Primary localized ureteral amyloidosis mimicking urothelial carcinoma
By Ali ST, Shah S, MD, Przybycin C
CASE SUMMARY
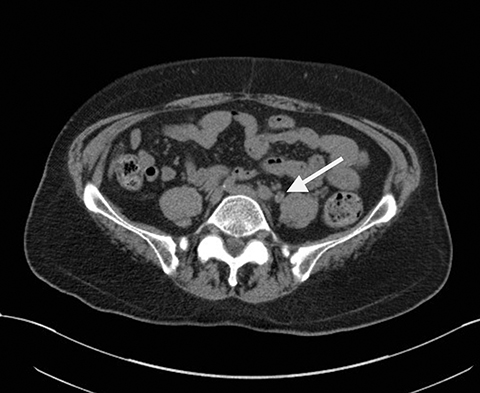
In 2005, a 74-year-old Indian male with a history of coronary artery disease, hyperlipidemia, and diabetes presented with left-sided flank pain without hematuria. The patient was a non-smoker and was on aspirin 81mg daily at home. Except for a mildly elevated blood glucose, his labs including comprehensive metabolic panel, complete blood count and coagulation studies (PT, PTT, and INR) were within normal limits. Urine cytology was negative for malignant cells. A noncontrast CT scan was ordered to evaluate for renal calculi but had revealed a left-sided, short segmental, mid-ureteral thickening with a punctate calcification and mild hydroureteronephrosis (Figure 1).
IMAGING FINDINGS
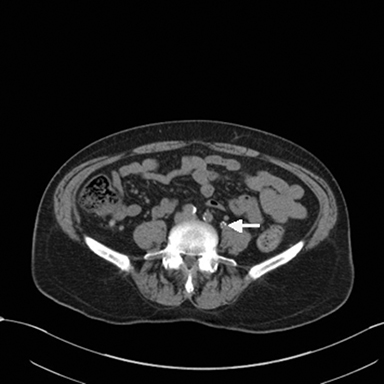
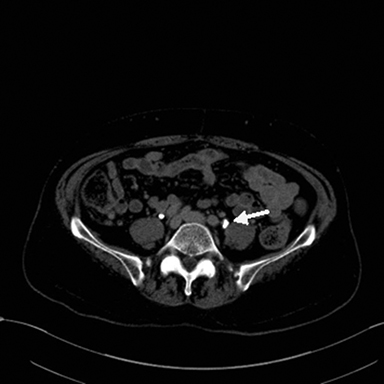
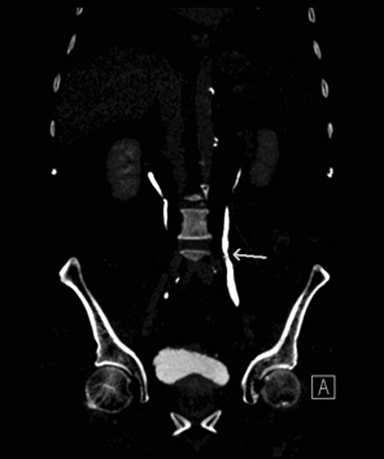
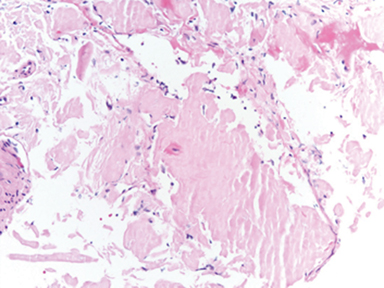
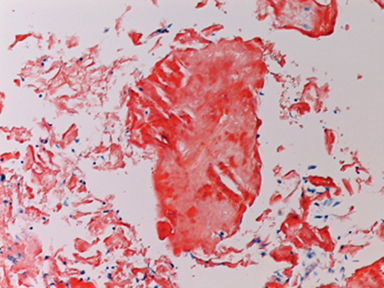
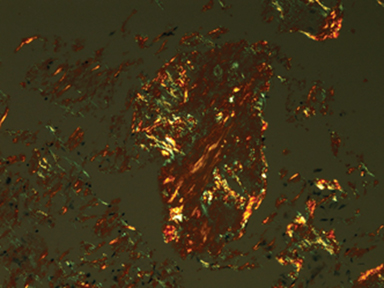
On a visit in 2013, the patient was evaluated with CT urogram without and with IV contrast (150cc IV iohexol 300, Figure 2). CT urogram without contrast demonstrated wall thickening with circumferential calcification of the middle left ureter with mild luminal narrowing without hydronephrosis. Corticomedullary phase did not depict an enhancing renal or ureteral mass. Excretory phase depicted a mild irregular wall thickening with no intraluminal filling defect. Cystoureteroscopic biopsy was subsequently performed and revealed abundant amorphous eosinophilic material consistent with amyloid. The presence of amyloid was confirmed by Congo red staining, showing apple-green birefringence under polarized light, as well as by a Thioflavin S stain under fluorescence microscopy, which was positive (Figure 3).
DIAGNOSIS
Primary localized ureteral amyloidosis mimicking urothelial carcinoma
DISCUSSION
Primary localized amyloidosis of the ureter is a rare disorder that is clinically and radiographically difficult to distinguish from urothelial carcinoma. Amyloidosis comprises a variety of protein-folding disorders that result in an extracellular deposition of protein aggregates, or amyloid, in tissues and organs, and may be systemic or localized, with the systemic form being classified as primary or secondary disease.1 Primary amyloidosis is associated with immune dyscrasias, such as multiple myeloma and Waldenström’s macroglobulinemia,2,3 while secondary amyloidosis is associated with chronic inflammatory conditions, such as rheumatoid arthritis, Crohn’s disease and tuberculosis.4 Localized amyloidosis is much less common than systemic amyloidosis and occurs in about 10-20% of amyloidosis cases.3,5 This condition can occur in the lungs, trachea, larynx, tongue, skin, nervous system, gastrointestinal system and genitourinary system.3,6
Localized amyloidosis of the urinary tract is of clinical importance because it mimics urothelial carcinoma. Depending on the degree of disease involvement, patients may present with painless hematuria, irritative urinary symptoms, and obstructive symptoms.3,7 Although the cause of localized amyloidosis of the urinary tract is unknown, local monoclonal plasma cell infiltrates and local amyloid synthesis have been suggested as causes.3,7 Within the genitourinary tract, localized amyloidosis is commonly found in the prostate and seminal vesicles, but can also occur in the bladder, renal pelvis, ureter and urethra.5,9 Ultrasound, CT scans and MRI are often used as initial methods to evaluate patients with urinary tract amyloidosis.
Primary localized amyloidosis of the ureter has been reported to occur more often in females, with the average age of presentation across both genders to be 58.4 It is a rare disorder and occurs less frequently than amyloidosis of the prostate, seminal vesicles and bladder.5,9 In a previous study, amyloidosis is typically unilateral and most commonly affects the distal third of the ureter.9 Patients can present with features of ureteral stricture and hydronephrosis.10 Ultrasound and intravenous pyelography can reveal hydronephrosis.4 Computed tomography may identify nonspecific diffuse thickening of ureteral walls and calcifications, which may also be seen with urothelial carcinoma, tuberculosis, schistosomiasis or hematoma.4,7,8,10,11 Localized amyloidosis has previously been described to present on MRI T2 weighted imaging as a hypointense lesion without obvious mass-effect, a characteristic that may distinguish amyloidosis from carcinoma.4,8,9,10
Urine cytology is insufficient for distinguishing amyloidosis from carcinoma because of the subendothelial location of many amyloid deposits and because of the limited (50%) sensitivity for urothelial carcinoma.6 Definitive diagnosis of amyloidosis is achieved with biopsy. Congo red staining of amyloid under light microscopy with polarized light classically produces the appearance of apple-green birefringence. Treatment of the amyloid sample with potassium permanganate may help distinguish the type of amyloid protein.4 Immunohistochemistry or mass spectrometry may provide further information about protein components of the particular amyloid.4
Localized amyloidosis of the ureter usually is benign and typically carries a good prognosis.4,6,12 Systemic amyloidosis must be ruled out prior to treatment, as certain diseases, including multiple myeloma, Hodgkin lymphoma, and renal cell carcinoma can manifest with systemic amyloidosis.13 Systemic amyloidosis can be excluded by utilizing serum and urine electrophoresis, chest radiography and if appropriate, rectal biopsy or fine needle aspiration of subcutaneous fat.2 Once localized amyloidosis of the urinary tract is confirmed, various treatment options may be considered. Patients with non-obstructing amyloidosis can be observed and followed with serial imaging to assess disease status.12 Cases of ureteral amyloidosis in which malignancy could not be excluded preoperatively or intraoperatively, or cases in which ureteral involvement precluded renal preservation have been treated with nephroureterectomy.4 Alternative surgical treatments may be utilized in patients in whom biopsy can confirm amyloidosis prior to surgery, and include ureteroneocystostomy, resection with end anastomosis of the ureter, and autotransplantation.4,8 Medical management of ureteral amyloidosis with oral colchicine and oral or topical dimethyl sulphoxide have been reported.4,8,9
CONCLUSION
Localized amyloidosis of the urinary tract is rare and is difficult to differentiate from malignancy based on clinical and radiographic features alone. MRI findings of T2 weighted hypointense lesions may help distinguish amyloidosis from malignancy. Additional studies would help characterize the sensitivity and specificity for this study. Radiographic features of the other imaging modalities may be nonspecific, but it is important for clinicians and radiologists to be cognizant of this disease so proper management and treatment may be provided.
REFERENCES
- Chitale S, Morsey M,Peat D,Webb R.Amyloidosis of lower genitourinary tract: a review. EAU-EBU Update Series. 2007;5:70-76.
- Merrimen JL, Alkhudair WK, Gupta R. Localized amyloidosis of the urinary tract: case series of nine patients. Urology. 2006;67(5):904–909
- DeSouza MA, Rekhi B, Thyavihally YB, et al. Localized amyloidosis of the urinary bladder, clinically masquerading as bladder cancer. Indian J Pathol Microbiol. 2008;51:415-417.
- Ding X, Yan X, Ma X, et al. Localized amyloidosis of the ureter: A case report and literature review. Can Urol Assoc J. 2013;7(11-12):E764-E767. doi:10.5489/cuaj.576.
- Kawashima A, Alleman WG, Takahashi N, et al. Imaging evaluation of amyloidosis of the urinary tract and retroperitoneum. Radiographics. 2011;31:1569-1582.
- Zhou F, Lee P, Zhou M, Melamed J, Deng F-M. Primary localized amyloidosis of the urinary tract frequently mimics neoplasia: a clinicopathologic analysis of 11 cases. Am J Clin Exp Urol. 2014;2(1):71-75.
- Domiciano DS, De Carvalho JF. Primary localized amyloidosis of the ureter. Isr Med Assoc J. 2008;10:237-238.
- Tsujioka Y, Jinzaki M, Tanimoto A, et al.. Radiological findings of primary localized amyloidosis of the ureter. J Magn Reson Imaging. 2012;35:431-435.
- Singh SK, Wadhwa P, Nada R, Mohan VC, Singh P, et al. Localized primary amyloidosis of the prostate, bladder and ureters. Int Urol Nephrol. 2005;37:495–497
- Weiwei Z, Yi H, Jinsong Z. Primary localized amyloidosis of the ureter. Abdom Imaging. 2011;36:609-611.
- Paidy S, Unold D, Catanzano TM. AIRP best cases in radiologic-pathologic correlation: localized amyloidosis of the renal pelvis. Radiographics. 2012;32:2025-2030.
- Borza T, Shah RB, Faerber GJ, Wolf JS. Localized amyloidosis of the upper urinary tract: a case series of three patients managed with reconstructive surgery or surveillance. J Endourol. 2010;24(4): 641–644.
- Raja K, Ahmed E, Mubarak M, et al. Primary Localized Amyloidosis of Urinary Bladder: A Case Report and Review of Literature. Nephrourol Mon. 2013;5(5):994-996.
Prepared by Dr. Ali and Dr. Shah while practicing in the Department of Radiology, and Dr. Pryzybycin while practicing in the Department of Pathology, at the Cleveland Clinic, Cleveland, OH. The authors have no conflicts of interest to disclose.
