Breast Leiomyoma
Case Summary
A middle-aged, asymptomatic patient presented for routine screening mammography.
Imaging Findings
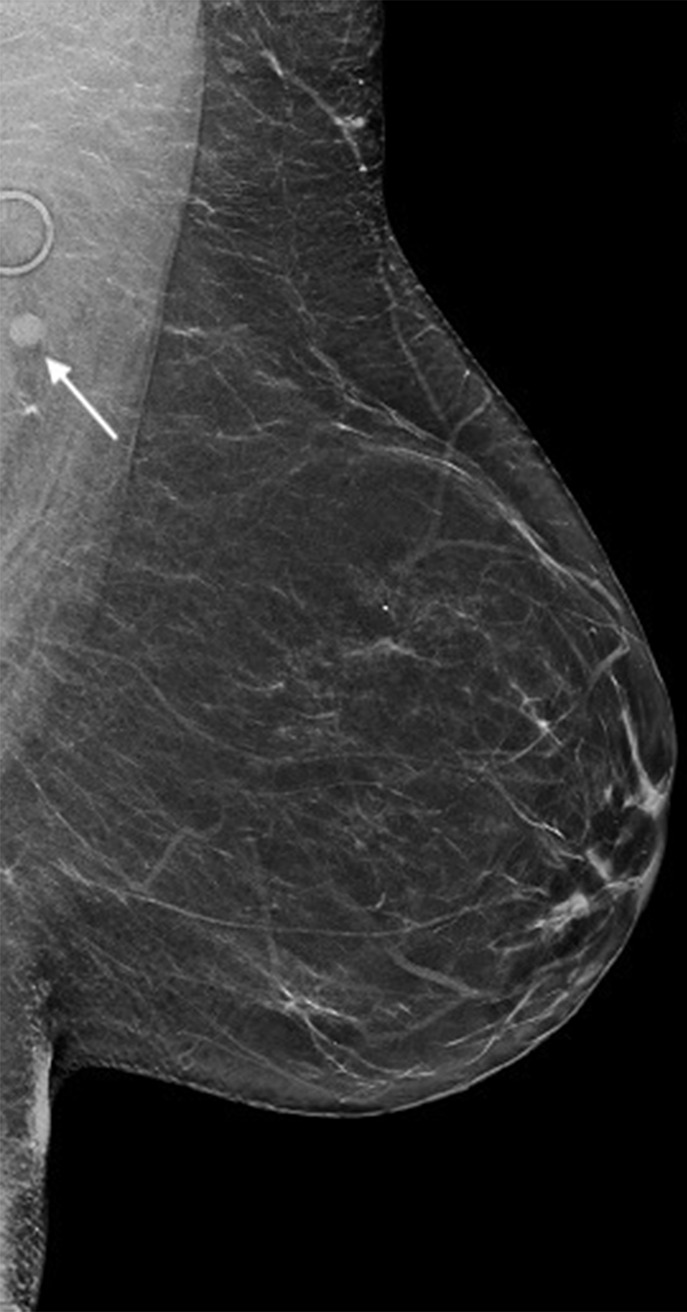
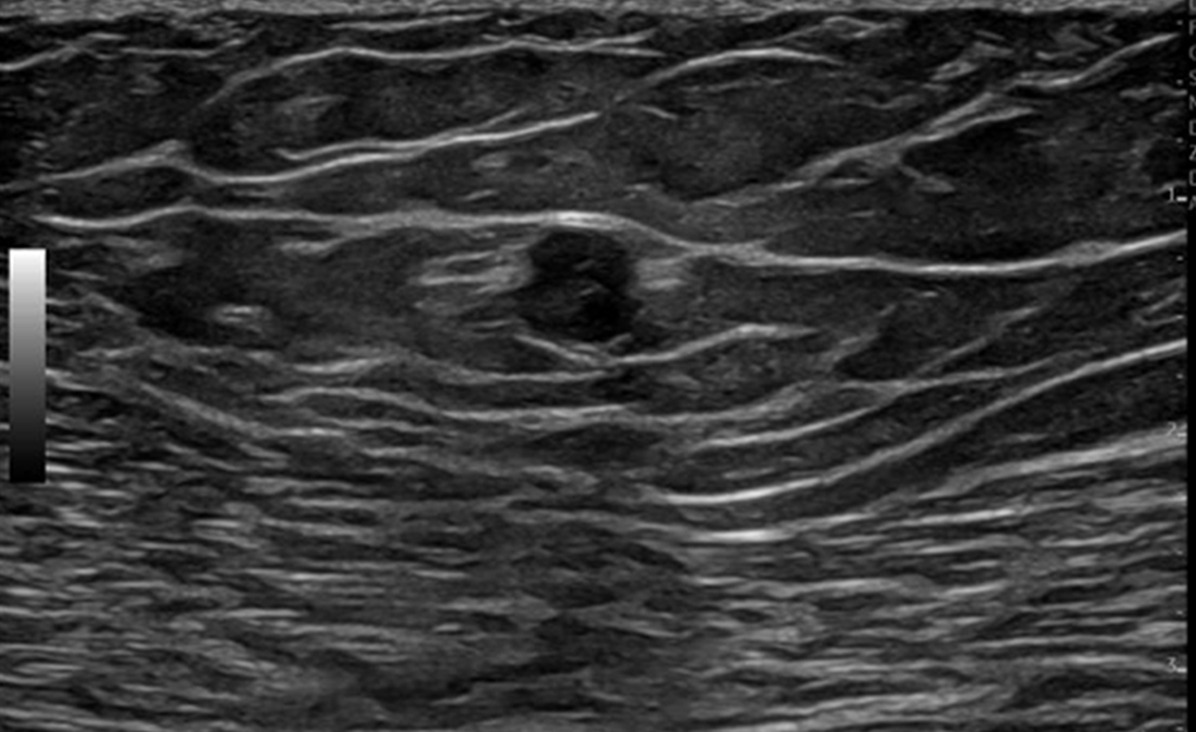
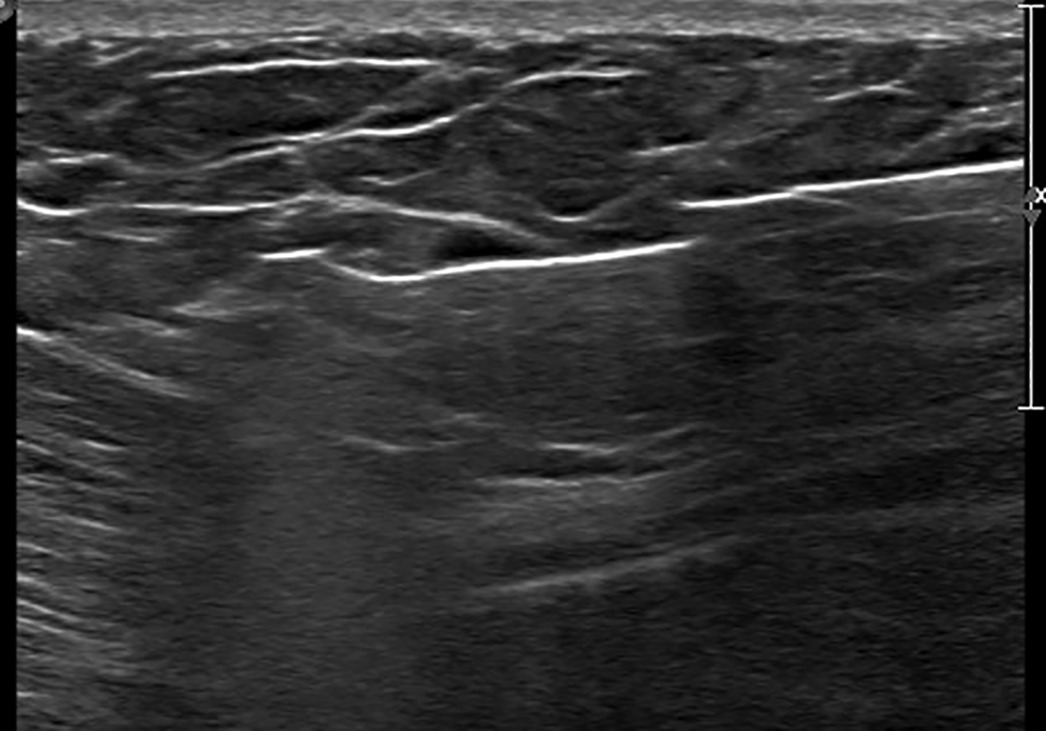
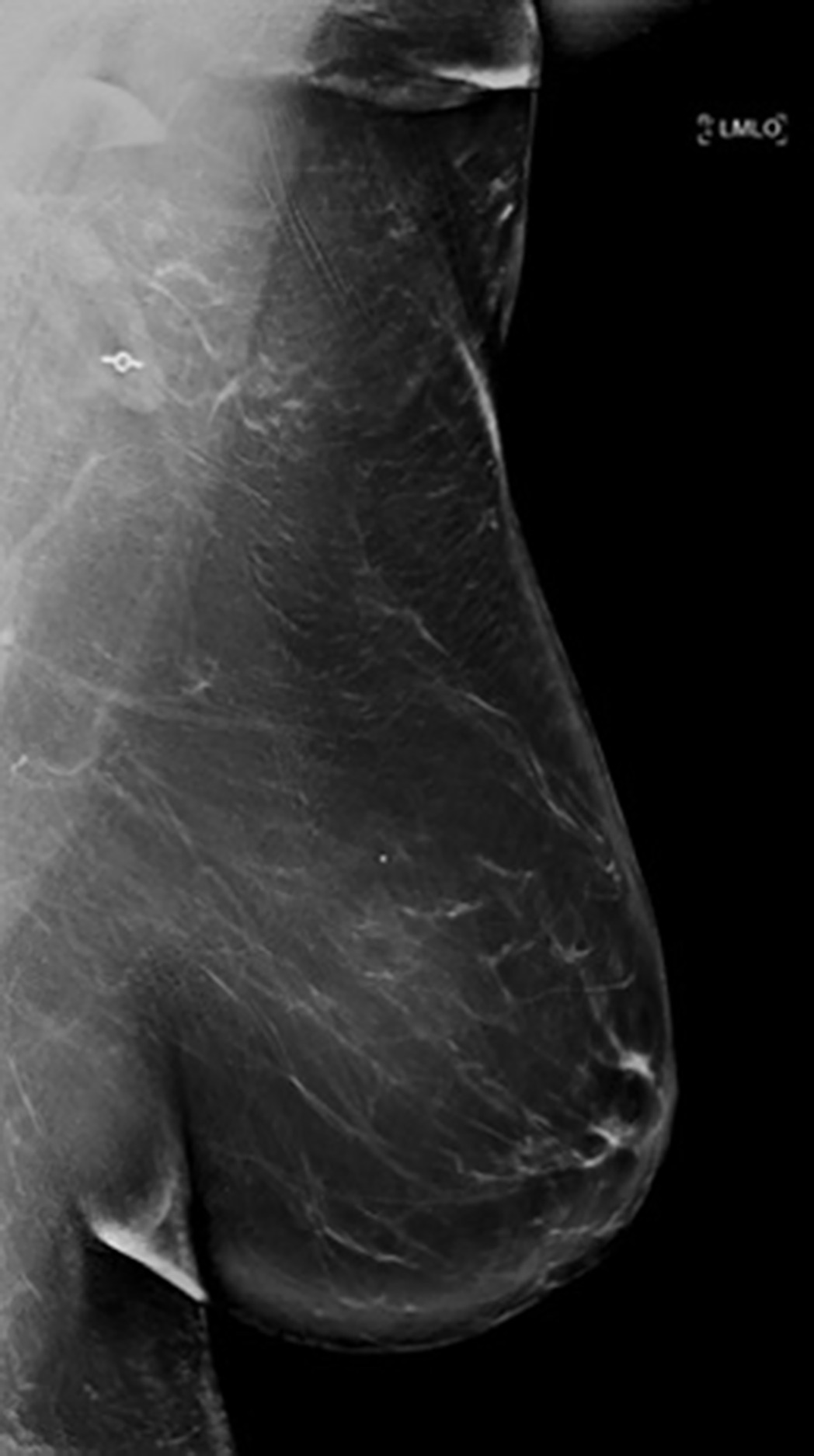
Screening mammogram of the left breast ( Figure 1 ) demonstrated an asymmetry in the posterior, upper quadrant on the mediolateral oblique (MLO) view. On subsequent tomosynthesis images, this was localized to the posterior, upper-inner quadrant of the left breast. Diagnostic mammogram ( Figure 2 ) demonstrated a 6 mm round asymmetry in the posterior upper-inner left breast, which appeared more consistent with a circumscribed mass. Diagnostic US ( Figure 3 ) revealed a corresponding 6 × 5 × 5 mm round, hypoechoic mass with some angular margins at the 11 o’clock position in the left breast, 12 cm from the nipple. The mass was assessed as BI-RADS 4, suspicious for malignancy, and US-guided biopsy was recommended. US-guided biopsy ( Figure 4 ) adequately sampled the mass with postprocedure mammography ( Figure 5 ), demonstrating appropriate positioning of the biopsy clip.
Screening mammogram mediolateral oblique view demonstrates an asymmetry (arrow) in the posterior upper-left breast.
Spot compression mediolateral oblique view with tomosynthesis demonstrates a 6 mm circumscribed round asymmetry (arrow) in the posterior upper-inner left breast.

US image shows a 6 × 5 × 5-mm round hypoechoic mass with some angular margins at the 11:00 position, 12 cm from the nipple.
US-guided biopsy image demonstrates sampling of the mass.
Postprocedure mammogram shows appropriate positioning of the biopsy clip.
Diagnosis
Leiomyoma of the breast.
The differential diagnosis for a round, hypoechoic mass in the posterior breast includes fibroadenoma, intramammary lymph node, complicated cyst, papilloma, phyllodes tumor, sarcoma, metastatic malignancy, and schwannoma.
Discussion
Leiomyomas are benign, nonepithelial neoplasms. While most often associated with the uterus and sometimes with the small bowel and esophagus, they rarely occur in other organs.1 Leiomyomas of the breast are very rare and predominantly seen in female patients aged 40 to 60, with only a few published case reports.2 Most breast leiomyomas are peri-areolar, with peripheral or deeper parenchymal lesions being extremely rare.1, 2 Their etiology is largely unknown and are theorized to arise from embryological displacement of the areolar, capillary, or subcutaneous smooth muscle cells of the breast, with subsequent overgrowth and transformation.3
Case reports and literature reviews describe imaging findings of mammary leiomyomas to be relatively nonspecific, with the most similarity shared with fibroadenomas.2, 3 They usually appear as circumscribed, round or oval homogeneous masses on mammography, and circumscribed homogeneous solid hypoechoic masses on US.4, 5 In this case, based on the imaging features and the posterior upper location on the initial 2D synthesized MLO view, the lesion could have easily been mistaken for an intramammary lymph node, a benign BI-RADS II finding, and the patient would not have been called back for diagnostic imaging.6 However, subsequent tomosynthesis images localized the mass to be more medial, which was further confirmed on the diagnostic mammogram and US. This demonstrates the importance of using a multimodal approach for precise localization to better characterize and diagnose breast lesions.7
Leiomyosarcomas are rare, malignant, mesenchymal tumors showing smooth muscle differentiation. Most often they are found in the abdomen or uterus, and they can be aggressive.8 Leiomyosarcomas of the breast are extremely rare, and it is worth noting that they have been seen in the peripheral and deep-breast parenchyma, which is uncommon for benign leiomyomas.3, 4 Breast leiomyosarcomas can often be mammographically and sonographically indistinguishable from a leiomyoma as they are typically circumscribed and slow growing.4, 9
Currently, the definitive diagnostic test for breast leiomyomas/sarcomas is tissue sampling. While uterine leiomyomas are often distinguished from uterine leiomyosarcomas on MRI,8 little has been published on MR features of breast leiomyomas. They have been described in the limited case reports as circumscribed masses intermediate to high signal on T2-weighted images and persistent enhancement on dynamic postcontrast images.2, 10 MRI may not be helpful to distinguish leiomyomas from leiomyosarcomas or other breast masses as features are nonspecific and most lesions being too small to definitively characterize.2 Thus, tissue sampling remains the preferred tool for diagnosis of breast leiomyomas/sarcomas.
Owing to their low prevalence, no standard guidelines have been established for the management of leiomyomas. However, it is theorized that they can be treated similarly to leiomyomas of other organs based on their pathological similarity.1, 3 The accepted treatment is local resection with free margins due to the potential of leiomyomas to continually grow, unlike most other benign lesions.3 In a literature review of 20 breast leiomyoma case reports by Brandão et al, a majority of the leiomyomas were resected with free margins, with a few patients opting for mastectomies.2 In well-sampled, asymptomatic cases, surveillance is also considered a reasonable approach.10
Conclusion
Leiomyomas of the breast are very rare and typically have nonspecific imaging features that most closely mimic fibroadenomas. Typically breast leiomyomas are found in the peri-areolar breast tissue instead of in the deeper, peripheral breast parenchyma, as in this case. This case also highlights the importance of using a multimodal approach to achieve precise localization, which can better characterize and diagnose breast lesions. Accurate diagnosis of leiomyomas is key, as they are often mammographically and sonographically indistinguishable from leiomyosarcomas.
References
Citation
Puchhalapalli K, Wadhwa A, Dykstra D, Cherian S.Breast Leiomyoma. Appl Radiol. 2025; (1):1 - 3.
doi:10.37549/AR-D-24-0054
February 12, 2025