Chronic Periaortitis Mimicking Aortic Intramural Hematoma
Images

Case Summary
An elderly patient with a history of hypertension, hyperlipidemia, and type II diabetes presented initially for gastroenterology evaluation. The patient reported a remote history of jaundice prompting exploratory laparotomy, cholecystectomy, and partial liver resection in another country, with unclear underlying pathology. Records were not available.
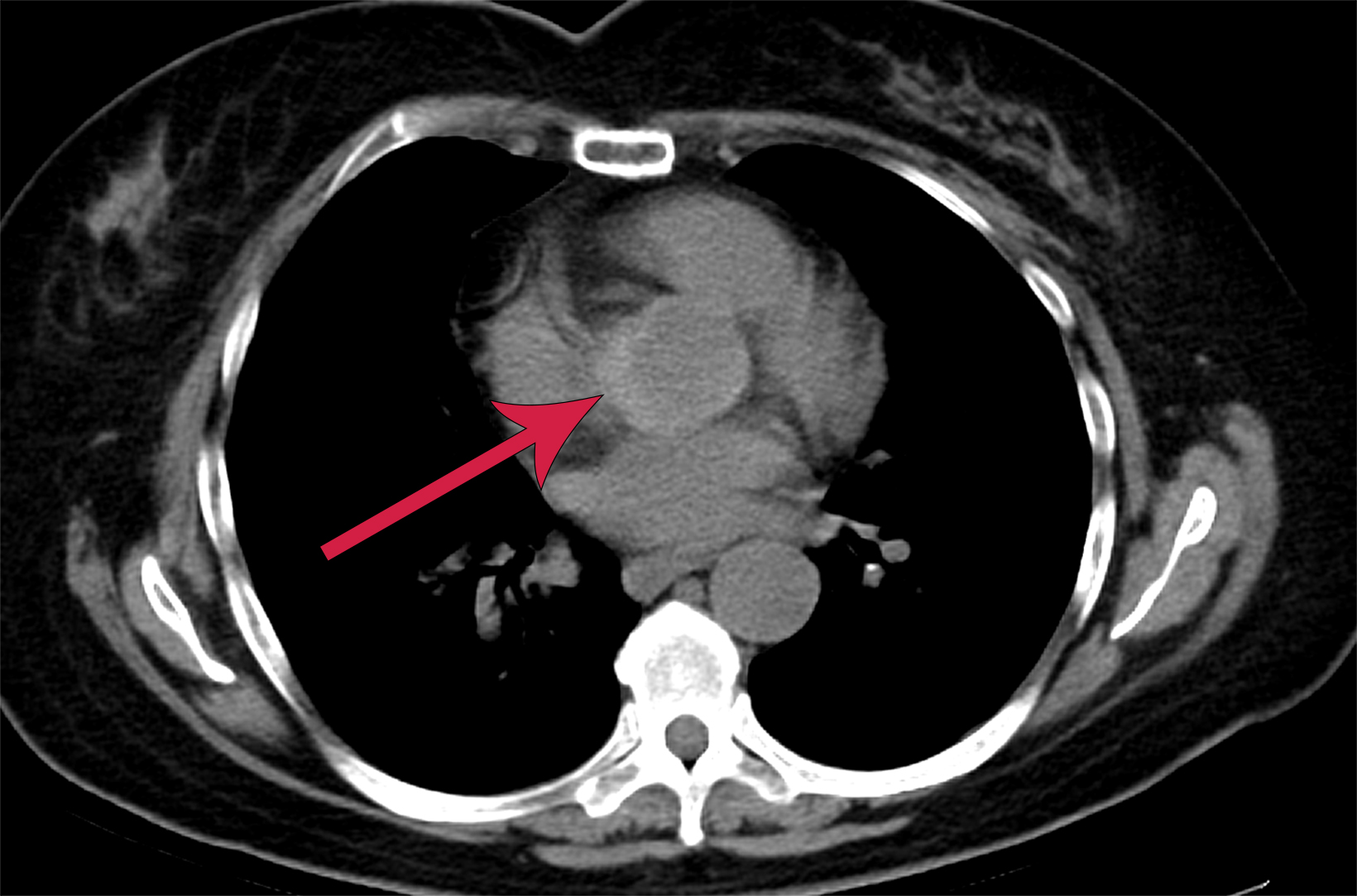
To guide further treatment, the gastroenterology service requested abdominal CT with and without contrast. The study demonstrated postsurgical changes in the liver without acute abdominal findings. However, the included portion of the lower chest incidentally revealed a crescentic hyperdensity surrounding the proximal aorta, concerning for intramural hematoma (Figure 1). Computed tomography angiography (CTA) of the chest was subsequently performed.
Imaging Findings
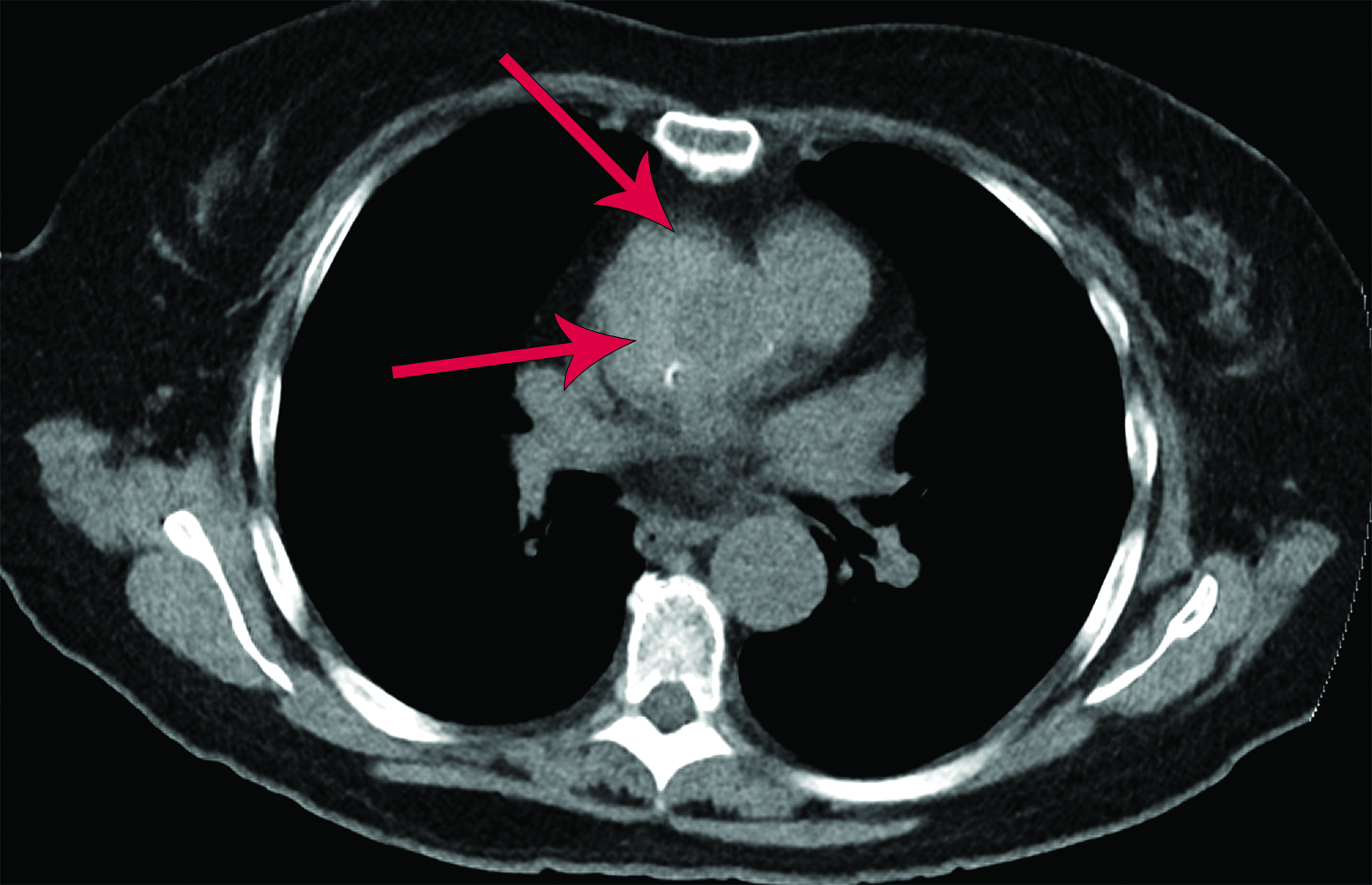
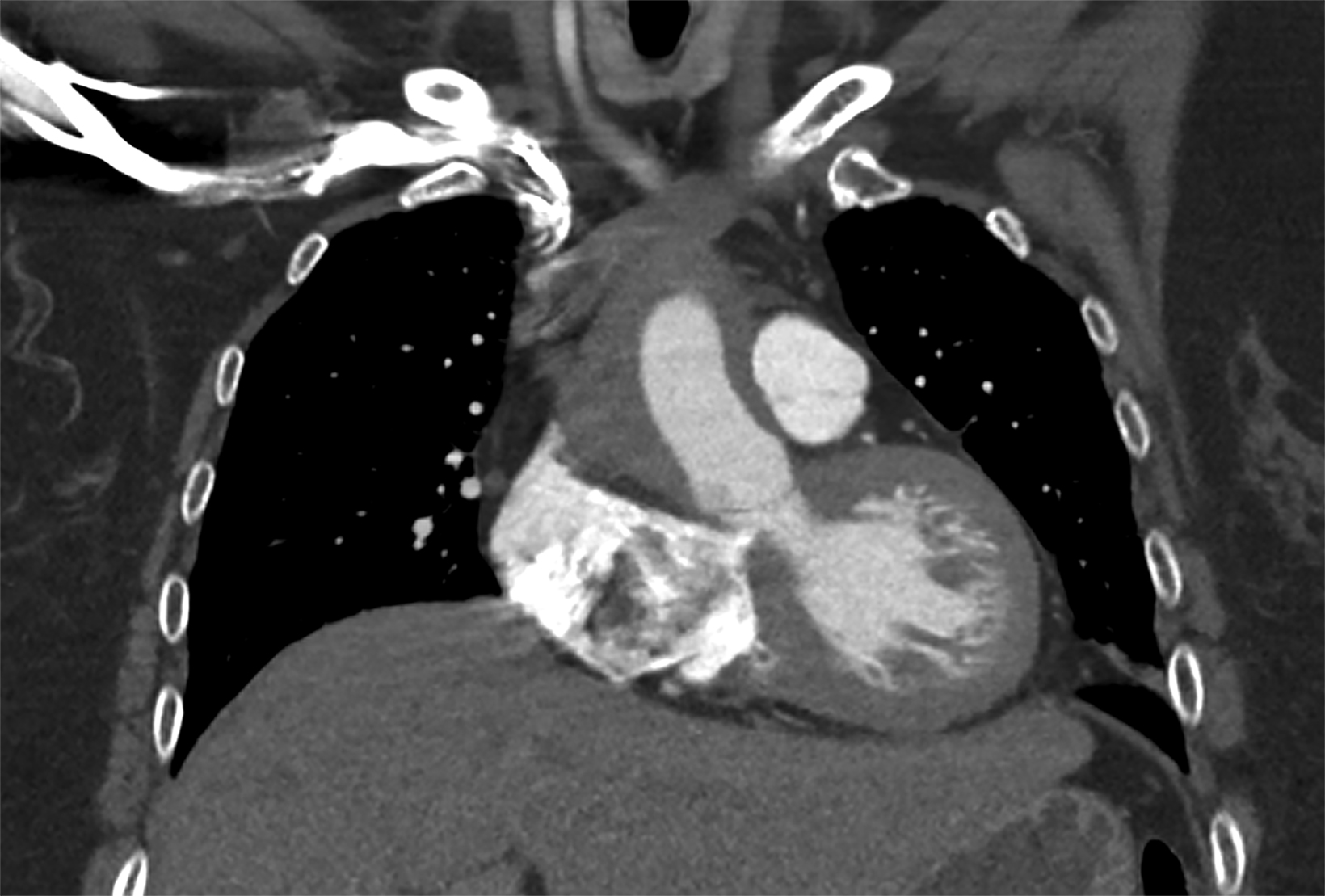
The chest CTA revealed eccentric, lobulated tissue encasing the aorta from the root through the great vessels extending to the descending aorta. The tissue was hyperdense on noncontrast images, measuring 58-60 Hounsfield units, and contained several calcifications. The findings were concerning for a type A intramural hematoma (IMH, Figure 2).
Diagnosis
Chronic periaortitis.
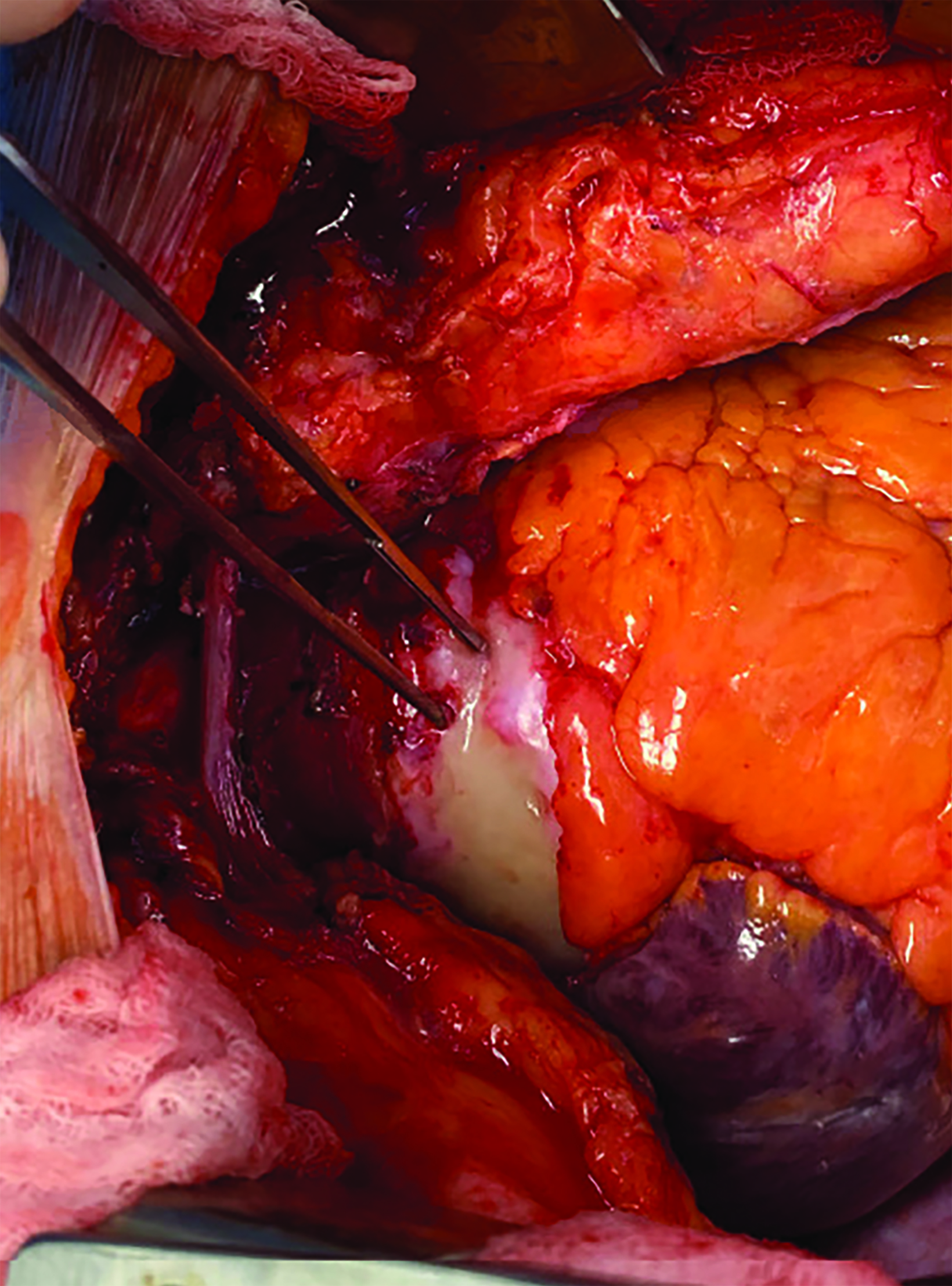
The patient underwent surgery for presumed type A IMH but instead was found to have rubbery, white tissue encasing the aorta. Biopsy revealed densely fibrotic tissue with plasma cells.
Discussion
Chronic periaortitis (CP) is rare and most commonly described as involving the infrarenal descending aorta and iliac arteries. The spectrum of disease includes idiopathic retroperitoneal fibrosis, as well as inflammatory abdominal aortic aneurysms. However, this process has increasingly been noted to involve the thoracic aorta.
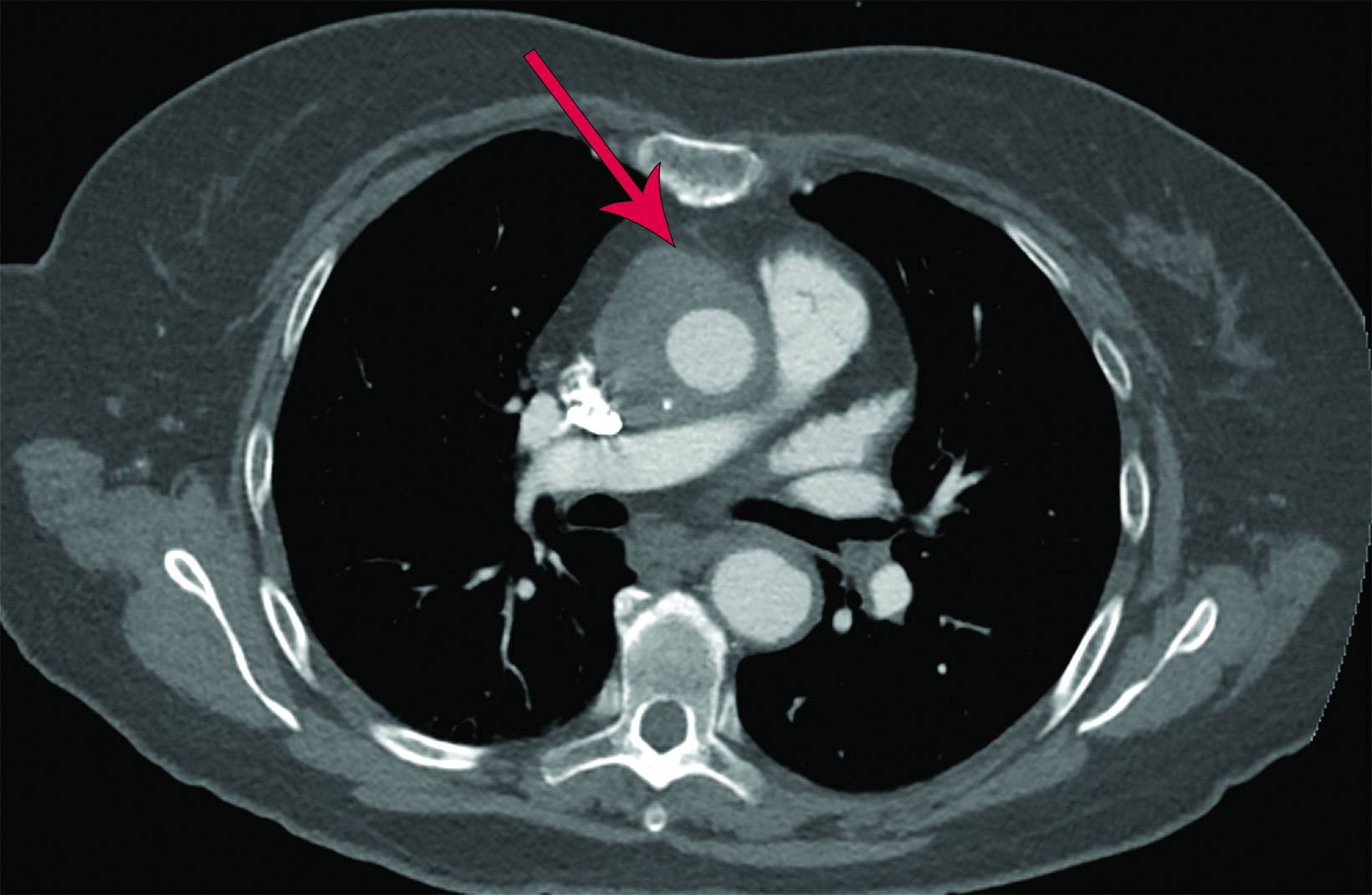
This disorder presents a diagnostic conundrum, as the imaging findings are hard to ignore as a type A IMH. However, the patient denied ever having symptoms of an acute aortic syndrome. Given the possibility of progression to frank rupture or dissection, the patient was taken to surgery, but instead of an IMH, “a shiny white very firm rubbery tissue that could best be described as resembling cartilage” was encountered as described in the operative report (Figure 3). Biopsies of the periaortic tissue and an aorticopulmonary window lymph node revealed densely fibrotic tissue with chronic inflammation, including plasma cells. Additional special and immunohistochemical stains were performed, the results of which were negative for spirochetes, with only a minor subset positive for IgG4 (<40%), which was considered to be insufficient evidence for IgG4-related disease.
Chronic periaortitis has been postulated to reflect an exaggerated inflammatory response to atherosclerotic plaque antigens.1 Limited studies exist regarding this condition, however, and its exact etiology remains unconfirmed. Much of the literature is supported by research about other periaortic conditions. A similar autoimmune process affects patients with IgG4-related disease or fibrosing mediastinitis,2 which supports an autoimmune etiology. Thoracic involvement has been described in several studies.1,3 In a review by Palmisano, et al, of 153 patients with CP documented by abdominal imaging, 36% were also noted to have thoracic involvement.3
In the same study, the patterns of large thoracic artery involvement mimicked findings seen in other large vessel inflammatory diseases such as giant cell arteritis and temporal arteritis. They compared pathology from patients with inflammatory conditions involving the periaortic abdominal aorta, such as retroperitoneal fibrosis, as well as those with thoracic involvement with or without concurrent abdominal involvement.
Comparison of the two subgroups revealed similar biopsy findings in thoracic and abdominal involvement, namely adventitial inflammation.3 These findings were also present in giant cell and temporal arteritis, suggesting that thoracic aortic involvement may reflect a large-vessel inflammatory disease3 and be a primary inflammatory or autoimmune disorder.
Mainstays of treatment are inflammation- or immune-modulating medications. Our patient remained asymptomatic, did not show progression on short-term follow-up, and continues to be managed conservatively.
Conclusion
Recognizing the imaging pattern of thoracic aortic intramural hematoma is important , especially in the setting of acute aortic syndrome. Any crescentic hyperdensity surrounding the ascending aorta should prompt further imaging and/or surgical evaluation. This case highlights a rare mimic of this life-threatening condition and demonstrates how much overlap can exist between certain conditions. Furthermore, this case presents a potential link to other periaortic vascular diseases and may be a topic of future study in radiology and rheumatology.
References
Citation
A K, T Y.Chronic Periaortitis Mimicking Aortic Intramural Hematoma. Appl Radiol. 2023; (3):40-42.
May 5, 2023