Bilateral Abdomino-Scrotal Hydrocele
Images
Case Summary
An infant presented with scrotal swelling that was present since birth. According to the mother, the scrotal bulging was stable throughout the day. Physical examination revealed an uncircumcised penis with a large left inguinal inguino-scrotal hydrocele and a small right scrotal hydrocele. While the right testis was palpated easily, the left one could not be palpated, owing to the swelling. The reminder of the examination was unremarkable.
Imaging Findings
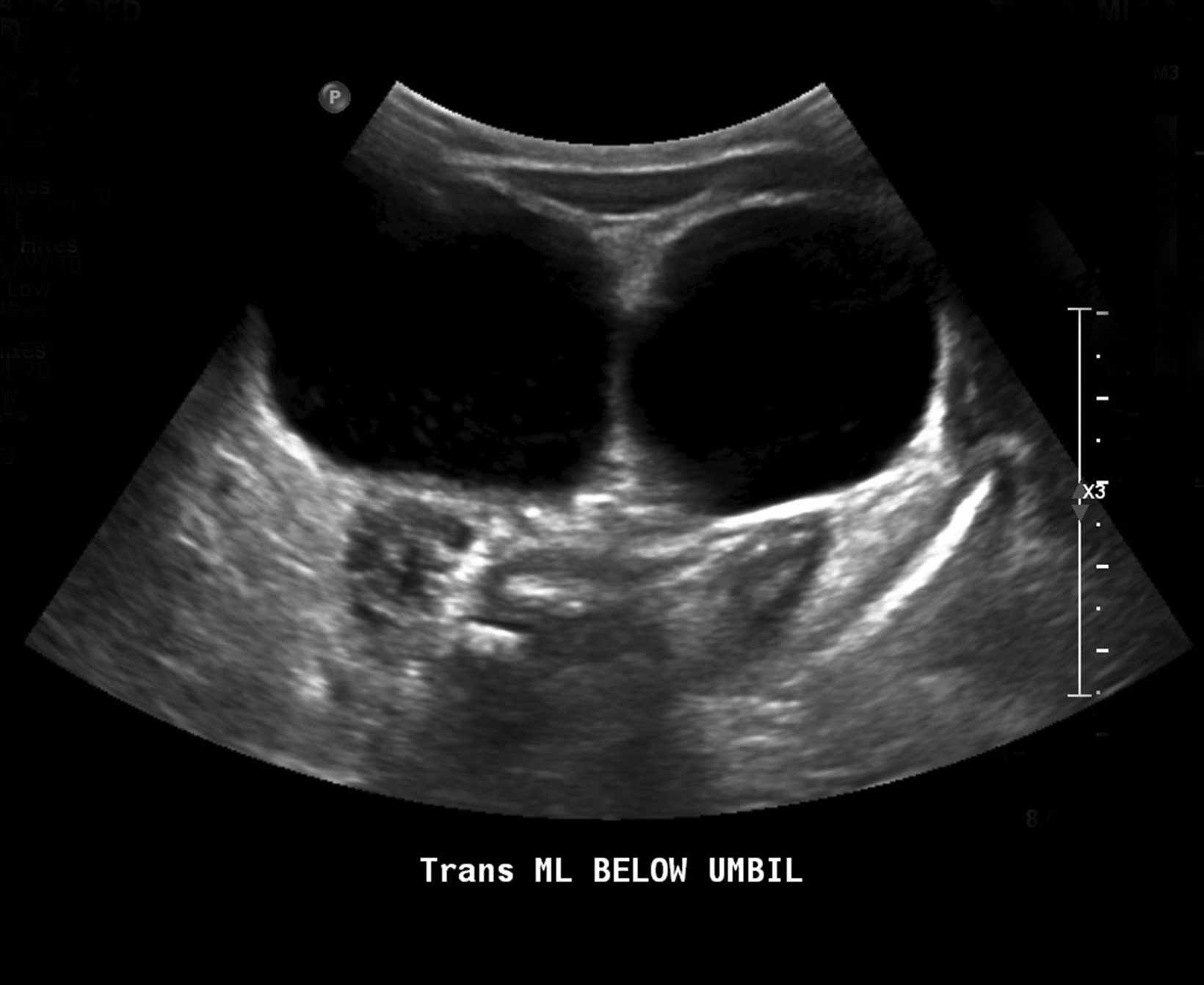
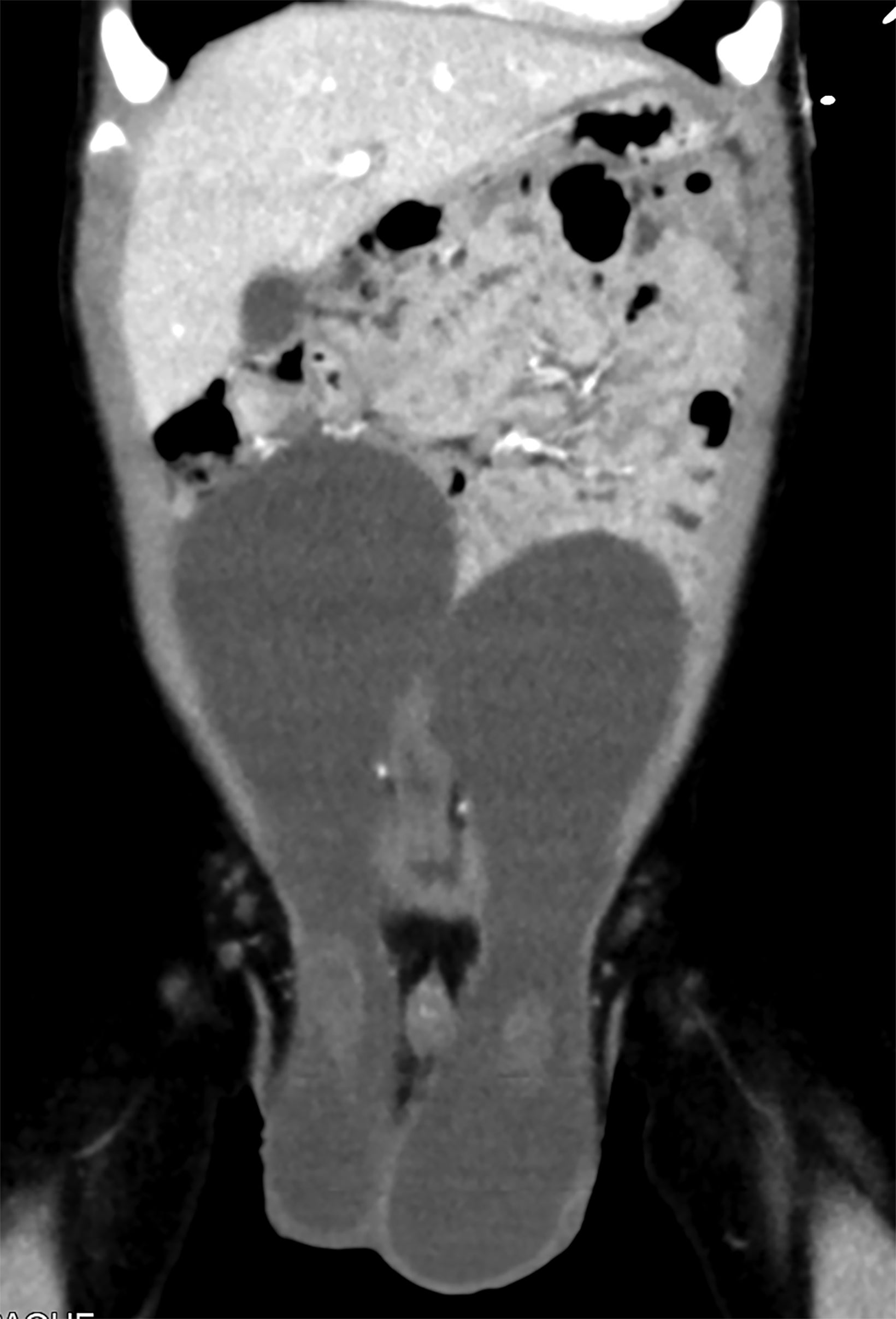
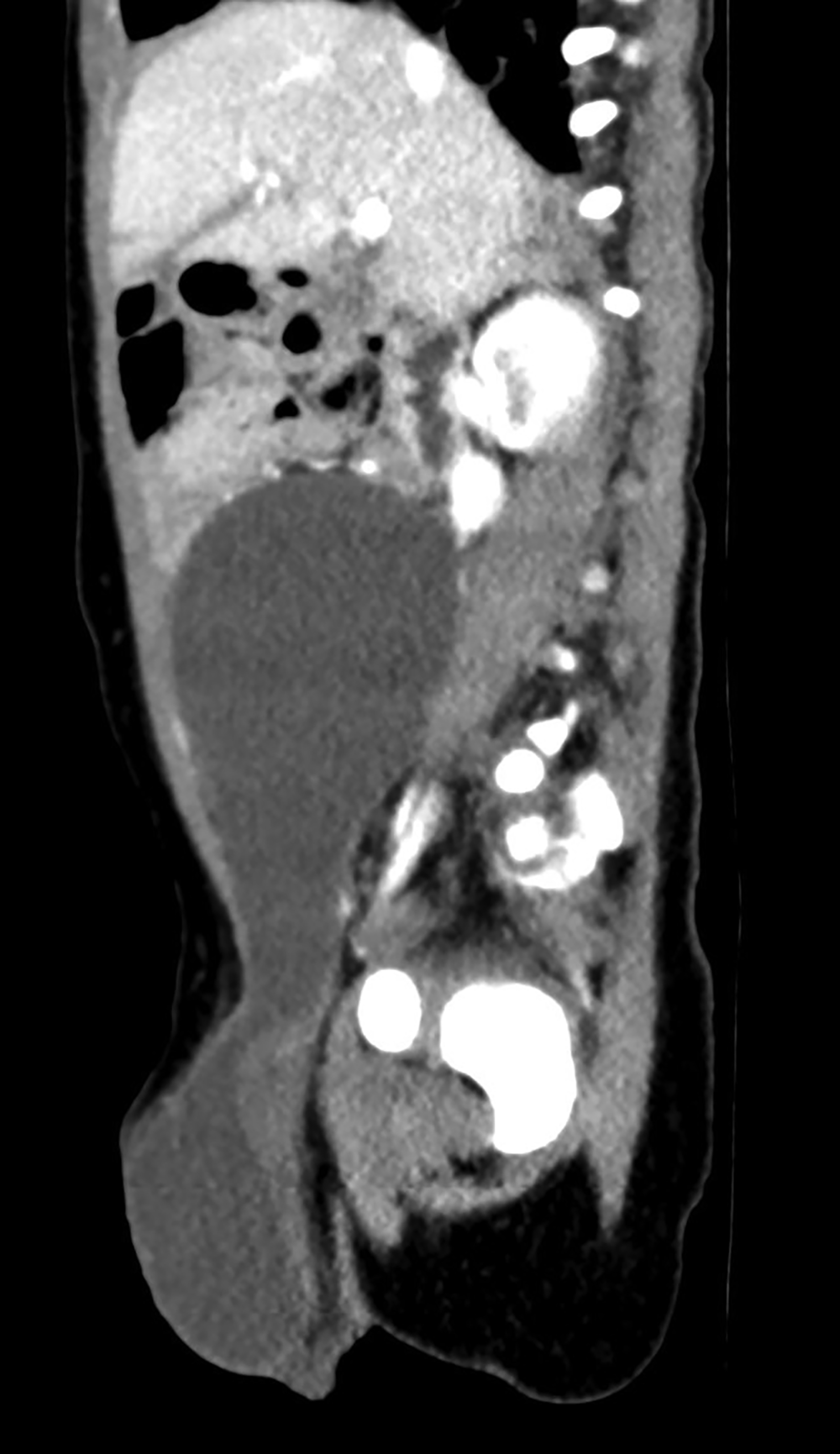
Scrotal ultrasound revealed bilateral large hydroceles extending through the inguinal canal. Abdominal ultrasound demonstrated bilateral large anechoic lesions that extended above the umbilicus level (Figure 1). Coronal and sagittal contrast-enhanced computed tomography (CT) images (Figure 2) of the abdomen and pelvis revealed large cystic lesions extending from the iliac fossae into the umbilical area with both testes in the scrotal sac.
Diagnosis
Bilateral abdomino-scrotal hydroceles
Discussion
Abdomino-scrotal hydrocele (ASH) is a rare entity that is responsible for 3.1% of all pediatric hydroceles.1 Bilateral ASHs are extremely rare.2 These hydroceles are characterized by a scrotal fluid-filled mass that expands across the internal inguinal ring into the extra-peritoneal cavity.1,2 Most ASHs are asymptomatic and usually present with scrotal swelling and abdominal mass. Owing to the mass effect and pressure, ASHs can be associated with rare complications such as hydronephrosis, rupture, and associated malignancy of the tunica vaginalis.3,4
The diagnosis of ASH is often clinical, through a detailed history and physical examination. Abdominal and scrotal ultrasound evaluation is usually used to confirm the diagnosis. Occasionally, contrast-enhanced CT or magnetic resonance imaging are utilized to better delineate the relation between ASH and the surrounding structures.1 Because the spontaneous resolution of ASH is rare, surgical correction of the hydrocele is recommended.5
The pathogenesis of ASH remains controversial, with multiple theories suggested in the literature. The most compelling theory proposes that ASH results from the cephalic extension of the scrotal hydrocele into the extraperitoneal space in the presence of high partial obliteration of processus vaginalis. This superior extension occurs when the scrotal intracystic pressure exceeds the intraperitoneal pressure, leading to the protrusion of tunica vaginalis through the inguinal ring into abdominal cavity.2,4,5
While open inguinal repair is considered the standard approach for correcting ASHs, laparoscopic techniques are increasingly used in this era of minimally invasive surgery to correct these anomalies.6 Most ASHs are repaired laparoscopically via either the extraperitoneal or intraperitoneal approaches. The extraperitoneal method uses two incisions, one at the umbilicus and one or two incisions at the lower abdomen. The intraperitoneal method uses three port incisions on the abdominal wall. The recurrence rate after laparoscopic repair is rare, ranging from 1.4% to 3.52%.6
Conclusion
ASH is a rare entity that is diagnosed clinically and confirmed with scrotal and abdominal ultrasound. Cross sectional imaging is occasionally used when the relationship between ASH and surrounding structures is unclear. Management and pathogenesis of ASH remain controversial. Laparoscopic repair is widely used to correct these hydroceles, which have a low rate of recurrence.
References
- Doudt AD, Kehoe JE, Ignacio RC, Christman MS. Abdominoscrotal hydrocele: A systematic review. J Pediatr Surg. 2016;51(9):1561-1564.
- Serels S, Kogan S. Bilateral giant abdominoscrotal hydroceles in childhood. Urology. 1996;47(5):763-765.
- Belman AB. Abdominoscrotal hydrocele in infancy: a review and presentation of the scrotal approach for correction. J Urol. 2001;165(1):225-227.
- Costantino E, Ganesan GS, Plaire JC. Abdominoscrotal hydrocele in an infant boy. BMJ Case Rep. 2017;2017.
- Avolio L, Chiari G, Caputo MA, Bragheri R. Abdominoscrotal hydrocele in childhood: is it really a rare entity? Urology. 2000;56(6):1047-1049.
- Jin Z, Wang F. Effectiveness of Laparoscopy in the Treatment of Pediatric Hydrocele: A Systematic Review. J Laparoendosc Adv Surg Tech A. 2018; 28(12):1531-1539.
Citation
SE A, S M, Almehmi.Bilateral Abdomino-Scrotal Hydrocele. Appl Radiol. 2022; (5):34-35.
August 31, 2022