Atypical Teratoid Rhabdoid Tumor of the Oculomotor Nerve
Images

Brought to you by Guerbet.
Case Summary
An 8-year-old child with a history of attention deficit hyperactivity disorder, expressive language disorder, strabismus, and developmental delay. Patient initially presented to the emergency department with the following symptoms including restricted left eye movements (cranial nerve III palsy), ptosis, vomiting, and a 1-day history of headache. Initial magnetic resonance imaging (MRI) demonstrated a mass along the left oculomotor nerve (CN III), which was concerning for a schwannoma. The patient was discharged and scheduled for follow-up with ophthalmology and neurosurgery. The child's ptosis worsened, and she presented to the emergency department 3 weeks later, when a follow-up MRI revealed enlargement of the mass despite steroid treatment. A follow-up MRI at 4 weeks again revealed continued enlargement of the mass, and the patient underwent surgical resection of the mass.
Imaging Findings
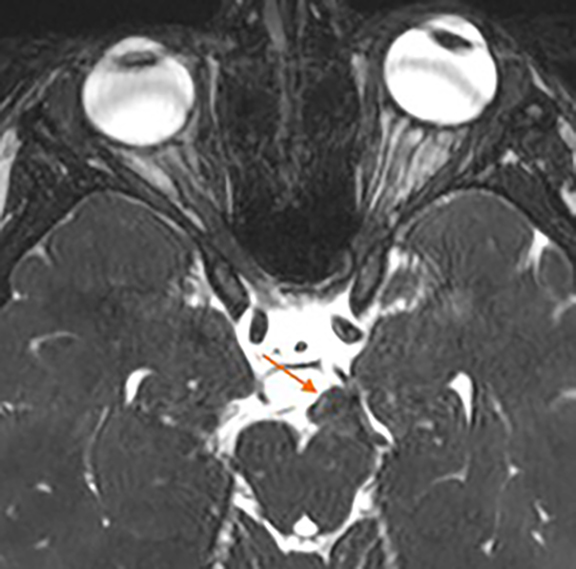
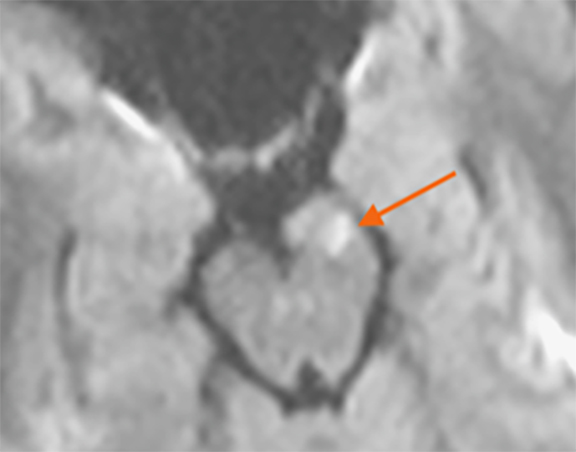
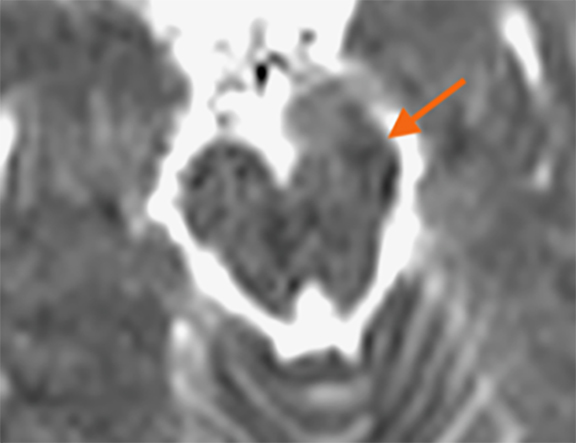
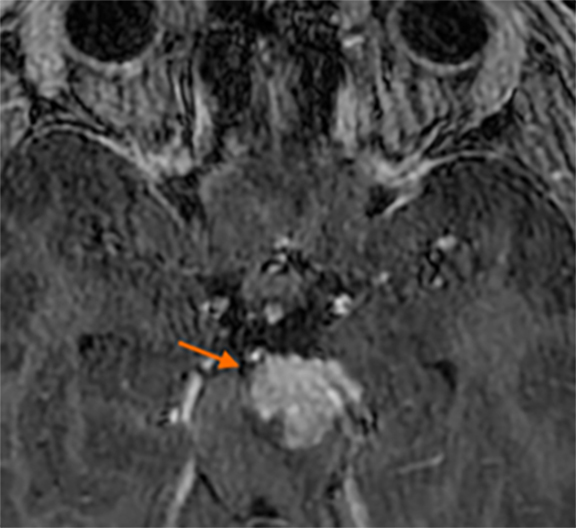
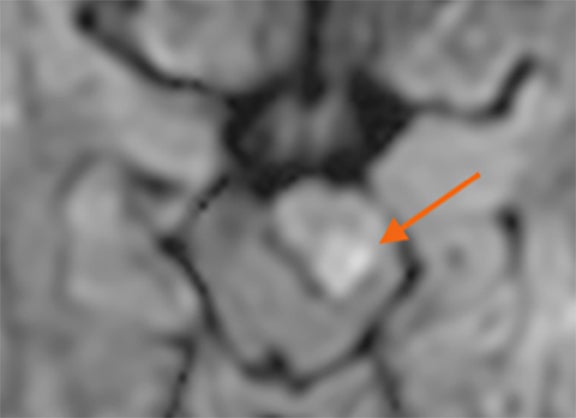
Initial MRI demonstrated a mass involving the cisternal segment of the left oculomotor nerve (CN III) in the midbrain (Figure 1). The mass demonstrated diffuse enhancement following intravenous administration of a gadolinium-based contrast agent (GBCA). The mass also correlated with areas of reduced diffusion on diffusion weighted imaging (DWI). Follow-up MRI revealed continuing enlargement of the same mass, as well diffuse enhancement, and areas of reduced diffusion at 3 and 4 weeks after presentation. There were no additional masses or abnormal leptomeningeal enhancement and the remainder of the brain and orbits appeared normal on MRI.
Diagnosis
Atypical teratoid/ rhabdoid tumor (ATRT; WHO IV)
Discussion
Atypical teratoid/ rhabdoid tumor is listed in the embryonal group on the most recent WHO 2016 classification of CNS tumors and is defined by alterations in either the INI1 gene or the rarer BRG1 gene.1 The tumor most commonly appears before age 3 years, with a median age of 24 months at diagnosis. Most have been described in the posterior fossa, including the brainstem; however, ATRT can present supratentorial and even as extra-renal rhabdoid tumors outside the central nervous system.2,3 This case describes an atypical location involving the oculomotor nerve (CN III).
There are three molecular subtypes of ATRT (sonic hedgehog [SHH)], TYR, and MYC), each having different behavioral and clinical characteristics.4 ATRT can also express ASCL1, a regulator of NOTCH signaling, which is more common in the SHH subtype and is correlated with supratentorial location and an improved 5-year overall survival.
MRI findings of ATRT classically describe a mass with reduced diffusion, heterogeneous to homogeneous enhancement, and necrosis. ATRT is similar to medulloblastoma on imaging; however, ATRT typically affects a younger age group. Metastatic disease is common and found in up to 25% of patients at initial presentation.
MR spectroscopy has shown promise in predicting the molecular subtypes, which can help predict therapeutic response. A higher Cr/Cho ratio and ml/Cho ratio in subtype 1 may correlate with the SHH subtype and ASCL1 expression. The ASCL1 is associated with the NOTCH target, which provides a favorable therapeutic target.
Cases of ATRT involving the oculomotor nerve are extremely rare.2 The similarity of this case to those in the literature is not only in the mass (involving CN III and showing diffuse enhancement after GBCA administration and areas of reduced diffusion), but also in the clinical presentation of ptosis and CN III palsy. Other masses that can involve CN III include schwannomas and low-grade gliomas, which do not commonly display reduced diffusion. Obtaining thin slice, post-contrast MRI sequences of a mass is important for further characterization and evaluation of leptomeningeal spread and post-contrast spine imaging for metastatic disease.
Balanced steady-state free precession (b-SSFP) sequences, such as constructive interference in steady-state (CISS) and fast imaging employing steady-state acquisition with phase cycling (FIESTa–c), permit high spatial resolution and high cerebrospinal fluid-to-soft tissue contrast.5 The b-SSFP sequences enable accurate detection of masses along cranial nerves; these masses can easily be missed, owing to their small size and challenging location within CSF, where other sequences can produce CSF flow artifacts.
Conclusion
A mass involving the oculomotor nerve displaying enhancement and reduced diffusion on MRI in the pediatric population (especially 3 years or younger) should include ATRT in the differential. ATRT is a high-grade tumor that can present in atypical locations. Familiarity with these atypical presentations can aid neuroradiologists in making an accurate diagnosis.
References
- Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):1-18. doi:10.1007/s00401-016-1545-1
- Oh, C. C., Orr, B. A., Bernardi, B., Garré, M. L., Rossi, A., Figà-Talamanca, L., Robinson, G. W., & Patay, Z. (2015). Atypical teratoid/rhabdoid tumor (ATRT) arising from the 3rd cranial nerve in infants: a clinical-radiological entity?. J Neurooncol, 124(2), 175–183. https://doi.org/10.1007/s11060-015-1787-0.
- Lee IH, Yoo SY, Kim JH, et al. Atypical teratoid/rhabdoid tumors of the central nervous system: imaging and clinical findings in 16 children. Clin Radiol. 2009;64(3):256-264. doi:10.1016/j.crad.2008.09.007
- Ho B, Johann PD, Johann PD, et al. Molecular subgrouping of atypical teratoid/rhabdoid tumors - A reinvestigation and current consensus. Neuro Oncol. 2020;22(5):613-624. doi:10.1093/neuonc/noz235
- Li Z, Chen YA, Chow D, Talbott J, Glastonbury C, Shah V. Practical applications of CISS MRI in spine imaging. Eur J Radiol Open. 2019;6(May):231-242. doi:10.1016/j.ejro.2019.06.001