Clear Cell Renal Cell Carcinoma with Metastasis to the Thyroid
Images

CASE SUMMARY
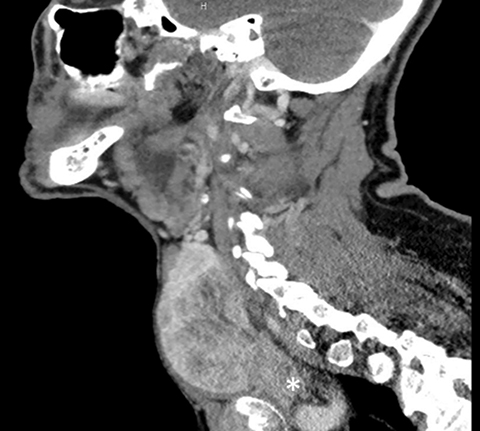
An elderly patient presented with a rapidly enlarging neck mass and associated voice changes. They denied dysphagia, odynophagia, or weight changes. Physical examination revealed a right sided neck mass, enlarged submandibular glands, and leftward deviation of the trachea. Medical history included renal cell carcinoma (RCC) treated with nephrectomy, prostate cancer treated with radiation, cerebrovascular accident with residual left-sided weakness, hypertension and hyperlipidemia. Contrast-enhanced computed tomography (CECT) scan revealed a mass with ill-defined margins in the right thyroid lobe with extension into the mediastinum, causing moderate tracheal deviation.
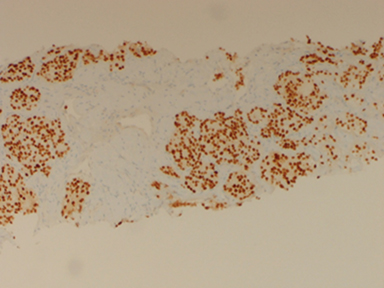
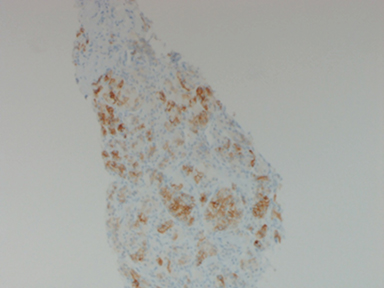
Preliminary pathology reports of the right thyroid mass revealed clear cell neoplasm consistent with either primary follicular thyroid cancer or metastatic renal cell carcinoma. Paired box gene 8 (PAX8) and carbonic anhydrase IX (CAIX) immunostains were positive in the same biopsy sample which further solidified the diagnosis of metastatic clear cell renal cell carcinoma (Figure 1). Thyroglobulin and thyroglobulin transcription factor-1 (TTF-1) stains were negative, effectively ruling out primary thyroid neoplasm.
IMAGING FINDINGS
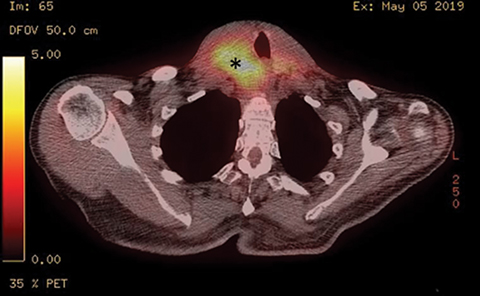
Initial diagnostic workup included CT abdomen and pelvis without contrast demonstrating cortical cysts in the right kidney and a surgically absent left kidney. CT of the neck revealed a heterogeneously enhancing right thyroid lobe mass with upper mediastinal extension and leftward shift of the trachea (Figure 2). After biopsy and initiation of chemotherapy, the patient was assessed with PET/CT (Figure 3).
DIAGNOSIS
Clear cell renal cell carcinoma with metastasis to the thyroid
DISCUSSION
Accounting for 3% of all malignancies, RCC is the most common renal malignancy of adults and the seventh-most common malignancy overall in men.1 RCC occurs more often in males (2:1 ratio) and tends to present later in life, often occurring after the 6th decade (median age 64).1 The clear cell variant, as seen in our case, is the most common subtype constituting up to 75% of all RCC cases.4 Other histopathological subtypes of RCC include papillary carcinoma, medullary carcinoma, and collecting duct carcinoma, as well as unclassified variants that can be differentiated using immunohistochemical stains.3
The most common route of RCC metastasis is hematogeneous; frequent targets include the liver, lung, bone, lymph nodes, and brain. Metastasis to the thyroid is rare, although RCC is the most common malignancy to spread to the thyroid. Findings of thyroid involvement can present at any time from initial diagnosis through several years following initiation of treatment (including nephrectomy), as in this case.
Recurrence ranging from several months to years following diagnosis is a prominent feature of RCC. Most recurrences occur within three years of surgery, although delayed recurrences of up to 26 years have been reported.6 Approximately 20-30% of patients, including those who have undergone curative nephrectomy, will develop recurrence; of these, upwards of 50% will develop distant metastasis.2,5
Ultrasound images of metastatic thyroid lesions usually demonstrate well-demarcated nodules with hypoechoic centers and increased vascular markings.7 While providing some information about the lesion, these findings remain nonspecific, making it nearly impossible to distinguish primary from secondary thyroid lesions.7
Fine-needle aspiration (FNA) cytology reliably establishes perioperative diagnosis, but several tumors of thyroid origin may present with a clear cell component on FNA cytology alone. Immunohistochemistry remains a powerful tool with increased sensitivity and specificity for RCC. Markers such as CAIX, anti-human kidney injury molecule-1 (hKIM-1), and PAX8 are highly sensitive and specific markers used to identify RCC.5
The traditional immunohistochemical markers to identify primary thyroid malignancies are thyroglobulin, TTF-1, and calcitonin.5 In our case, immunohistochemical stains were positive for CAIX and PAX-8 and negative for TTF-1.
Definitive diagnosis of metastatic RCC is typically made through histopathological testing following thyroidectomy.
CONCLUSION
Metastatic thyroid lesions pose a significant diagnostic challenge to clinicians, as they quite often occur years after diagnosis and treatment of the primary lesion. Although metastasis to the thyroid should remain a differential diagnostic consideration in any case of primary RCC, preoperative diagnosis remains difficult.
Patients presenting with a history of RCC and a concurrent thyroid mass should be evaluated for thyroid metastasis. While most metastatic masses to the thyroid are asymptomatic, presenting symptoms may include painless palpable nodules, voice changes, shortness of breath/wheezing, or difficulty swallowing.
REFERENCES
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: Cancer J Clin. 2016; 66(1): 7–30.
- Motzer RJ, Bander NH, Nanus DM, Renal cell carcinoma. NEJM.1996; 335(12): 865–875.
- Kovacs G, Akhtar M, Beckwith BJ, et al. The Heidelberg classification of renal cell tumours. J Pathol.1997;183(2):131–133.
- Hsieh, JJ, Purdue MP, Signoretti S, et al. Renal cell carcinoma. Nature Rev Dis Pri. 2017;3: 17009.
- Flanigan RC, Campbell SC, Clark JL, Picken MM. Metastatic renal cell carcinoma. Curr Treat Opt Oncol. 2003; 4(5):385–390.
- Nakhjavani MK, Gharib H, Goellner JR, van Heerden JA. Metastasis to the thyroid gland: a report of 43 cases. Cancer.1997; 79(3):574–578.
- Song OK, Koo JS, Kwak JY, Moon HJ, Yoon JH, Kim EK. Metastatic renal cell carcinoma in the thyroid gland: ultrasonographic features and the diagnostic role of core needle biopsy. Ultrasonography. 2016; 36(3):252-259.
- Cilengir AH, Kalayci TO, Duygulu G, Rezanko TA, İnci MF. Metastasis of renal clear cell carcinoma to thyroid gland mimicking adenomatous goiter. Pol J Radiol. 2016; 81:618-621. doi:10.12659/PJR.899459
References
Citation
H S, G M, F G, A P, L R, A S, M J.Clear Cell Renal Cell Carcinoma with Metastasis to the Thyroid. Appl Radiol. 2021; (5):50-52.
September 10, 2021