Congenital malignant melanoma of the dura
By Sylvestre D, Brown C, Schilling A

CASE SUMMARY
A male neonate presented at birth with a subcutaneous mass in the parieto-occipital region. He had an unremarkable birth history. Brain MR imaging at 4 days’ old revealed a large mass. The mass was resected. The mass was identified as dural-based malignant melanoma in the parieto-occipital region. The lesion extended between the sutures into subcutaneous tissue. The tissue was red-brown with scattered cytoplasmic pigment and extracellular pigment accumulation. Neoplastic cells were positive for S100, HMB-45, and vimentin. The BRAF mutation was not detected. The patient developed numerous hyperpigmented 2- to 3-mm nodular lesions, which were histopathologically identified as malignant melanoma. After resection, the patient began chemotherapy at 3 mo old. Postoperative brain MRI and CT demonstrated no evidence of intracranial mass, hemorrhage, or hydrocephalus. PET/CT revealed no evidence of metastases. The postoperative midline occipital defect was repaired with cranioplasty. He has met all developmental milestones with no residual neurological deficits.
IMAGING FINDINGS
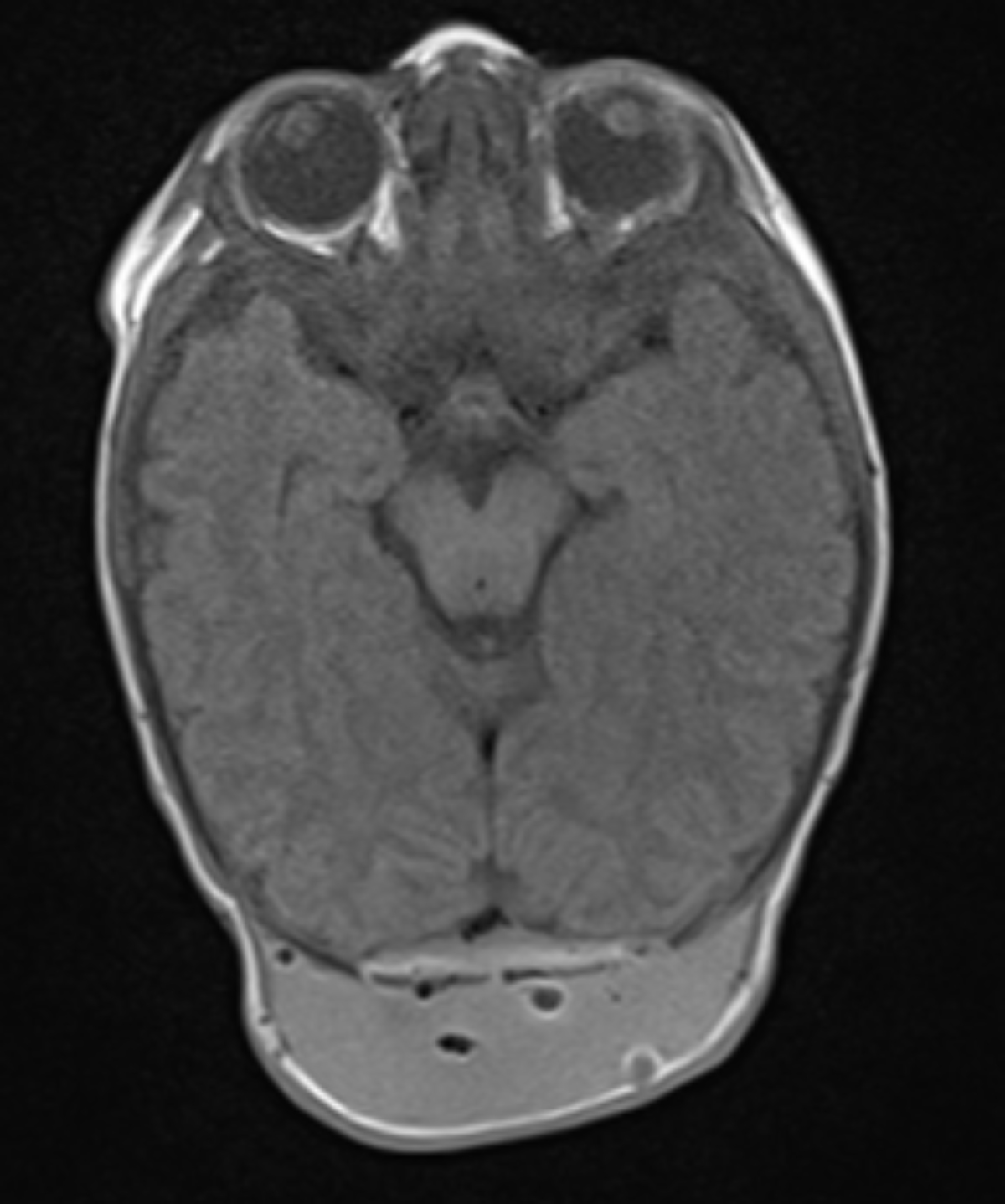
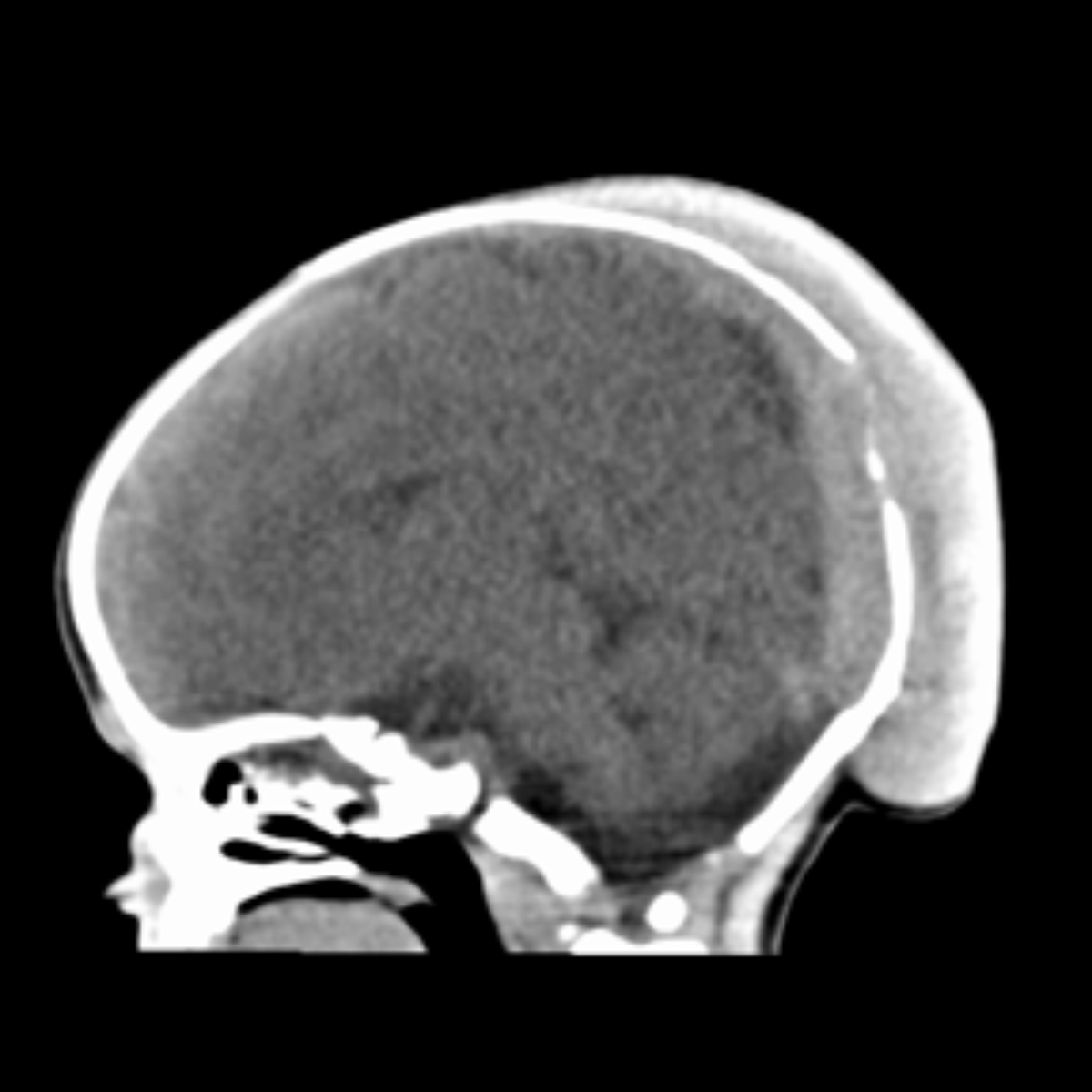
Brain MRI demonstrates a mass with intracranial T1 hyperintensity/T2 hypointensity and extracranial heterogenous T1 hyperintensity/T2 hypointensity with mass effect on the patent superior sagittal sinus and brain parenchyma (Figures 1,2). Computed tomography demonstrates posterior cortical irregularity with posterior scalp edema (Figure 3).
DIAGNOSIS
Congenital malignant melanoma of the dura
DISCUSSION
This case demonstrates congenital malignant melanoma of the dura mater with extracranial extension through the occipital bone. Magnetic resonance imaging (MRI) revealed mostly T1 hyperintensity and T2 hypointensity. Computed tomography revealed extracranial extension of the mass through the occipital bone.
Congenital brain tumors (CBTs) are uncommon diagnoses which account for less than 2% of pediatric brain tumors.1,2 There are many different types of CBTs, such as teratoma, astrocytoma, glioblastoma multiforme, PNET, and choroid plexus tumor.1,2 Teratoma is the most frequently diagnosed CBT.1,2 The CBT site is more commonly supratentorial than infratentorial.1,2 There are limited guidelines available for diagnosing and managing a CBT.2 The prognosis is guarded due to the large size of the tumor.1 Imaging plays a vital role in the detection and surgical treatment of CBT.1
Congenital malignant melanoma is very rare. The origin of this condition can be classified as de novo, transplacental, or from giant congenital malignant nevus.3 In a review of 20 reported cases, Scalvenzi et al found that the diagnosis has a variable outcome and is more common in males.3 It is likely that the tumor arose de novo, as there was no cutaneous GCMN present or maternal diagnosis of malignant melanoma. The immunohistochemistry of the intracranial mass and cutaneous lesions was consistent with malignant melanoma. Neoplastic cells were positive for S100, HMB-45, and vimentin. S-100 is the most sensitive for detection of melanocytic lesions, whereas HMB-45, MART-1/Melan-A, tyrosinase, and MITF are more specific and less sensitive.4
Meningeal melanoma is more likely to develop from leptomeninges (pia, arachnoid) than the pachymeninges (dura).5 According to Hayward, a central nervous system (CNS) malignant melanoma should be diagnosed as primary if there is “no malignant tumour outside the CNS, involvement of the leptomeninges, intramedullary spinal lesions, hydrocephalus, tumour in the pituitary or pineal gland, or a single intracerebral lesion.”6 This patient’s cutaneous lesions developed after the dural mass was resected. No other CNS masses were identified. These findings are consistent with a dural-based primary lesion.
Computed tomography and brain MRI were beneficial in narrowing the differential diagnosis. The CT scan demonstrated the intracranial mass with extracranial extension and posterior scalp swelling. Preoperative T1-weighted MRI demonstrated intracranial and extracranial hyperintensity, and T2-weighted MRI demonstrated mostly intracranial and extracranial hypointensity. Sinus pericranii, lymphangioma, and meningoencephalocele were considered unlikely. The MRI did not exclude hemangioma or hematoma. Brain MRI was consistent with the typical melanotic pattern of malignant melanoma with hyperintensity on T1-weighted images and hypointensity on T2-weighted images.7,8 Tumors with >10% melanin-containing cells are more likely to demonstrate the melanotic pattern.7 However, this pattern on T1- and T2-weighted MRI is not uniformly found in all malignant melanoma cases.7
CONCLUSION
This case describes dural based intracranial and extracranial congenital malignant melanoma, which is is an exceptionally rare diagnosis. Brain MRI of the tumor demonstrated the typical melanotic pattern of predominantly T1 hyperintensity and T2 hypointensity. Computed tomography revealed cortical irregularity and posterior scalp swelling. Neuroimaging with CT and MR was essential in guiding management and monitoring for recurrence of this condition.
REFERENCES
- Buetow P, Smirniotopoulos J, Done S. Congenital brain tumors: A review of 45 cases. Am J Neuroradiol. 1990; 11:793-799.
- Sugimoto M, Kurishima C, Masutani S, et al. Congenital brain tumor within the first 2 months of life. Pediatr and Neonatol. 2015; 56:369-375.
- Scalvenzi M, Palmisano F, Cacciapuoti S, et al. Giant congenital melanocytic naevus with proliferative nodules mimicking congenital malignant melanoma: A case report and review of the literature of congenital melanoma. Case Rep Derm Med. 2013;2013: Article ID 473635, 6 pages.
- Ohsie S, Sarantopoulos G, Cochran A, et al. Immunohistochemical characteristics of melanoma. J Cutan Path. 2008; 35:433-444.
- Escott E. A variety of appearances of malignant melanoma in the head: a review. Radiographics. 2001; 21:625-639.
- Hayward R. Malignant melanoma and the central nervous system. J Neuro Neurosurg Psychiatry.1976; 39:526-530.
- Isiklar I, Leeds N, Fuller G, et al. Intracranial metastatic melanoma: correlation between MR imaging characteristics and melanin content. Am J Roentgenol. 1995; 165:1503-1512.
- Smith A, Horkanyne-Szakaly I, Schroeder J. From the radiologic pathology archives: Mass lesions of the dura: beyond meningioma—radiologic-pathologic correlation. Radiographics. 2014;34: 295-312.
Prepared by Ms. Sylvestre while a third-year Medical Student at Mercer University School of Medicine, Savannah, GA; and Dr. Brown while a PGY-4 Diagnostic Radiology Resident, and Dr. Schilling while Section Chief of Neuroradiology, at Memorial Health University Medical Center, Savannah, GA.
