Approach to local anesthesia in children
Pain management is a very important component of pediatric intervention, especially in procedures performed only under local anesthesia or local anesthesia and sedation. It has been stated that the administration of a local anesthetic can be the most painful part of a procedure. A minor pain at the beginning of a procedure can upset the child, making completion of the procedure more difficult. The best way to minimize the intensity of a painful stimulus is to provide suitable skin and track anesthesia to the level of the target anatomy. There are several ways to approach this objective. They include: using warmed, buffered 1% lidocaine, EMLA cream, or needleless injection of 1% lidocaine with J-tip technology. This review discusses the advantages and disadvantages of the different approaches to decreasing or even eliminating the pain of medical procedures performed in the pediatric population.
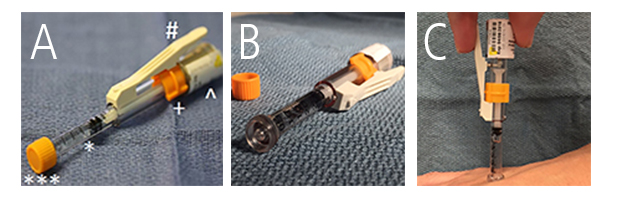
Figure 1. The J-tip. (A) The J-tip device filled with a 1% lidocaine solution. The features of the device include the CO2 charge to propel the solution into the skin surface [^], a reservoir for the local anesthetic [*], and an orange trigger guard [+] that is pushed downward to allow the trigger [#] to be pressed releasing the CO2. At the tip of the device is a cover [***] that is removed prior to injection. (B) A close up of the needle-free end of the J-tip. (C) The tip is pressed against the skin perpendicular to the surface. The trigger is than pushed activating the CO2 charge and injecting the anesthetic solution into the skin.
Multiple variables influence the amount of pain associated with injection of local anesthesia. Needle diameter, analgesic agent, pH and temperature of the anesthetic agent, and injection rate are just a few. Needle size was tested in a double-blinded study using 27g, 28g, 30g, 31g, and 32g needles injected into the thighs of 30 adults. The authors felt that by decreasing the outer diameter of a needle, the frequency and severity of insertion pain can be reduced.
Lidocaine has a natural pH balance of 6.4. When buffered in a 9:1 ratio with sodium bicarbonate, the pH is increased to 7.4. Along with pH, it is thought that the temperature of the injection can also aid in pain reduction. Warming the liquid agent is an inexpensive and easy way to reduce injection pain. Interestingly, warming the anesthetic does not affect drug activity. The injection rate can also be varied to reduce pain. It is believed that injection with slow, incremental needle advancement allows for the anesthetic to be injected into an area previously injected, minimizing pain.
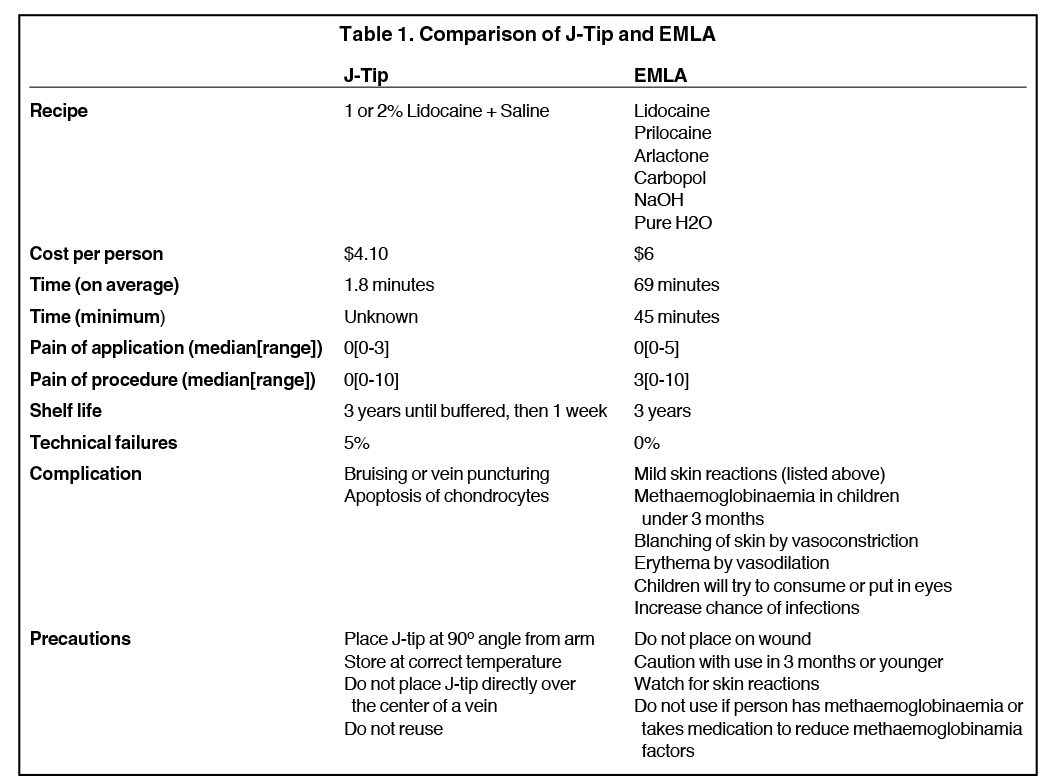
One (1) gram of Eutectic Mixture of Local Anesthetics (EMLA) cream is made up of 25 mg Lidocaine, 25mg Prilocaine, 19mg Arlactone 289, 10mg Carbopol 934, sodium hydroxide, and purified water. Both Lidocaine and Prilocaine are local anesthetics, while Arlactone is a stabilizer and carbopol a thickening agent. Sodium hydroxide is added until the compound reaches a pH of 9.6. EMLA cream can be used by itself prior to procedures or as a skin numbing agent before injecting a local anesthetic. EMLA cream is applied to the skin and a dressing is applied over it. The cream must be applied to the skin at least 45 minutes prior to the procedure. It often causes skin blanching and vasoconstriction of surface blood vessels that can make placing a peripheral intravenous line more challenging.
The anesthetic in the J-tip (Figure 1) is made from a mixture of 1% or 2% lidocaine and saline. The liquid components are administered via a plastic injector. The injector is needle-free and works by forcing the liquid into the dermis via a small carbon dioxide charge set off by a trigger-like feature while the device is in contact with and perpendicular to the skin. The local anesthetic can penetrate to a depth of 5-8mm and has been recorded to stimulate no pain. The J-tip provides adequate sedation within minutes, and similar to the EMLA cream, it can be used alone or as a pre-anesthetic for injection. For a comparison of a J-tip and EMLA cream see Table 1.
OPINION
Employing needles with the smallest diameter possible minimizes patient discomfort when injecting a local anesthetic. The use of a 30G needle would further reduce pain. Also, larger needles increase the likelihood of bleeding, which is associated with greater probability of a painful reaction.
Marcaine and Lidocaine are both commonly used local anesthetics for children. Marcaine, with added epinephrine, has been shown to have a longer time of action, lasting almost 5 hours compared to 2 hours with lidocaine. However, both anesthetics have significantly reduced pain.
The pH balance can also impact the pain response. Studies evaluating buffered Lidocaine have had mixed results. Some have shown no statistical difference in pain response, while others have shown a decrease in pain. We use buffered lidocaine on children who are sedated or awake and feel that it does help reduce pain.
Another common way to reduce injection pain is to warm the injected agent prior to administration. Compared to lidocaine at room temperature, warming lidocaine has been shown to reduce pain. The literature is unclear as to whether warmed and buffered lidocaine is beneficial. No studies show warming, buffering, or both to be more painful than plain lidocaine. We currently use a warmed and buffered solution of 1% lidocaine with excellent results.
One of the easiest and most effective ways to eliminate pain is through injection rate. We believe that a slow injection rate is crucial to reducing the pressure and burning sensation at the injection site, which in turn makes it less painful. Injecting slowly reduces injection pain more than buffering the solution. In addition, it is best to start injecting the local anesthetic from just below the dermis toward the target site and not deep to superficial. It is helpful to try to keep the injected liquid within the advancing edge of the injected liquid [numb zone]. This approach effectively minimizes patient discomfort and keeps the child calm.
EMLA cream is used as a topical anesthetic; it reaches its maximum effect within 120 to 180 minutes, at a 5mm depth into the skin. When applied for only 20 minutes, and compared to a placebo cream, there is no statistical difference in pain. Studies show that EMLA cream should be applied to the hand for at least 45 minutes. The EMLA cream will last up to 4 hours at a depth between 1.0 and 1.9 mm.
EMLA cream will blanch the skin after 30 minutes as a result of vasoconstriction and brings the risk of methemoglobinemia (especially in infants) due to the presence of Prilocaine. We no longer use EMLA cream due to its slow onset of action and its skin-blanching effect. In our practice, the EMLA cream has been replaced by the J-tip. The J-tip delivers near instantaneous skin anesthesia without a needle and is well accepted by children of all ages. It has been shown to be virtually painless, although the “popping sound” associated with the propulsion of gas can surprise the child if he or she is not warned ahead of time. It is important to note that a J-tip can injure a veinif applied directly over superficial venous anatomy. When compared to EMLA cream, the average time from application to procedure was 1.8 minutes for the J-tip and 69 minutes for the EMLA cream. Also, in comparison studies the J-tip facilitated less track pain.
CONCLUSION
We recommend using the J-tip before all local anesthesia injections. The J-tip immediately anesthetizes the skin and is less stressful for the child because of its needle-less technology. However, it is important to remember that this only provides superficial skin anesthesia, and when a longer track is required, it should be followed by a slow injection of warm, buffered 1% lidocaine through a 27g or 30g needle. The track of anesthesia should be created in a superficial to deep direction to minimize the “burning” sensation, an inherent property of the analgesic. By greatly reducing pain to the patient, taking all the precautions discussed here will maximize patient cooperation, confidence and satisfaction.
Citation
Approach to local anesthesia in children. Appl Radiol.
June 10, 2016