Alveolar Capillary Dysplasia with Misalignment of Pulmonary Veins
Images




CASE SUMMARY
A 3-year-old with a history of imperforate anus and a one-day history of congestion, oxygen desaturations, and intermittent tachypnea pre sented with pulmonary hypertension and interstitial lung disease. Physical exam was nonspecific with tachypnea, mild subcostal retractions, and clear lungs bilaterally.
IMAGING FINDINGS
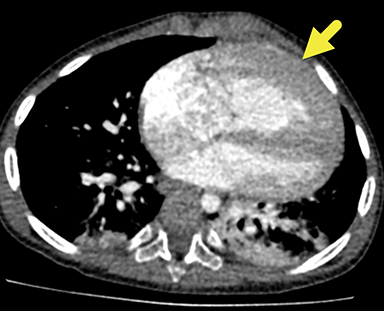
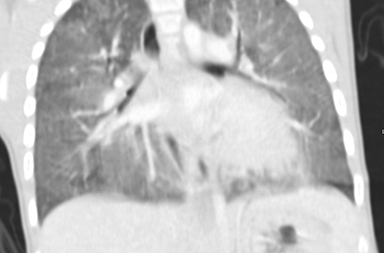
Chest CT revealed diffuse ground-glass pulmonary opacities with peripheral upper lung sparing (Figure 1). An echocardiogram revealed moderate dilation of the main pulmonary artery, moderate dilation of the right ventricle, and an elevated right ventricular pressure; however, the left ventricle was normal in size.
DIAGNOSIS
Alveolar capillary dysplasia with misalignment of pulmonary veins (ACD/MPV). Differential diagnosis includes idiopathic persistent pulmonary hypertension and congenital cardiopulmonary disease with pulmonary hypertension.
DISCUSSION
Alveolar capillary dysplasia with misalignment of pulmonary veins is a rare, congenital disease with fewer than 200 cases reported.1 MacMahon first described the condition in the literature in 1948, reporting three infants, born full-term, who developed respiratory distress and cyanosis. Autopsy revealed stromal dysplasia and decreased alveolar air space.2 Since then, reports of ACD/MPV have increased with improved characterization of clinical features and pathology, but the pathogenesis and genetics of the disease remain unclear.
Patients with ACD/MPV typically develop respiratory distress, severe pulmonary hypertension, and cyanosis in the first 24-48 hours of life, with high probability of mortality in the first month.3 However, there have been a few reported cases of infants presenting with ACD/MPV beyond the neonatal period, with more suspected being unreported, owing to the need for biopsy or autopsy for diagnosis.4
In this case, lung biopsy revealed patchy features of lobular underdevelopment, concentric medial muscular hypertrophy, areas of deficient capillaries and poor apposition, as well as areas of near-normal capillary profiles, abnormal artery/vein pairing, extension of mural smooth muscle into distal acinar vessels, and dilation of the lymphatic vessels.
Patients with delayed ACD/MPV tend to present with mild or absent tachypnea at birth but may remain asymptomatic for months or years. One report suggests that viral infections may trigger a pulmonary hypertensive crisis in delayed-onset patients, owing to the abnormal pulmonary vasculature.
Systemic abnormalities may also be present with ACD/MPV. Concurrent gastrointestinal and urogenital abnormalities, including anal atresia and redundant colon, occur in 50-80% of ACD/MPV patients.1 Treatment is limited, with only transient or no response to nitric oxide, pulmonary vasodilators, or extracorporeal membrane oxygenation (ECMO); as in this case, lung transplant is the only effective form of treatment.4
Imaging, such as echocardiography, can be helpful for excluding differential diagnoses such as congenital heart disease that may explain pulmonary hypertension. Diffuse ground-glass attenuation on chest radiography in neonates and chest CT beyond the neonatal period are often seen in ACD/MPV, but imaging can also appear normal.1
Histological examination of a lung biopsy is the gold standard for diagnosing ACD/MPV. Common histological findings include medial hypertrophy of pulmonary arteries and muscularization of arterioles, decreased number of capillaries, immature lobular development, and malposition of pulmonary veins adjacent to small pulmonary arteries.5 The constellation of these histological findings is diagnostic for ACD/MPV. Lymphangiectasis has additionally been reported to be associated with ACD/MPV.7
Variations in histology may explain milder forms of ACD/MPV. One report correlates survivorship of ACD/MPV patients with increased capillary density and apposition to the alveolar epithelium.5 Ito has also noted a correlation of patchy capillary reduction and abnormal alveolar air space, with delayed clinical presentation; his findings are consistent with previous findings in the literature. The presence of normal lung tissue bilaterally on imaging is also associated with a milder phenotype.4
The genetics of ACD/MPV remain unclear, as 60% of affected patients have no known cause. However, in 40% of patients, mutations in the FOXF1 gene or microdeletions of 16q24.1-containing the FOX transcription gene cluster- have been associated with ACD/MPV. FOXF1 is expressed in muscle cells of the lung and has been implicated with pulmonary vascular abnormalities in a murine model.1
Differential diagnosis includes idiopathic persistent pulmonary hypertension, which can be excluded as it typically completely resolves with respiratory interventions, including ECMO or pulmonary vasodilators.
CONCLUSION
ACD/MPV should be considered in patients who present with pulmonary hypertension with little improvement from respiratory interventions. While classically a neonatal disease, milder forms of the disease can present beyond the neonatal period. Histological examination of lung biopsy with the constellation of features described above is considered diagnostic; imaging is useful for supporting the diagnosis during work-up. Genetic testing may also be helpful for discerning heritable forms of the disease.
REFERENCES
- Bishop NB, Stankiewicz P, Steinhorn RH. Alveolar Capillary Dysplasia. American Journal of Respiratory and Critical Care Medicine. 2011;184(2):172-179. doi:10.1164/rccm.201010-1697ci.
- MacMahon HE. Congenital alveolar dysplasia of the lungs. Am J Pathol. 1948;24(4):919–931.
- Towe CT, White FV, Grady RM, et al. Infants with Atypical Presentations of Alveolar Capillary Dysplasia with Misalignment of the Pulmonary Veins Who Underwent Bilateral Lung Transplantation. The Journal of Pediatrics. 2018;194. doi:10.1016/j.jpeds.2017.10.026.
- Ito Y, Akimoto T, Cho K, et al. A late presenter and long-term survivor of alveolar capillary dysplasia with misalignment of the pulmonary veins. European Journal of Pediatrics. 2015;174(8):1123-1126. doi:10.1007/s00431-015-2543-3.
- Deutsch GH, Young LR, Deterding RR, et al. Diffuse lung disease in young children: application of a novel classification scheme. Am J Respir Crit Care Med. 2007;176(11):1120–1128. doi:10.1164/rccm.200703-393OC
- Melly L, Sebire NJ, Malone M, Nicholson AG. Capillary apposition and density in the diagnosis of alveolar capillary dysplasia. Histopathology. 2008;53(4):450-457. doi:10.1111/j.1365-2559.2008.03134.x.
- Vassal HB, Malone M, Petros AJ, Winter RM. Familial persistent pulmonary hypertension of the newborn resulting from misalignment of the pulmonary vessels (congenital alveolar capillary dysplasia). Journal of Medical Genetics. 1998;35(1):58-60. doi:10.1136/jmg.35.1.58.
Citation
M M, RB T, M R, AJ T.Alveolar Capillary Dysplasia with Misalignment of Pulmonary Veins. Appl Radiol. 2021; (2):34-35.
March 11, 2021