Ankle Impingement Syndromes: What the Radiologist Needs to Know
Ankle impingement syndromes (AISs) compress the osseous and soft-tissue structures about the tibiotalar joint as a sequela of acute traumatic injury or repetitive microtrauma. They typically affect athletes who present with ankle pain and swelling that are relieved with rest. A chronic course may ensue with signs of ankle instability and/or limited range of motion (ROM), along with pain while squatting, sprinting, and climbing stairs. AISs are classified according to their location relative to the joint: anterior, anterolateral, anteromedial, posteromedial, or posterior.
While diagnosis is typically made with clinical examination, imaging plays an important role in localizing pathology and guiding treatment options, including surgery. Here, we review the anatomy, pathophysiology, physical exam, imaging characteristics, and management of AISs.
Anatomy Overview
A basic understanding of ankle anatomy is integral to understanding the structures that may be involved in the various impingement syndromes.
The tibiotalar joint comprises the articulation of the tibia, fibula, and talus ( Figure 1 ). The tibia and fibula collectively form a mortise that houses the trochlea of the talus, while the tibia forms the medial malleolus and the fibula forms the lateral malleolus. The malleoli constrain the talus into essentially a hinge joint with inherent stability in neutral alignment. Together with the wider anterior geometry of the talar trochlea, this imparts stability to the joint such that the bony constraints resist eversion in standing alignment. However, as the joint moves through the arc of motion along its oblique axis, the soft tissues become critical in maintaining ankle stability.
From left to right: frontal, posteromedial, and lateral depictions of relevant ankle joint anatomy created on complete anatomy.
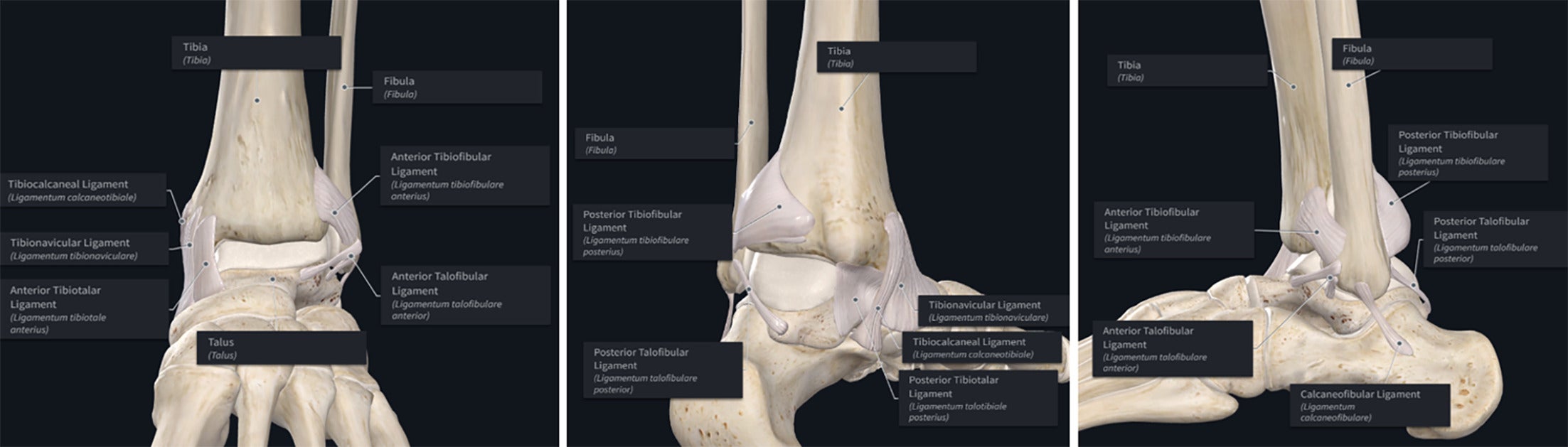
The syndesmotic complex restrains motion between the distal tibia and fibula to maintain the bony mortise geometry through dynamic motion. The complex comprises the anterior tibiofibular ligament (AITFL), posterior tibiofibular ligament, and the interosseous ligament. This complex is also referred to as the “high-ankle ligaments.”
Inferior to these structures are the “low-ankle ligaments,” including the deltoid ligament complex and the lateral ligament complex. The medial aspect of the ankle is supported by the former, which spans the medial malleolus to the calcaneus, navicular, and talus, and consists of a superficial and a deep layer. The superficial layer consists of the tibiocalcaneal, tibionavicular, and superficial posterior tibiotalar ligaments (PTTLs). The anterior tibiotalar (ATTL) and PTTL make up the deep layer ( Figure 1 ). The deltoid ligamentous complex has a wide range of anatomical variations.1
The lateral ligament complex consists of 3 ligaments: anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL). The ATFL and PTFL attach the talus to the fibula anteriorly and posteriorly, respectively, while the CFL attaches the calcaneus to the fibula ( Figure 1 ).
Anterior Impingement
Pathophysiology
The primary mechanism of anterior impingement syndrome is direct and/or repetitive microtrauma between the anterior tibial joint line and talar neck, resulting in the formation of osseous spurs.2, 3 These spurs can entrap soft tissue, causing acute swelling or long-term development of hypertrophic synovial plicae or adhesions and degenerative sequelae that further limit motion.4, 5
Physical Exam
Palpating the anterior joint line in slight plantarflexion may reveal tenderness over the ankle anterior to bony osteophytes. The anterior impingement test involves hyper-dorsiflexion of the joint, eliciting tenderness across the front of the ankle.6 - 8 Generally, patients may sustain loss of dorsiflexion ROM compared with the contralateral side. The Silfverskiöld test is also performed to rule out isolated gastrocnemius contracture, which can also cause loss of dorsiflexion, displaying increased ankle joint dorsiflexion when the knee is flexed compared with when it is extended as a positive sign.9 - 11
Imaging Characteristics
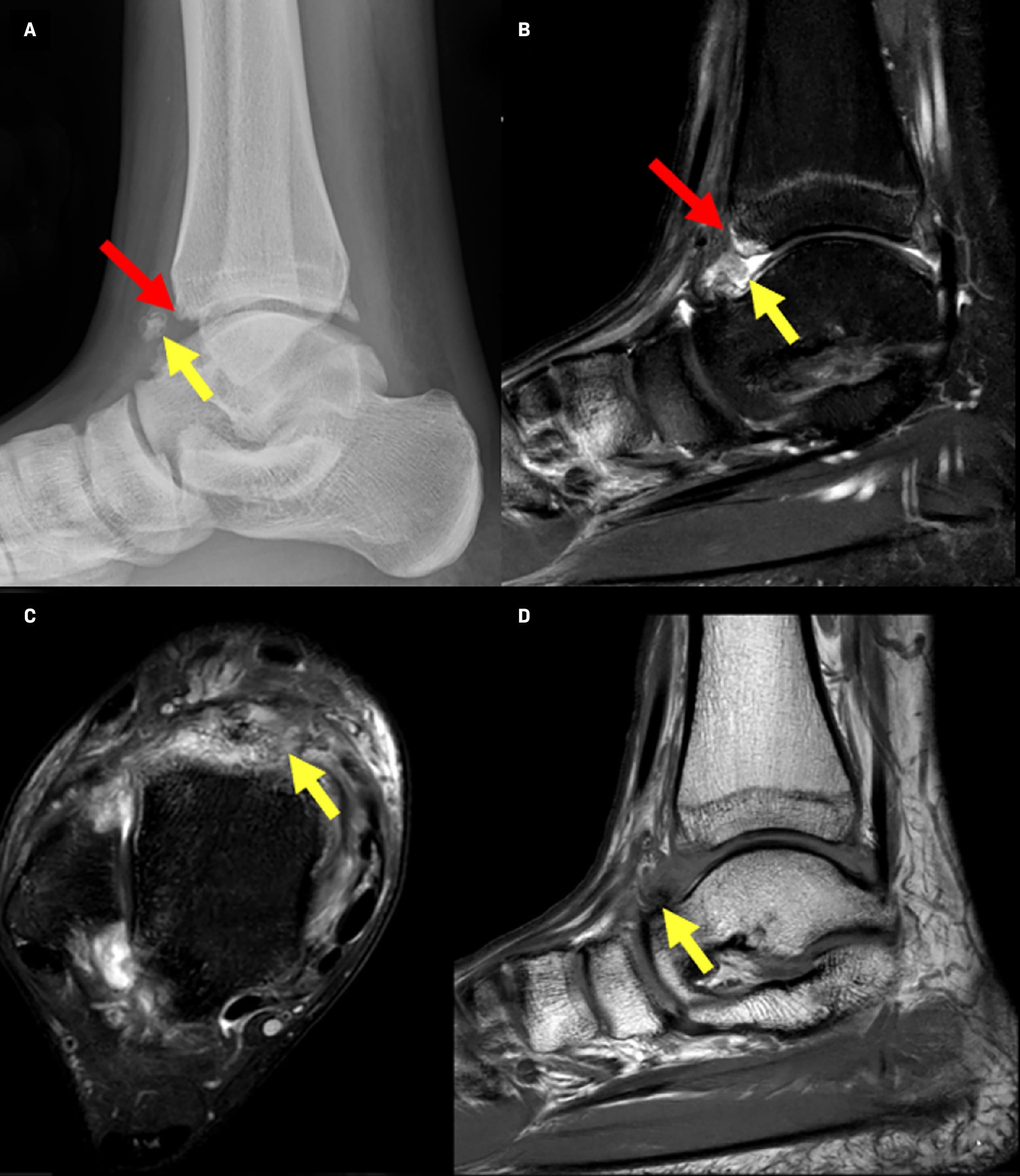
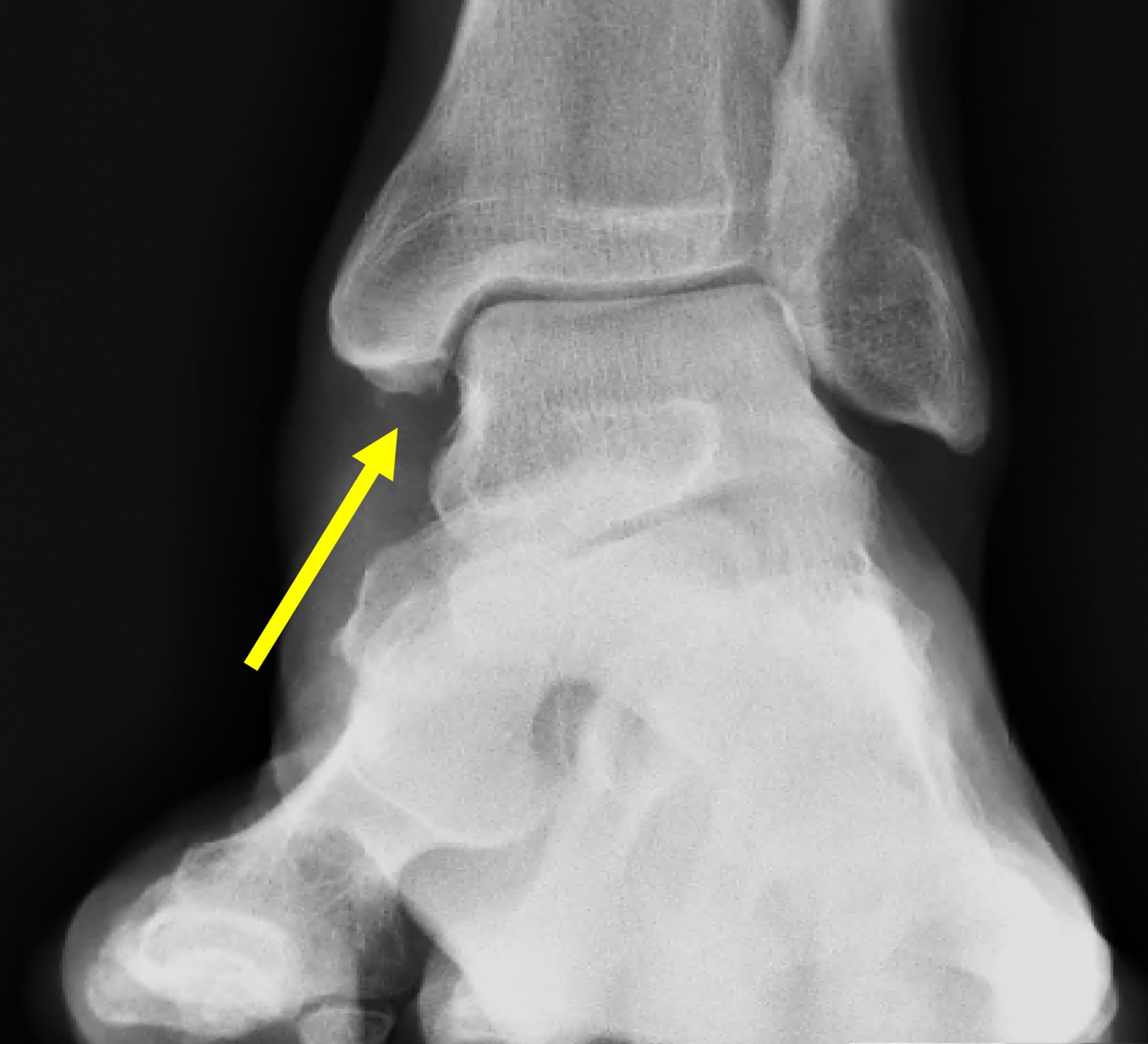
Conventional weight-bearing radiography demonstrates characteristic spurs, which appear as beaklike osseous outgrowths from the anterior margin of the tibial plafond. These can also be accompanied by spurs at the dorsal talar neck ( Figure 2 ). A weight-bearing lateral radiograph with the ankle in maximum dorsiflexion can demonstrate the opposing osseous spurs as seemingly overlapping at the anterior margins of the tibial plafond and talar neck.12 Although previously described as “kissing osteophytes,” morphological analyses with CT have suggested that talar and tibial spurs do not actually impinge upon each other as they are located medial and lateral to the talar dome, respectively.13 Radiography is usually sufficient to locate and quantify the size of the relative spurs. Talar spur length as determined on plain radiographs correlates positively with talar spur width as measured by CT.12
Conventional lateral ankle radiographs demonstrate characteristic spurs at the anterior tibial plafond and talar neck.

Two grading systems, Anterior Impingement Classification (AIC) and Osteoarthritic Classification (OAC), have been used to assess AIS based on radiography.14 - 16
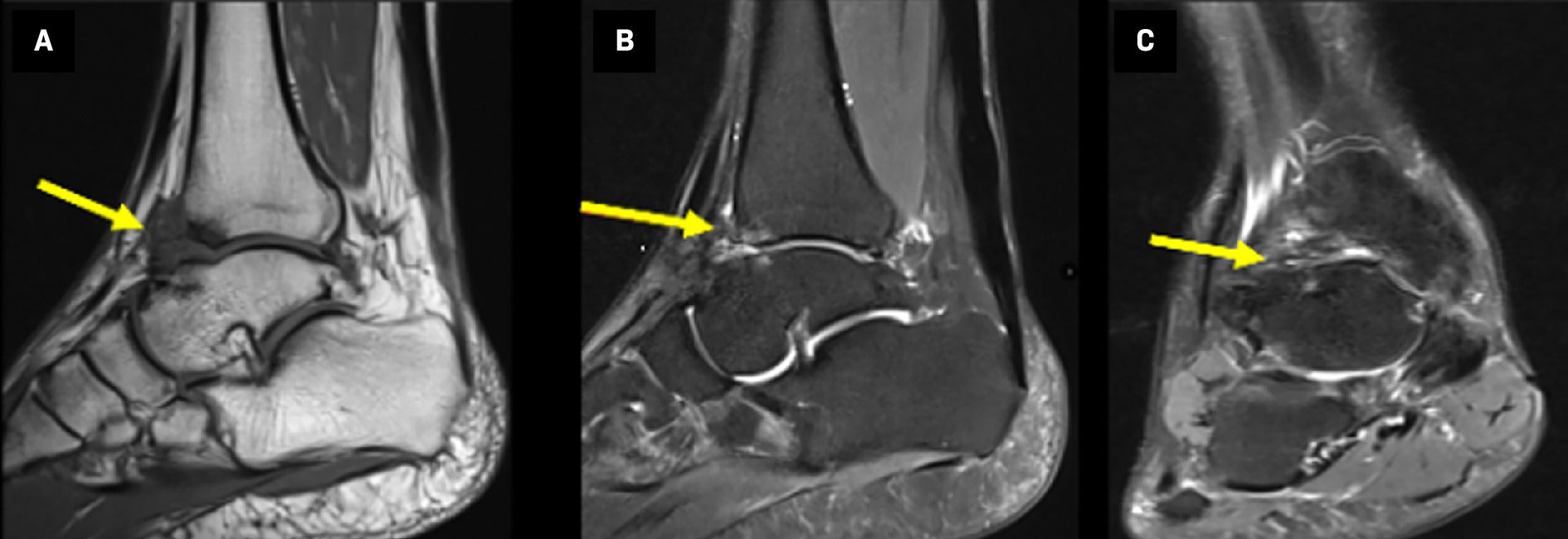
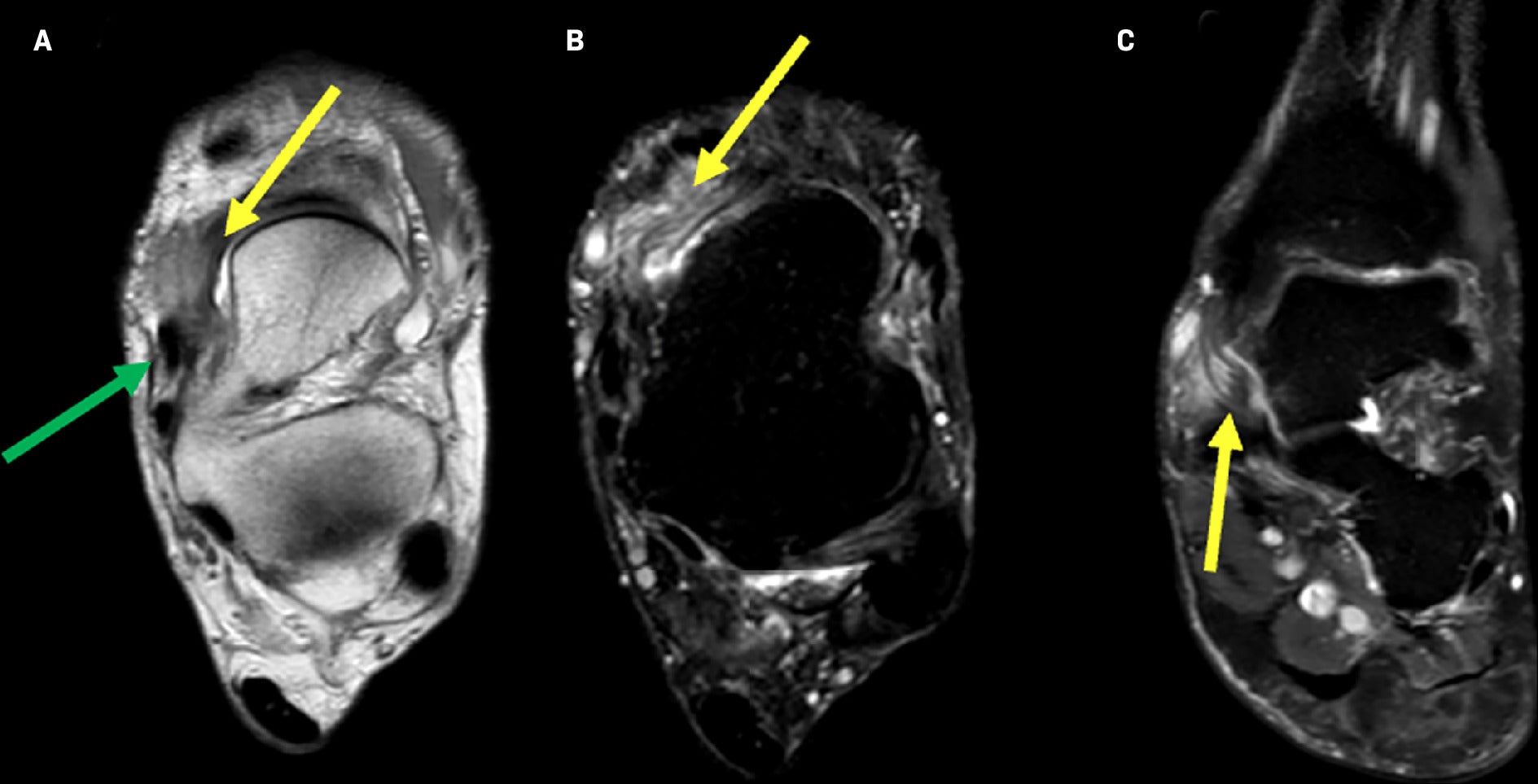
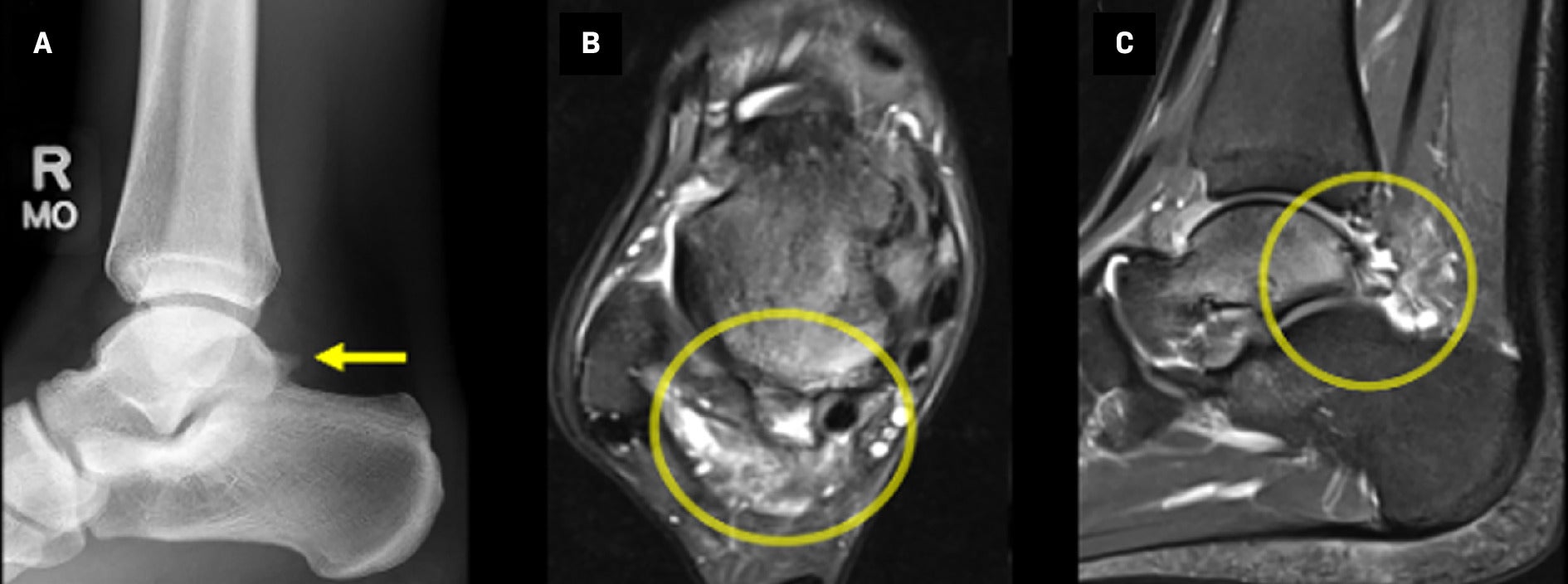
MRI may also help localize bone spurs.17 More importantly, however, MRI helps identify intra-articular fibrous bands, which may contribute to impingement, and detect any signs of synovial reactivity such as synovitis, capsular thickening, and formation of scar and granulation tissue ( Figures 3 , 4 ).18 - 20 Synovial inflammation is optimally seen on fat-suppressed T2 and contrast-enhanced fat-suppressed T1 images as an enhanced signal. MRI can also be useful in excluding other causes of pain that may clinically mimic anterior impingement such as an occult stress fracture of the anterior aspect of the distal tibia or an osteochondral lesion at the medial talar dome.12
( A ) T1 sagittal image demonstrates osteophytic spurring projecting from the anterior distal tibia and talar neck with surrounding region of soft-tissue fibrosis or focal synovitis. ( B ) T2 sagittal fat-saturated image demonstrates talar neck and anterior tibial marrow edema-like signal and intra-articular soft-tissue synovitis/fibrosis. ( C ) T2 coronal fat-saturated image demonstrates intra-articular soft-tissue synovitis/fibrosis.
( A ) Lateral radiograph of the ankle (top left) demonstrates a large intra-articular body and osteophytic spurring of the anterior talus and anterior distal tibia. ( B ) T2 fat-saturated sequence sagittal image (top right) demonstrates distal tibial edema-like signal and intra-articular soft-tissue synovitis/fibrosis. ( C ) T2 fat-saturated sequence axial image (bottom left) demonstrates anterior tibiotalar intra-articular soft-tissue synovitis/fibrosis. ( D ) T1 sagittal image (bottom right) demonstrates the radiographically large intra-articular body as a hypointense structure (yellow arrow).
Anterolateral Impingement
Pathophysiology
Anterolateral impingement (ALI) syndrome occurs when there is decreased space in the anterolateral recess—a space bounded by the ATFL and PTFL. A sprain of the ATFL is a common injury that can result in hemarthrosis and subsequent synovitis, contributing to a hyalinized fibroid mass within the recess known as a “meniscoid lesion.”21 Additionally, post-traumatic ligamentous hypertrophy and/or hyperlaxity leads to abnormal contact between the ATFL and osseous structures during movement, altering the normal biomechanics of talus extension into the recess during dorsiflexion.22, 23 Adjacent abnormalities to this recess, such as thickening of the AITFL, the presence of Basset ligament in ankle injury, or spurs at the anterolateral tibia or anterolateral talar neck, can lead to obliteration of the recess.24 - 26
Physical Exam
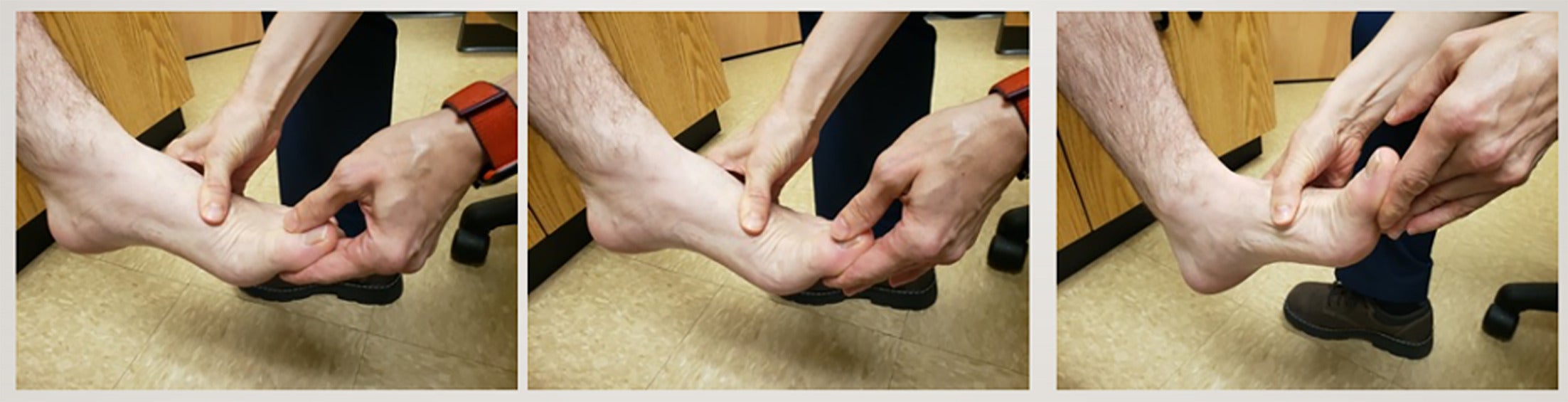
Patients typically demonstrate swelling and pain on palpation over the anterolateral joint line; however, most have normal ankle ROM.27 The anterior impingement test is performed with the patient sitting and the ipsilateral knee bent to 90° while the examiner passively hyperdorsiflexes the affected ankle. The test is considered positive if pain is elicited over the anterolateral ankle joint line ( Figure 5 ). The anterior drawer test and talar tilt test are also performed to assess integrity of the lateral ligaments and detect possible concomitant instability.
Anterior impingement test demonstrated with passive hyper dorsiflexion to elicit pain in the anterior ankle joint.

Imaging Characteristics
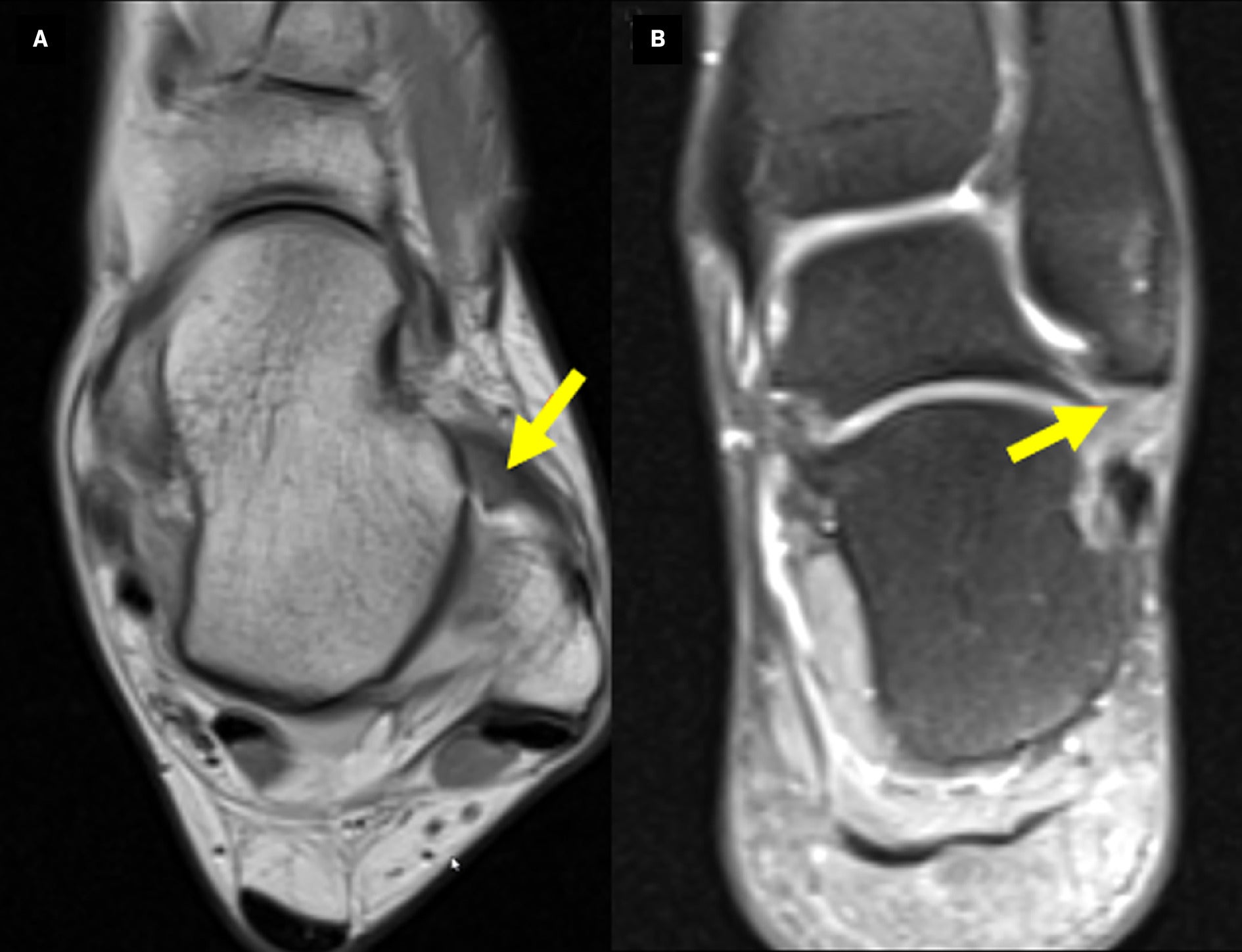
Conventional radiography may help identify osteophytes contributing to anterolateral recess obstruction ( Figure 6 ). However, given the etiology of this impingement is primarily related to soft tissue, MRI is often the modality of choice despite its variable sensitivity, which ranges from 42% to 83%.28 Ligamentous abnormalities such as thickening of ATFL and AITFL, synovial hypertrophy, and scarring in the anterolateral recess may be seen.28, 29 In advanced cases, the fibrotic scar tissue can hyalinize into a meniscoid lesion, which has an intermediate-to-low signal intensity with peripheral rim enhancement on T1 and T2 imaging ( Figure 7 ).12
( A ) Sagittal CT image demonstrates osseous spur in the anterior talar neck. ( B ) Sagittal CT image demonstrates osseous spur in the anterior tibial plafond.

( A ) Axial T1 image and ( B ) coronal proton density image of the ankle demonstrate scarring in the region of the anterior talofibular ligament with a low-to-intermediate signal meniscoid-shaped mass extending into the lateral ankle gutter.
MRI can be used with contrast-enhanced 3D fast spoiled gradient-echo protocols to visualize enhanced vascularized synovial and granulation tissue in the anterolateral recess with sensitivity upward of 91% and accuracy of 87%. These results are comparable to MR arthrography without being as invasive.30, 31 Bone marrow edema is rarely found.12 It is important to remember that physical exam findings play a particularly crucial role in diagnosing anterolateral ankle impingement. Liu et al demonstrated that physical examination, with a sensitivity and specificity of 94% and 75%, respectively, was more reliable than MRI, at 39% and 50%, for the diagnosis of suspected ALI compared against intra-operative confirmation.27
Anteromedial Impingement
Pathophysiology
Anteromedial impingement (AMI) has been the focus of little research, owing to its rarity relative to other such syndromes, the strength of the anteromedial joint, and the destabilizing forces required to cause impingement pathologies.32 Generally, AMI occurs with disruption of the anteromedial recess, which is bounded inferiorly by the ATTL. This can occur in the setting of ATTL thickening or hypertrophic synovial plica resulting from previous trauma or microtrauma, leading to the formation of spurs at the dorsal medial talar neck or anterior aspect of the tibia. Spurs alone are not sufficient for diagnosis.1, 33 Medial malleolar avulsion ossicles (nonunions), common in gymnasts and other athletes in high-stress sports, can also contribute to AMI.34, 35 Nonunion micromotion increases scarring and inflammation, essentially obliterating the medial ankle joint recess between the talus and medial malleolus.
Physical Exam
Palpation demonstrates pain and swelling over the medial anterior joint line. A forced anterior impingement test may also exacerbate pain, but the test has overall low sensitivity.34 Important to assess general joint laxity or restriction, ROM testing may also reveal the presence of subtle osteophytes. Ankle valgus stress testing is used to check the integrity of the deltoid ligament complex compared with the contralateral ankle; increased laxity or lack of a firm endpoint may indicate more severe injury and instability.
Imaging Characteristics
Spurs often appear along the most anterior portion of the medial talar facet, along with a corresponding “kissing” osteophyte just anterior to the corner of the medial mortise and the front of the medial malleolus.36 Anteroposterior and lateral radiographs are limited in diagnostic value because the anteromedial aspect of the tibiotalar joint is concealed by projection of the lateral aspect of the tibia. Instead, a lateral view with a craniocaudal inclination of 45°, with the foot in plantarflexion and the leg rotated 30o externally, is preferred.14 This nearly doubles the sensitivity for tibial and talar bone spurs ( Figure 8 ).11
Anteroposterior radiograph of the ankle demonstrates medial malleolar bone spur formation.
The role of MRI in detecting AMI has not been established. Images are aimed at visualizing ancillary soft-tissue pathology such as synovitis and deltoid ligament and capsular thickening ( Figures 9 , 10 ).37 The anteromedial recess itself may appear normal.38 Capsular thickening may be more subtle and can be better detected with intra-articular contrast-enhanced CT or MRI.37 MRI also plays a role in excluding other abnormalities, such as talar osteochondral injuries, in patients presenting with similar symptoms.
( A, B ) Axial proton density and proton density fat-saturated images demonstrate thickening and increased signal intensity of anteromedial ankle soft tissues, including the tibial spring ligament and the superficial portion of the deltoid ligament. Note that the tibialis posterior tendon (green arrow) demonstrates a normal appearance, arguing against a sequela of posterior tibial tendon dysfunction. ( C ) Coronal proton density fat-saturated image demonstrates thickening and edema of the anteromedial ankle soft tissues.
( A ) Anteroposterior radiograph of the foot shows osteophytic spurring of the medial talar neck and the distal tip of the medial malleolus. ( B ) Axial T2 fat-saturated image of the ankle demonstrates a reactive marrow edema-like signal of the medial talus and focal synovitis in the anteromedial gutter. ( C ) Coronal proton density fat-saturated image of the ankle demonstrates thickening of the deltoid ligament, focal synovitis in the anteromedial gutter, and reactive marrow edema-like signal of the talus.

Posteromedial Impingement
Pathophysiology
Posteromedial impingement (PMI) is often related to damage to the PTTL, which lies anterior to the posteromedial recess. Swelling from hypertrophy caused by healing of the PTTL can lead to entrapment of the posteromedial tibiotalar joint capsule.39 One arthroscopic study found concurrent distal medial malleolus and talar facet articular cartilage injuries in affected patients, indicating a possible association.40
Physical Exam
Clinical history and radiography are more useful in diagnosing PMI, owing to the challenges in examining the deeper posterior ankle tendons and ligaments.41, 42 Posteromedial pressure during ankle inversion and plantarflexion enhances identifying pain in the posteromedial corner; gait analysis is also useful as it can help differentiate true posterior tibial tendon dysfunction from PMI, which is associated with entrapment of the PTTL portion of the deltoid ligament.43
Imaging Characteristics
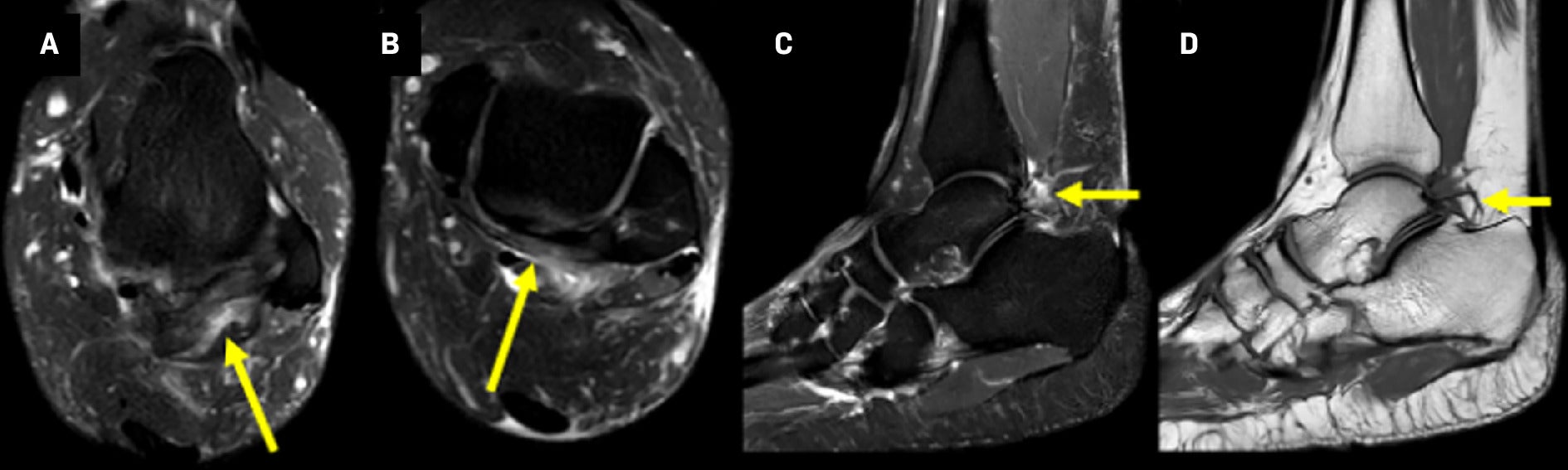
As pathophysiology is largely related to soft-tissue pathology, radiography plays a little role in imaging for PMI syndromes. Radiographs may show periosteal new bone formation along the posteromedial wall of the talus and along the medial malleolus.43 On MRI, signs can vary based on chronicity; in the subacute stage (within 4 weeks post-injury), the primary finding can be increased signal in the posteromedial capsule and the PTFL, whereas chronic stages (greater than 14 weeks post-injury) demonstrate a higher incidence of PTTL disruption with thickening and loss of normal fibrillar pattern, resulting in an amorphous appearance ( Figure 11 ).42 Fluid-sensitive sequences increase the conspicuity of synovitis, which may be seen as a focal increased signal relative to adjacent tissue.44 Marrow edema can be seen infrequently and has no specific distribution.45 In general, bone changes are less common in PMI; however, small cortical avulsion fractures may be present in the PTTL and are best demonstrated on CT.44
( A ) Coronal T2 fat-saturated image of the ankle demonstrates reactive edema-like signal and fluid within the posteriomedial ankle, likely owing to impingement by prominent talocalcaneal osteophytes. ( B ) Axial T2 fat-saturated image of the ankle demonstrates thickening and loss of the normal deltoid ligament striations and marked posteromedial soft-tissue swelling.

Posterior Impingement
Pathophysiology
The posterior ankle is bordered by the posterior tibia and calcaneus and extends to the Kager fat pad. Compression within this region during plantar flexion is characteristic of posterior impingement (PI) syndrome.
In particular, os trigonum is a common finding, seen in up to 63% of patients with PI.46 Normally, the secondary ossification center of the posterolateral talus forms between the ages of 8 and 13 years and fuses within 1 year; however, 7 % of the time a lack of fusion can result in an os trigonum.47 Other osseous pathologies, such as chronic fracture nonunion of the medial tubercle of the posterior talus, can present with a similar clinical picture or a congenital Stieda process, which is a fusion of a secondary ossification center, resulting in posterolateral elongation of the talus.46
Physical Exam
Examination involves passive hyperplantarflexion of the ankle while using 2 fingers to palpate just lateral to the Achilles tendon at the level of the distal fibula; PI is suspected if the patient’s pain is reproduced. Contributing pathology can be delineated with maneuvers such as the Tomassen test, in which a positive result reveals decreased ROM of the great toe metatarsophalangeal joint with the ankle dorsiflexed. This can suggest FHL pathology ( Figure 12 ). Additional maneuvers, such as a calcaneal squeeze test, which involves squeezing both sides of the posterior tuberosity, can raise concern for differential diagnoses such as a calcaneal stress fracture involving the posterior tuberosity.
Normal examination of great toe metatarsophalangeal joint pathology range of motion, which is greater in ankle plantarflexion than ankle dorsiflexion. Alternative findings can be suggestive of flexor hallucis longus pathology.
Imaging Characteristics
Weight-bearing radiography in the anteroposterior, lateral, and mortise views, along with an oblique view of the foot, is important for treatment planning. The oblique view, with the foot in 25° of external rotation, can help differentiate hypertrophy of the posterior talar process from os trigonum in cases of bony impingement.48 Advanced imaging may also be necessary in equivocal cases.
Os trigonum in the lateral view is the most pertinent radiographic finding when assessing for PI; however, its presence alone is not sufficient to cause impingement, but it can contribute to symptomatology.18 Up to 14% of the asymptomatic population may have an os trigonum.49
CT facilitates the assessment of osseous changes between the os trigonum and talus, such as fragmentation of the os and pressure-related erosions along the talus.49 On MRI, PI can present with bone marrow edema within the talus, os trigonum, increased signal at synchondrosis, fluid accumulation around the posterior talus and tibia, and synovitis with thickening of posterior ligaments ( Figures 13 , 14 ).50 In certain populations such as ballet dancers, who frequently practice maximal plantar flexion, hyaline-like cartilage can form on the posterior talus, appearing as low-signal intensity on T2 images.51
( A ) Axial T2 fat-saturated image demonstrates thickening of the posterior talofibular ligament. ( B ) Axial T2 fat-saturated image demonstrates thickening of the posterior intermalleolar ligament. ( C ) Sagittal T2 fat-saturated image demonstrates abnormal edema adjacent to the posterior talus suggestive of posterior ankle impingement. ( D ) Sagittal T1 image demonstrates a prominent os trigonum.
( A ) Lateral radiograph of the ankle demonstrates an os trigonum. ( B ) Axial T2 fat-saturated image shows reactive marrow edema-like signal of the os trigonum, fluid across the synchondrosis, and marked posterior synovitis. ( C ) Sagittal T2 image shows reactive marrow edema-like signal of the talus and os trigonum with reactive posterior tibiotalar and subtalar joint effusions.
Treatment
Despite mixed study findings in the literature, standard initial therapy of AISs consists of nonsteroidal anti-inflammatory drugs, physical therapy, and intra-articular steroid injections for 3-6 months to reduce stress on the joint and promote healing.8, 9, 11, 52
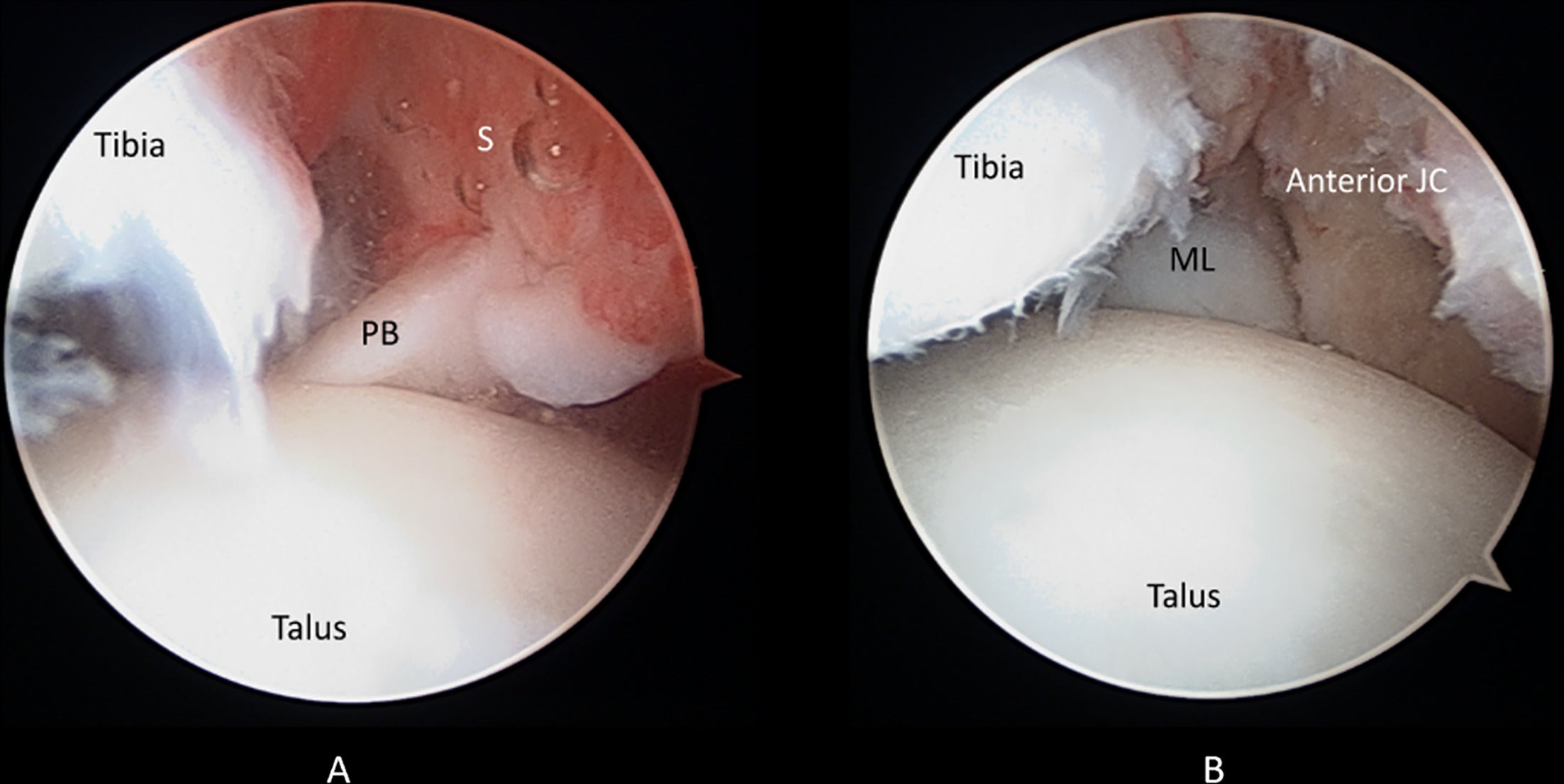
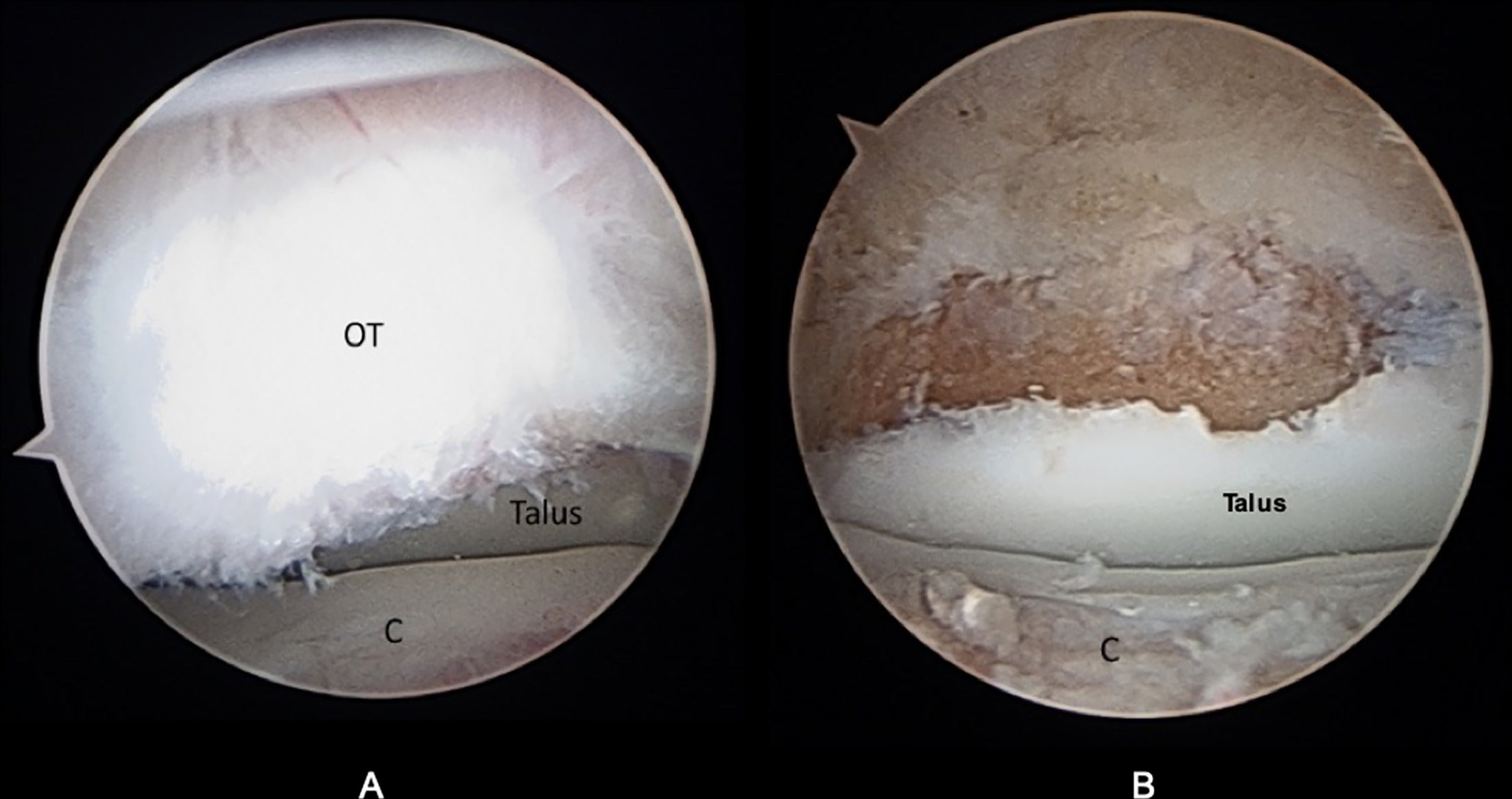
Surgical intervention may be warranted if pain or restriction persists beyond 6 months. Surgery aims to remove osteophytes, debride inflamed soft tissue and loose fragments in the joint space, and correct coexisting contributing conditions.6 - 8, 11, 15, 22, 34 While open arthrotomy was once considered the standard procedure, complications such as cutaneous nerve entrapment, long extensor tendon damage, wound dehiscence, and hypertrophic scar tissue formation led to a shift toward arthroscopy, reducing recovery times and complication rates ( Figures 15 - 19 ).6, 11, 16, 53 - 55
Surgical management of anterior impingement. ( A ) Anterolateral arthroscopic view shows talar spur, with arrows pointing at approximate demarcation from the talus neck and shaver burr holding up the joint capsule. ( B ) Medial arthroscopic view after debridement with arrows demonstrates a restoration of the concavity of the talar neck with restoration of normal anatomic profile.
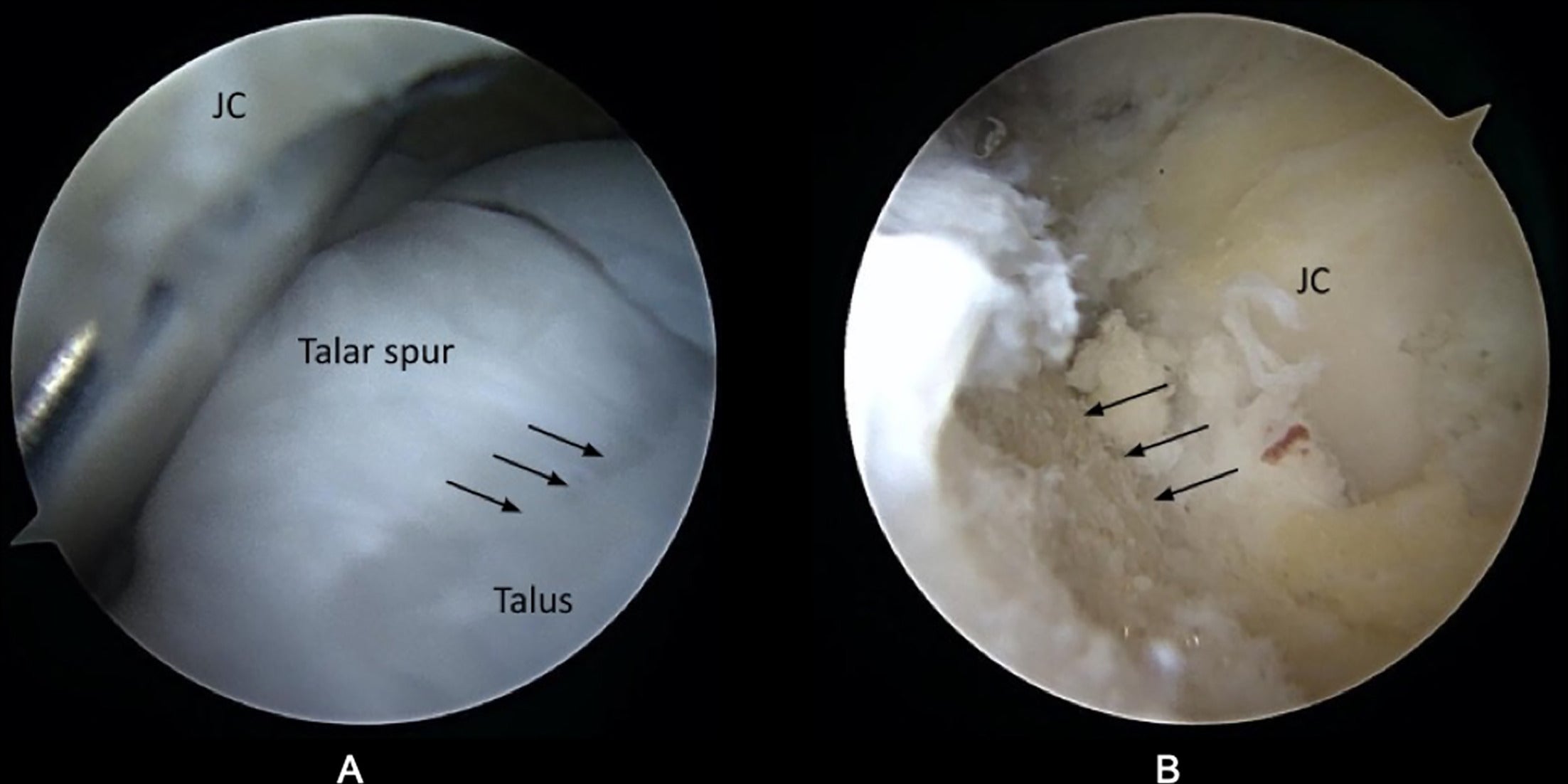
Surgical management of anterior impingement. ( A ) Anterolateral arthroscopic view of relative anatomy shows a loose body encased in arthrofibrotic bands with the tibia seen behind. ( B ) Central arthroscopic view of deformation after the loose body and arthrofibrotic band were debrided showing chondromalacia on the tibia.
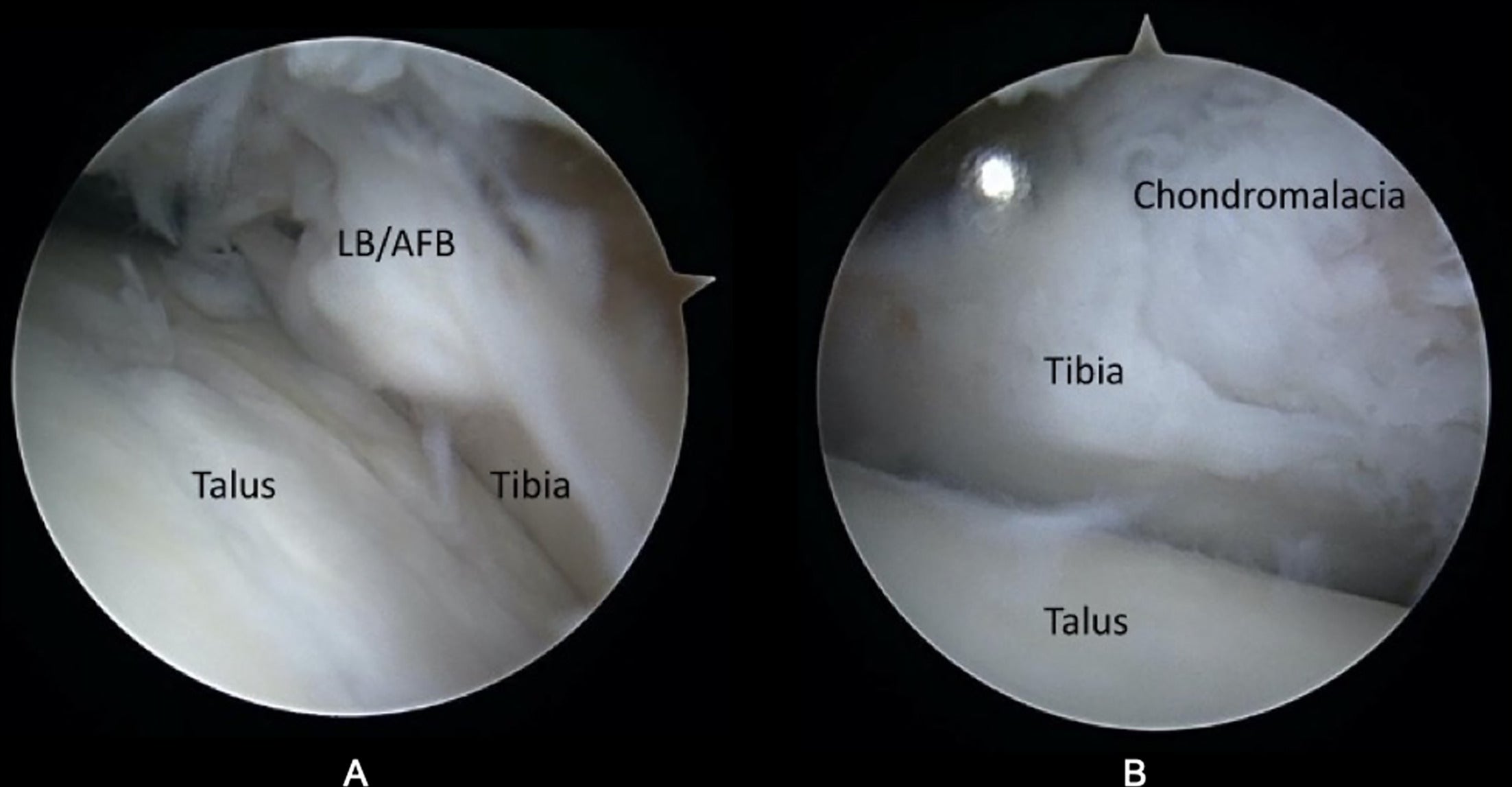
: Surgical management of anterolateral impingement. ( A ) Anterolateral arthroscopic view with meniscoid lesion in syndesmosis. ( B ) Arthroscopic view of anatomy after debridement of syndesmotic meniscoid lesion.
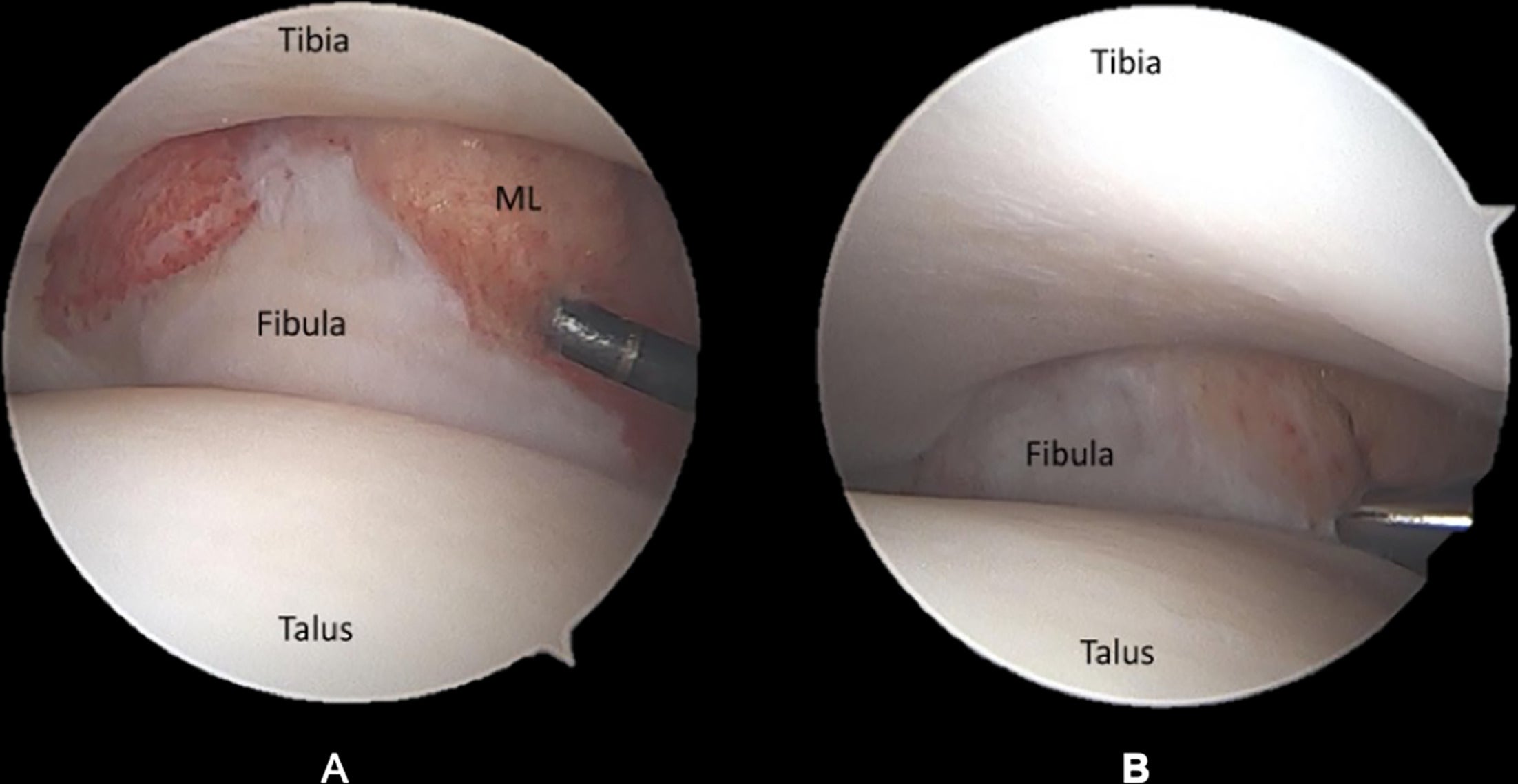
Surgical management of anteromedial impingement. ( A ) Arthroscopic view of hypertrophied anteromedial plica band. ( B ) Arthroscopic view after the removal of plica band and debridement shows medial malleolus and restoration of relative anatomy.
Surgical management of posterior impingement. ( A ) Relative osseus anatomy demonstrates os trigonum, calcaneus, and talus. ( B ) Hindfoot endoscopy view shows complete os trigonum removal after resection of medial and lateral attachments.
Conclusion
Imaging plays an important role in localizing pathology and guiding treatment of AISs. Choice of modality is based largely on the pathophysiology of the impingement.
Radiography is particularly useful in cases caused by ossesous abnormalities such as AI. As mentioned earlier, 2 commonly used classification systems for AI are the AIC and OAC. Preoperative staging, especially regarding the extent of degenerative changes, is a significant factor in predicting treatment outcomes in anterior impingement types. When using AIC, arthroscopic surgical interventions have demonstrated good outcomes in type I and II AI, with less successful outcomes in type III and IV cases.19, 20 The OAC can also be predictive of outcomes; arthroscopic surgical interventions have been reported to deliver good outcomes in patients with grade O/I impingements, while not faring as well in patients with grade II/III impingments.19, 53 Van Dijk et al found that the OAC classification was a better predictor of surgical outcomesl19 ; however, Coull et al concluded that the OAC system did not provide enough detail and that patients were too broadly grouped.14 Further studies comparing the 2 classification systems as well as developing additional systems for other impingement syndromes would be useful in quantifying image findings for surgical planning.
In some cases, CT can permit a more detailed assessment of the location and burden of osteophytes and other osseous abnormalities, particularly in cases where the physical exam and history are not consistent with initial imaging findings. Indeed, more detailed imaging can sometimes change the diagnosis from a single form of impingement to a combined type, potentially redirecting the approach to treatment.56
As CT provides limited information on bone marrow and soft-tissue abnormalities, MRI can be useful in syndromes caused predominantly by soft-tissue pathology. Alternatively, patients without clinical symptoms or signs of AIS have been found to have incidental abnormalities on MR arthrography that are then confirmed at surgery.57 Thus, a thorough history and physical examination are important to accurately correlate imaging features and treat only symptomatic cases of AISs.
References
Citation
Qureshi H, Sobotie A, Hallwachs A, Pagano K, DeVita R, Barger R, Kosaraju V, Miskovsky S, Faraji N. Ankle Impingement Syndromes: What the Radiologist Needs to Know. Appl Radiol. 2025; (1):1 - 15.
doi:10.37549/AR-D-24-0064
February 14, 2025