Automated CT tool assesses bone mineral density
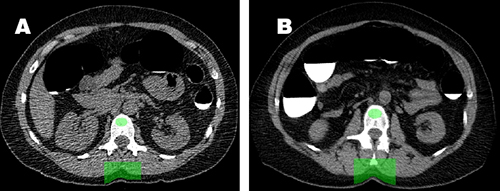
Axial image from initial CTC screening study (A) in a 50-year-old woman
shows placement of the automated BMD tool (green oval) in the trabecular
space of the L1 vertebral body. Image from follow-up CTC five years later
(B) shows interval decrease in L1 trabecular BMD, which still remains
within the normal range.
Radiologists from the National Institutes of Health (NIH) Clinical Center in Bethesda, MD, and the University of Wisconsin School of Medicine and Public Health in Madison, have developed a fully automated software program that can accurately estimate bone mineral density (BMD) from computed tomography (CT) scans performed for other diagnostic purposes. This CT-based, spinal trabecular BMD tool can identify patients with or at risk for developing osteoporosis who have not had a bone density screening exam or to supplement dual-energy X-ray absorptiometry (DXA) findings.
In the online edition of the Nov. 28 British Journal of Radiology, the physicians explain how the tool works, its validation process, and its utilization to assess BMD changes over time in a population-based study of over 1,600 individuals with more than one CT scan over time.
Low-radiation DXA is the modality of choice for bone density screening. It calculates areal bone density at regions of interest (ROI) which typically include the proximal end of the femur, lumbar spine, and distal end of the radius. However, body mass, degeneration, deformity, surgery, and the ROI can all affect exam accuracy.
Quantitative CT strongly correlates with BMD, but the manual process to acquire this data is laborious and impractical for osteoporosis screening. The automated BMD tool developed by Ronald M. Summers, MD, PhD, and his colleagues at NIH, and applied by Perry J. Pickhardt, MD, and colleagues at UW makes it possible to automatically add BMD data to an abdominal and/or pelvis CT scan report.
According to the radiologists, the tool initially segments the trabecular spine from CT images, extracting the spinal column and positioning into individual vertebrae. An oval ROI is placed in the middle transverse (axial) cross-sections of extracted L1 and L2 vertebrae. Mean HU values are calculated and converted to BMD estimates.
The study included 1,603 (52% female) consecutive adults with at least two CT colonography (CTC) studies between January 2004 and March 2017 at UW. These individuals were asymptomatic and ranged from 51 to 61 years of age at their initial CTC screening. The mean interval for subsequent screening was 6 years, but ranged from 1 to 12 years. More than 75% of the study cohort had not undergone DXA screening prior to their first CTC exam.
The BMD tool obtained L1 HU and BMD values in all 1,603 cases, although it failed on four cases, which were excluded. The annual rates of BMD loss peaked in women between ages 50-55, corresponding with menopause. Their overall mean annual BMD change was -2.0% per year. As with women, mean BMD decreased with men as they aged, but at a mean annual change of -1.0%.
“These data stress the potential importance and possible preventive opportunity for this accelerated BMD loss seen in the early post-menopausal period in females,” the researchers wrote. “Because these changes occur before the age of recommended osteoporosis screening, other interventions might be considered.”
“In general, abdominal CT scans provide a wealth of data beyond the specific clinical indication for imaging. With over 50 million adults undergoing abdominal CT each year in the United States, this provides an enormous opportunity for additional health screening,” Dr. Pickhardt told Applied Radiology. Dr. Summers said the NIH Office of Technology Transfer is managing commercialization of the tool.
Dr. Pickhardt also said that the team is actively exploring other uses of CT. “Beyond BMD, we are also investigating automated tools for assessing hepatic and visceral fat, muscle mass, and vascular calcification that will be able to provide a veritable virtual physical exam,” he said.
REFERENCE
- Pickhardt PJ, Lee SJ, Liu J, et al. Population-based opportunistic osteoporosis screening: Validation of a fully automated CT tool for assessing longitudinal BMD changes. Br J Radiol. Published online November 28, 2018. doi: 10.1259/bjr.20180726.
Citation
Automated CT tool assesses bone mineral density. Appl Radiol.
January 24, 2019