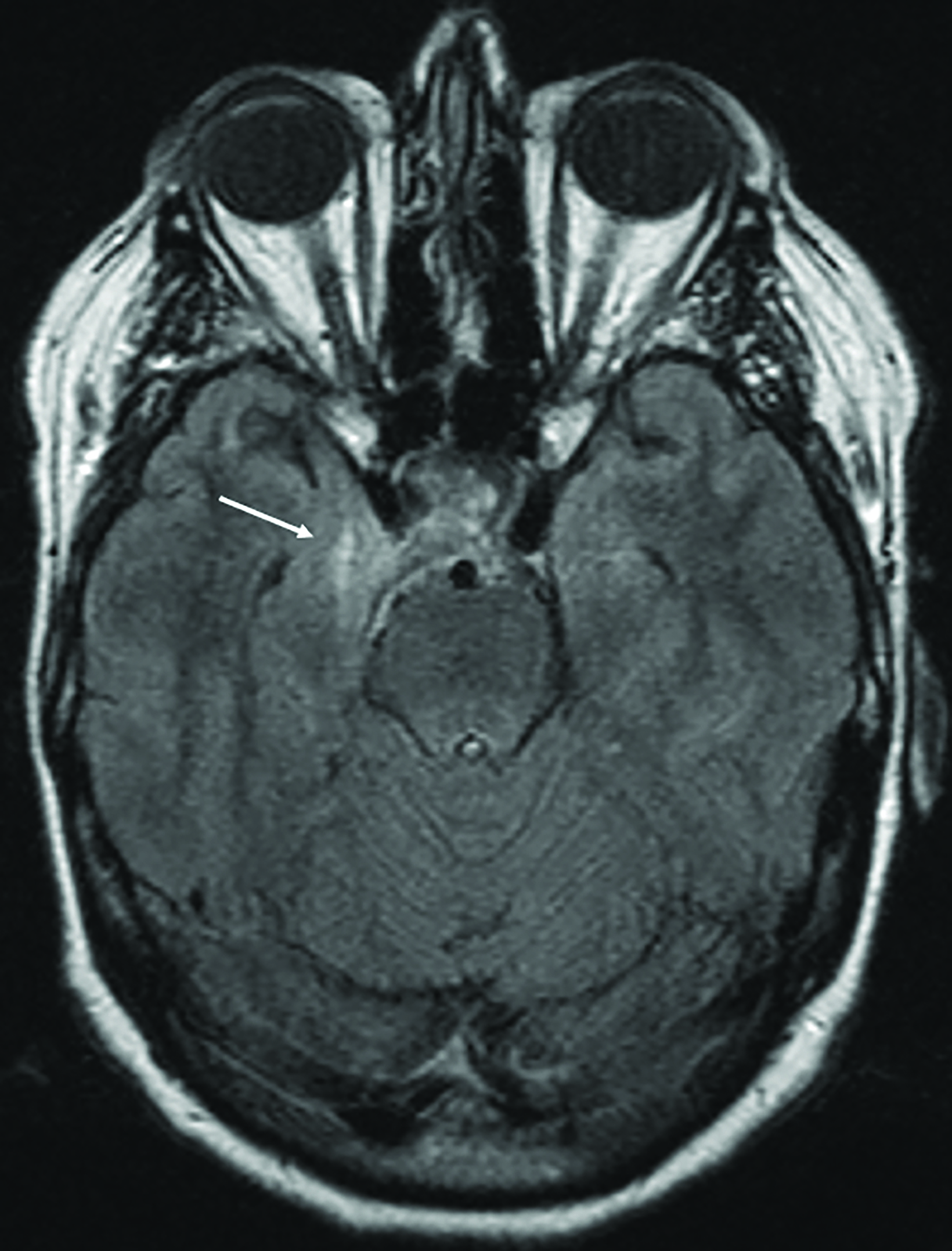
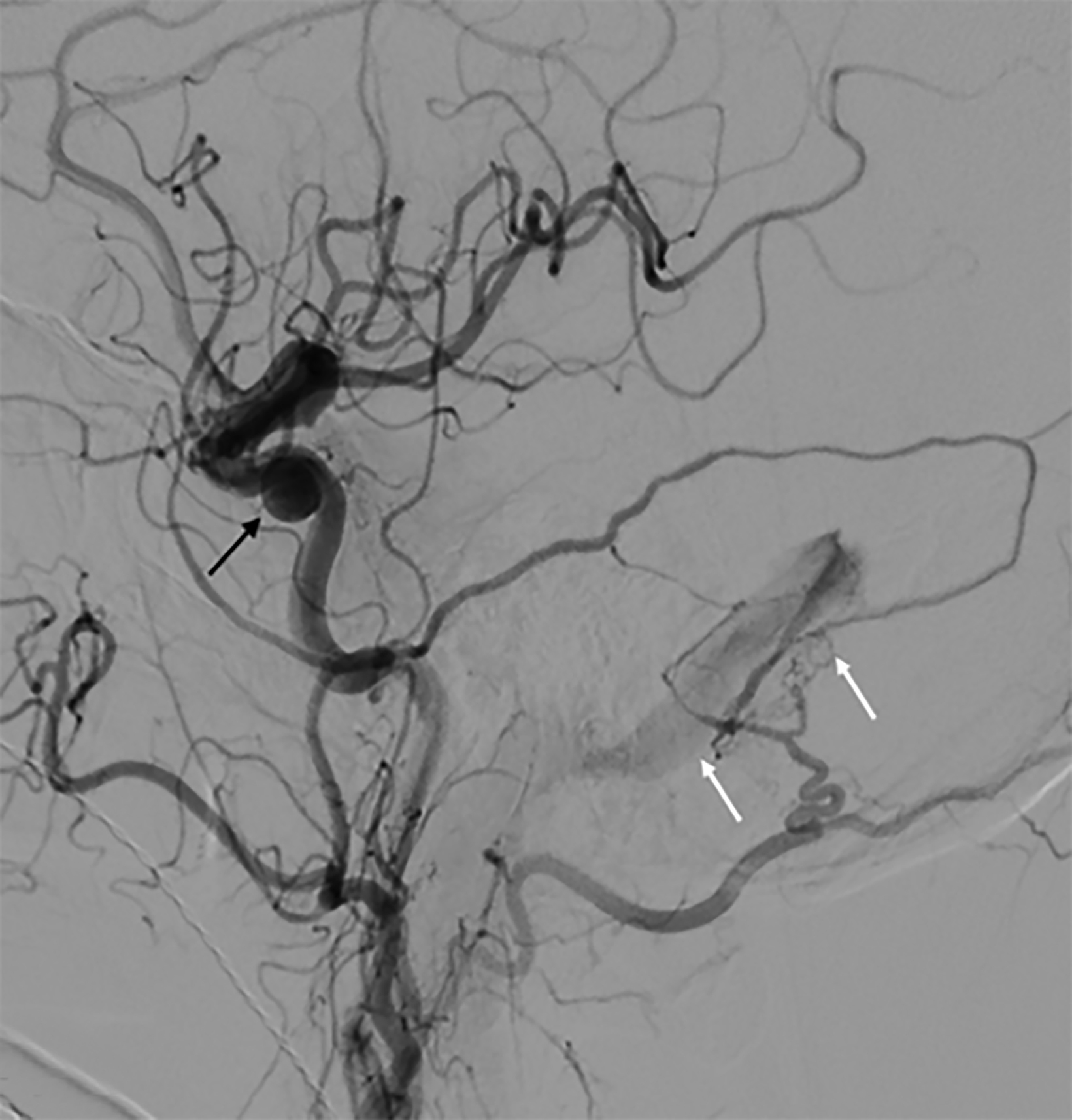
Magnetic resonance imaging demonstrated increased T2 FLAIR signal within the right cavernous sinus (Figure 2). Digital subtraction angiography (DSA) was negative for a carotid-cavernous fistula but demonstrated a dural arteriovenous fistula (DAVF) between the right occipital artery and right sigmoid sinus. The terminal branches of the right middle meningeal artery were also communicating with the DAVF (Figure 3). The drainage through this sinus, however, remained anterograde (Borden type I AV fistula).
Diagnosis
Dural arteriovenous fistula (DAVF)
Discussion
Intracranial DAVFs are pathologic shunts occurring between the dural arteries and the venous sinuses, meningeal veins, or cortical veins; they account for 10%-15% of all intracranial malformations.1 The transverse, sigmoid, and cavernous sinuses are common locations for most DAVFs.2 Symptoms may include tinnitus, diplopia, ocular pain, exophthalmos, and intracranial hemorrhage. Low-grade DAVFs are usually benign, with a reported 2% rate of conversion to aggressive.3 We present a case of DAVF which was treated with endovascular embolization and open surgery.
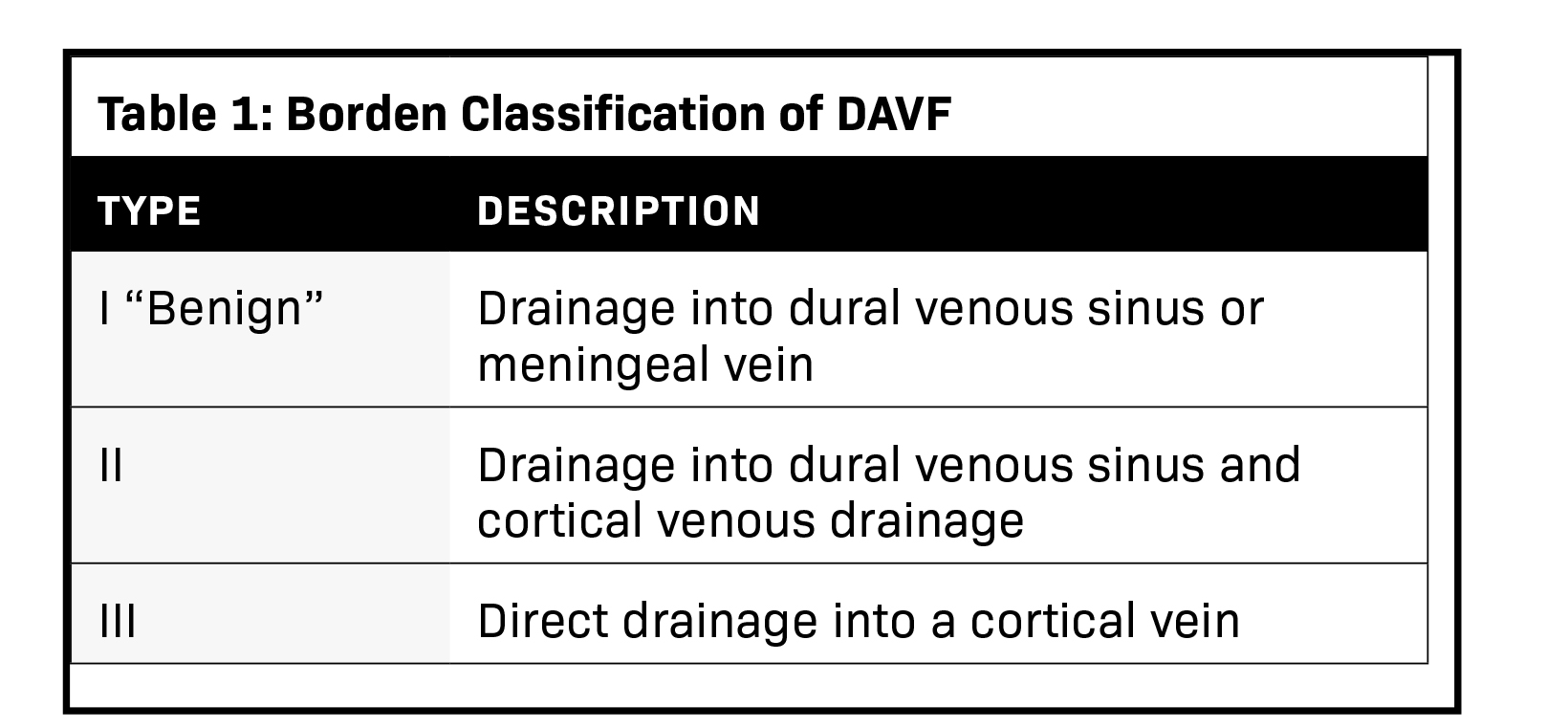
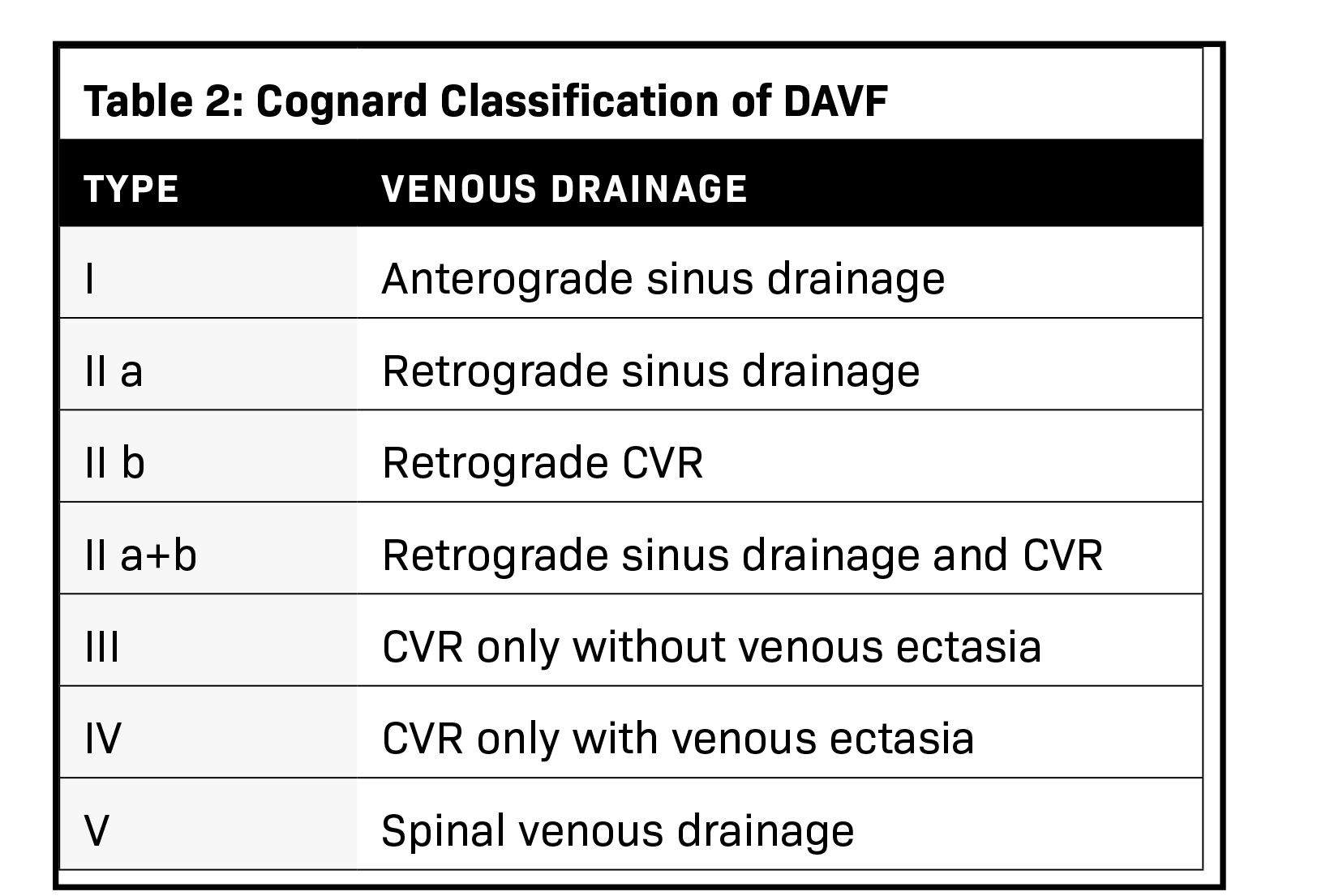
The severity of DAVF symptoms is determined by the venous drainage pattern. There are two classification schemes, Borden, et al, and Cognard, et al (Tables 1 and 2).4,5 The Borden classification, more frequently used clinically, classifies lesions based on the site of venous drainage and the presence of cortical venous drainage (CVD). The Cognard classification, however, is more anatomic and imaging oriented. It is based on the direction of dural sinus drainage, presence of CVD, and venous outflow architecture. In both classifications, the lack of CVD is associated with a benign course and an extremely low risk of intracranial hemorrhage.6 DAVF has a dynamic nature and can convert into a more aggressive type or undergo spontaneous resolution.7 A change in symptoms requires reevaluation, as it may reflect exacerbation of the venous drainage pattern. Further subdivision of aggressive types in both classifications into symptomatic and asymptomatic improves the accuracy of risk stratification, as demonstrated by Zipfel, et al.6 The study revealed a significant difference in the annual hemorrhage risk between symptomatic and asymptomatic subtypes of 7.4% and 1.5%, respectively.6 DAVF are initially evaluated with noncontrast CT and MRI. Any suspicious dilated vessels, venous pouches, or vascular enhancement should be further evaluated with CTA or MRA.1 Four-dimensional (4D) CTA using a can accurately diagnose, classify, and assist in treatment planning for DAVF. A recent preliminary study showed an accuracy rate of 85.7% using 4D CTA to detect DAVF feeding arteries.8 However, DSA remains the most accurate method for DAVF detection and classification.
Endovascular therapy is the mainstay of treatment. Nevertheless, surgery, stereotactic radiosurgery, or combined approaches may be alternatives in cases of failed endovascular therapy, as in this case. Owing to a sharp turn at its origin, the occipital artery was not accessible endovascularly. The aim of endovascular treatment is to completely eliminate the arteriovenous shunt to prevent recruitment of collaterals and persistent risk of hemorrhage.9 Surgical options include direct intraoperative embolization of meningeal arteries or veins, dural resection, venous sinus packing, and skeletonization of the dural sinus with disconnection of the dural arterial supply. A combined approach employing presurgical arterial embolization is reported 100% efficient in DAVF ablation. However, mortality and morbidity risks remain considerable (>10%).10
Conclusion
Dural arteriovenous fistulas are uncommon; CTA is effective for diagnosis and follow-up. Three-dimensional reconstructions offer a dynamic look at the fistula and its feeding arteries. However, it remains less sensitive than DSA. Endovascular embolization is the gold standard for DAVF treatment. Surgery is considered in cases where endovascular approaches have failed or are not feasible.
References
- Kwon BJ, Han MH, Kang HS, et al. MR imaging findings of intracranial dural arteriovenous fistulas: relations with venous drainage patterns. Am J Neuroradiol. 2005;26: 2500–2507.
- Kirsch M, Liebig T, Kuhne D, et al. Endovascular management of dural arteriovenous fistulas of the transverse and sigmoid sinus in 150 patients. Neuroradiology. 2009; 51:477–483.Satomi J, van Dijk JM, Terbrugge KG, et al. Benign cranial dural arteriovenous fistulas: outcome of conservative management based on the natural history of the lesion. J Neurosurg. 2002;97:767–770.
- Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166–179.
- Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 1995;194:671–680.
- Zipfel GJ, Shah MN, Refai D, et al. Cranial dural arteriovenous fistulas: modification of angiographic classification scales based on new natural history data. Neurosurg Focus. 2009;26:E14.
- Luciani A, Houdart E, Mounayer C, et al. Spontaneous closure of dural arteriovenous fistulas: report of three cases and review of the literature. Am J Neuroradiol. 2001;22:992–996.
- Tian B, Xu B, Lu J, et al. Four-dimensional computed tomography angiographic evaluation of cranial dural arteriovenous fistula before and after embolization. Eur J Radiol. 2015;84;1144–1149.
- Mironov A. Selective transvenous embolization of dural fistulas without occlusion of the dural sinus. Am J Neuroradiol. 1998;19:389–391.
- Kakarla UK, Deshmukh VR, Zabramski JM, et al. Surgical treatment of high-risk intracranial dural arteriovenous fistulae: clinical outcomes and avoidance of complications. Neurosurgery. 2007;61:447–459.
References
Citation
S M, A F, A K, M B.Dural Arteriovenous Fistula. Appl Radiol. 2022; (2):39-41.
March 4, 2022