Breast Granular Cell Tumor
Case Summary
A middle-aged adult with a complex medical history, including diabetes mellitus, osteoporosis, and previous bilateral salpingo-oophorectomy for stated malignancy, presented for overdue routine breast screening.
Imaging Findings
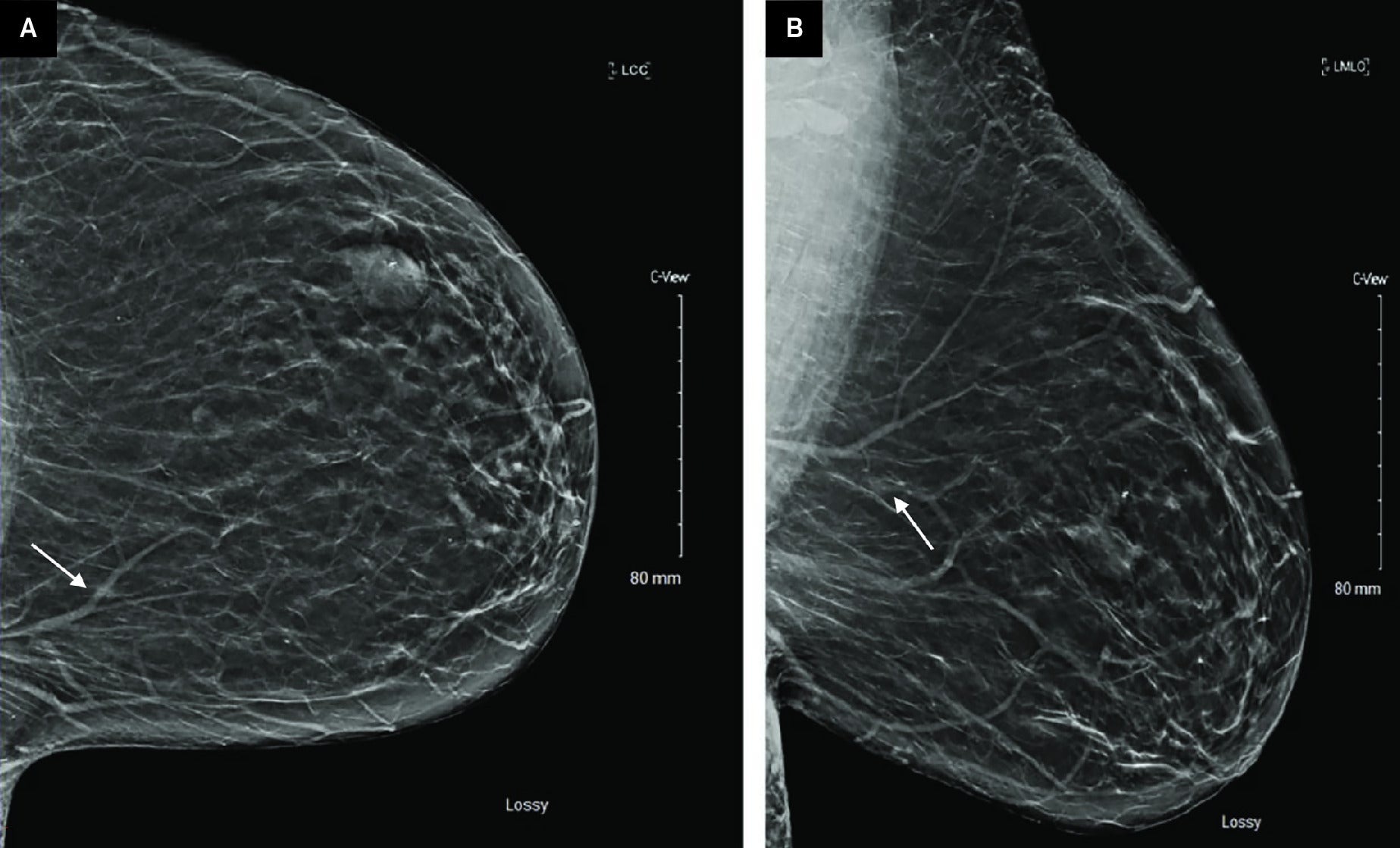
Screening full-field digital mammography with digital breast tomosynthesis (DBT) in craniocaudal (CC) and mediolateral oblique (MLO) projections demonstrated a 0.6-cm focal asymmetry in the upper inner left breast, posterior depth ( Figure 1 ). An additional previously biopsied fibroadenoma in the left breast with biopsy marker was stable.
Screening full-field digital mammography with DBT of the left breast in the CC (A) and MLO (B) projections demonstrates a focal asymmetry in the left breast upper inner quadrant, posterior depth (arrows). An additional stable fibroadenoma in the upper outer left breast, middle depth (arrowhead)
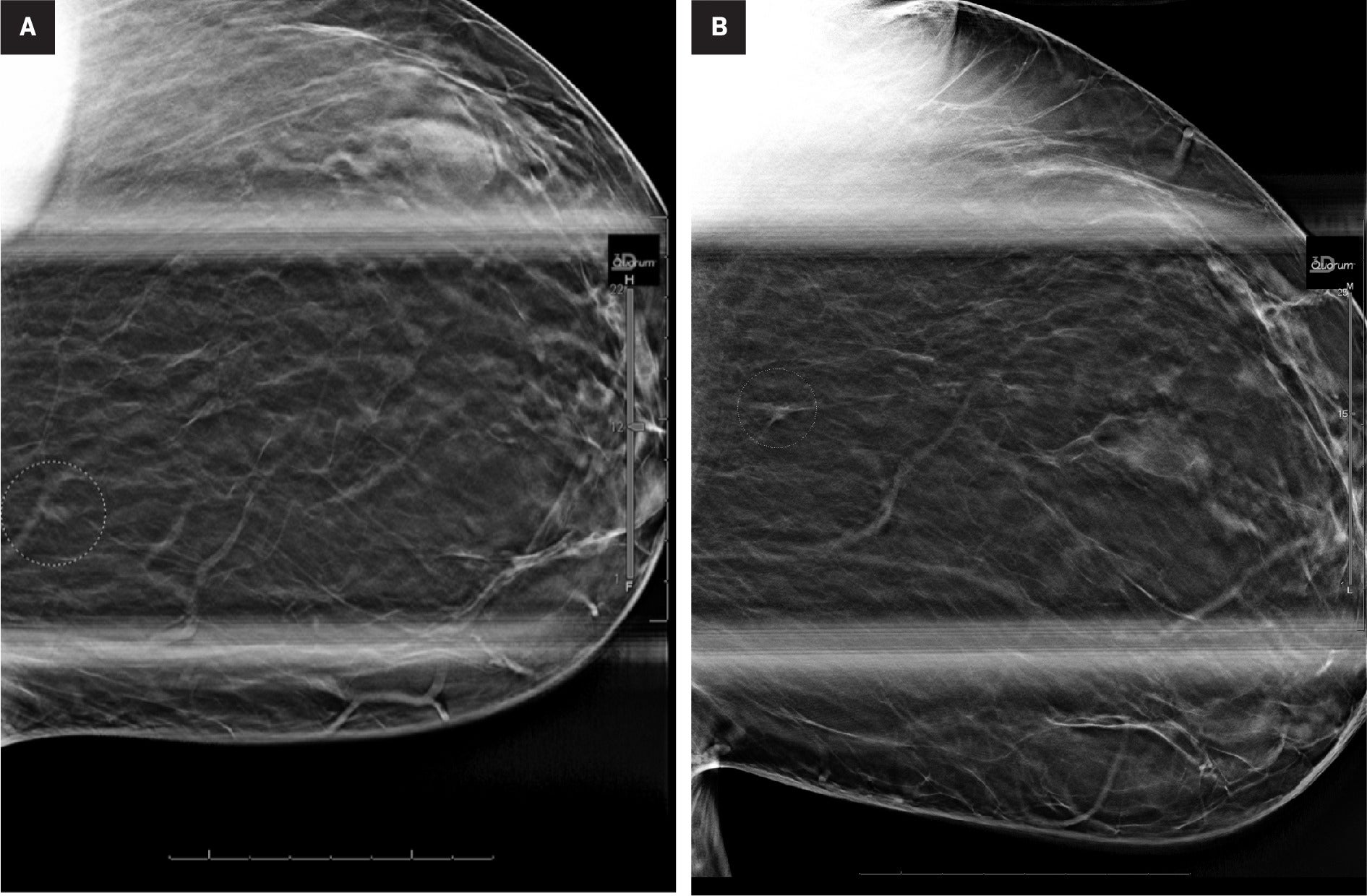
The patient was called back for diagnostic CC and MLO spot compression mammographic views with DBT, which confirmed the presence of a 0.6-cm focal asymmetry in the upper, inner left breast, posterior depth. ( Figure 2 )
Diagnostic spot compression views with DBT in the CC (A) and MLO (B) projections confirm a focal asymmetry in the upper inner left breast, posterior depth (circles)
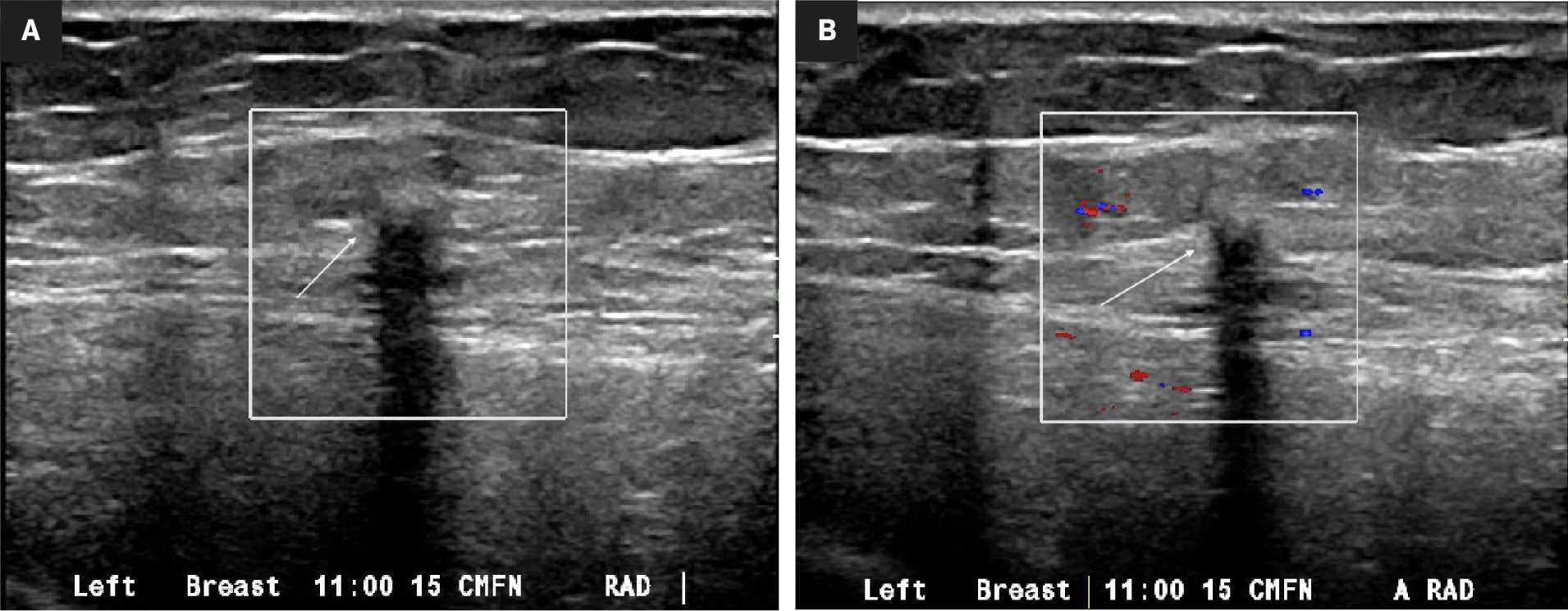
Targeted diagnostic ultrasound of the left breast demonstrated a 0.5 × 0.4 × 0.3 cm hypoechoic mass with indistinct margins and minimal associated internal vascular flow at the 11 o'clock position, 15 cm from the nipple, corresponding to the mammographic finding ( Figure 3 ), and assessed as BI-RADS 4 (suspicious). Ultrasound-guided core needle biopsy was performed with clip placement, confirming mammographic correlation.
Targeted gray scale (A) and color Doppler (B) ultrasound demonstrates an irregular hypoechoic mass with posterior acoustic shadowing at 11 o'clock, 15 cm from the nipple (arrows)
Diagnosis
Granular cell tumor (GCT), negative for in situ or invasive carcinoma.
The gross pathology specimen after localized surgical excision demonstrated an ill-defined, firm, homogeneous, gray-white, and yellow mass measuring 1.5 × 1.2 × 1 cm. Microscopic examination revealed infiltrating sheets and cords of polygonal bland cells with relatively well-defined cell borders, abundant eosinophilic granular cytoplasm, and round/oval nuclei surrounded by collagenous stroma. Immunohistochemistry showed that the tumor cells were positive for SOX10, S-100, and CD68, while they were negative for AE1/AE3, CAM5.2, CD163, and MART-1, supporting the diagnosis of GCT.
Discussion
Granular cell tumors in the breast are rare, typically benign, and can often mimic malignant lesions both clinically and radiologically. They present a diagnostic challenge because they may exhibit features similar to breast carcinomas, such as irregular margins and heterogeneous echo patterns on ultrasound. Studies suggest that the incidence of these tumors in the breast is low, accounting for approximately 5%-8% of all GCTs.1
Granular cell tumors typically present as firm, usually non-tender masses and may be found incidentally on routine mammograms or during physical examinations. They can vary in size and are often mobile unless they are located deep and adherent to the chest wall or overlying fascia, where they may feel fixed.1
GCTs may grow slowly without significant change over time. Any rapid change in size or newly associated symptoms should prompt further investigation to rule out malignant transformation or other complicating factors. Importantly, GCTs can occasionally be associated with pain or discomfort if they impinge on nerves or have a deep location affecting muscle or connective tissue layers.2, 3 They do not usually present with systemic symptoms unless they are part of a rare malignant variant. However, patients with GCTs can present with skin changes such as thickening or dimpling over the tumor, which can further complicate the clinical picture, suggesting more aggressive underlying pathology.1
Mammographically, GCTs usually present as high-density masses with irregular or spiculated margins. These characteristics overlap significantly with those of invasive breast carcinomas, making it difficult to differentiate between the two based solely on mammographic findings.1 Occasionally, GCTs may appear as circumscribed oval masses, mimicking benign conditions such as fibroadenomas.1
On ultrasound, GCTs are typically hypoechoic masses with indistinct or spiculated margins and may exhibit posterior acoustic shadowing as in malignancies, thus necessitating needle biopsy to achieve a definitive diagnosis.3
While not always utilized, MRI can provide additional detail, particularly in complex cases. GCTs on MRI generally appear as well-defined masses with low signal intensity on T1-weighted images and variable signal intensity on T2-weighted images. They may enhance uniformly or heterogeneously after contrast administration.1
These details emphasize the importance of a comprehensive diagnostic approach, including imaging and biopsy, to distinguish GCTs from more aggressive breast lesions.
Granular cell tumors arise from Schwann cells and are histologically defined by polygonal cells with granular eosinophilic cytoplasm, arranged in clusters or sheets. The cytoplasmic granules, indicative of lysosomal origin, are PAS-positive and diastase-resistant. Immunohistochemically, GCTs are consistently positive for neural markers and negative for epithelial and melanocyte markers, helping to distinguish them from other neoplasms.
Most GCTs are benign, but the risk of recurrence or rare malignant transformation makes thorough surgical management essential.1 The standard treatment is wide local excision with clear margins to prevent recurrence, which can range from 2%-8%.2, 3 Clear margins and meticulous surgical techniques are crucial for minimizing recurrence. In rare cases of malignant GCTs, management may require additional therapies similar to those used for breast cancers, highlighting the importance of precise pathological assessment and follow-up.3
Conclusion
Granular cell tumors of the breast, while rare, present a significant diagnostic challenge due to their ability to mimic more aggressive malignancies. This case emphasizes the importance of a thorough diagnostic workup, including advanced imaging and biopsy, to differentiate GCTs from other breast pathologies. Wide local excision with clear margins is crucial to prevent recurrence, and regular follow-up is necessary to monitor for any signs of recurrence. A multidisciplinary approach is essential for effective management and favorable patient outcomes. This case also highlights the importance of considering GCTs in the differential diagnosis of breast masses with suspicious imaging features, ensuring comprehensive care, and accurate diagnosis.
References
Citation
Taghi-Zadeh E, Choudhury MSR, Shaar M, Singh E.Breast Granular Cell Tumor. Appl Radiol. 2025; (4):1 - 3.
doi:10.37549/AR-D-25-0094
August 1, 2025