Abdominal Pseudocyst in a Patient with a VP Shunt
Affiliations
- 1 Lake Erie College of Osteopathic Medicine, Bradenton Campus, Bradenton, Florida
- 2 Buffalo General Hospital, Buffalo, New York
Case Summary
A middle-aged patient, with a history of long-standing hydrocephalus and ventriculoperitoneal (VP) shunt secondary to a ruptured posterior inferior cerebellar artery (PICA) aneurysm at the age of 2, presented with increasing upper extremity weakness that worsened over the course of 6 months.
A significant increase in ventricular size is observed during image comparison from a year prior.
A shunt tap revealed an opening pressure of 7 mmHg without indications of a cerebrospinal fluid (CSF) infection. A CT scan of the abdomen revealed a pseudocyst above the liver, with a catheter in situ.
The recent deterioration in the patient’s condition, characterized by progressive upper extremity weakness, notable ventricular enlargement, shunt pressure measurements, and CT findings, indicated a need for surgical intervention. Surgery was performed to address both the abdominal catheter and valve concerns identified.
Image Findings
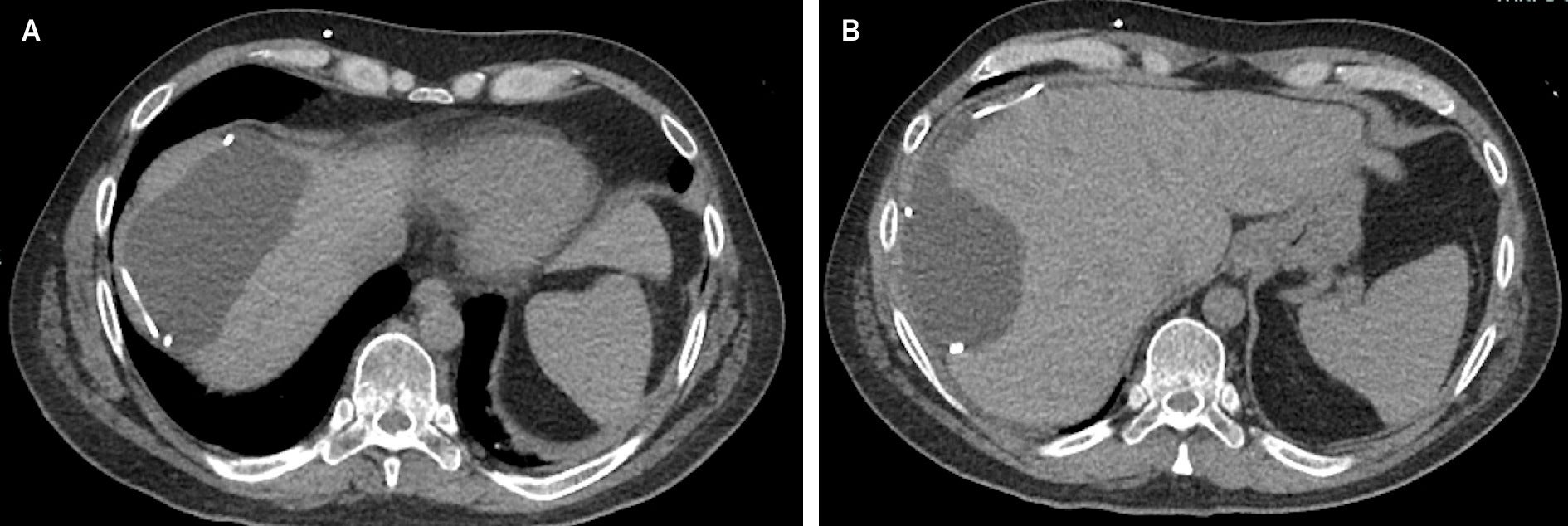
An axial CT without contrast reveals the presence of a large fluid-density mass in the right upper quadrant measuring 10.9 × 11.5 × 5.6 cm. This demonstrates a mass effect on the liver, with deformity of the hepatic contour. The VP shunt catheter can be seen as the dense curvilinear structure within the collection ( Figure 1 ).
(A, B) Axial CT without contrast shows a large mass in the right upper quadrant measuring 10.9 × 11.5 × 5.6 cm, appearing as a loculated collection that deforms the contour of the liver containing the distal tip of a VP shunt catheter.
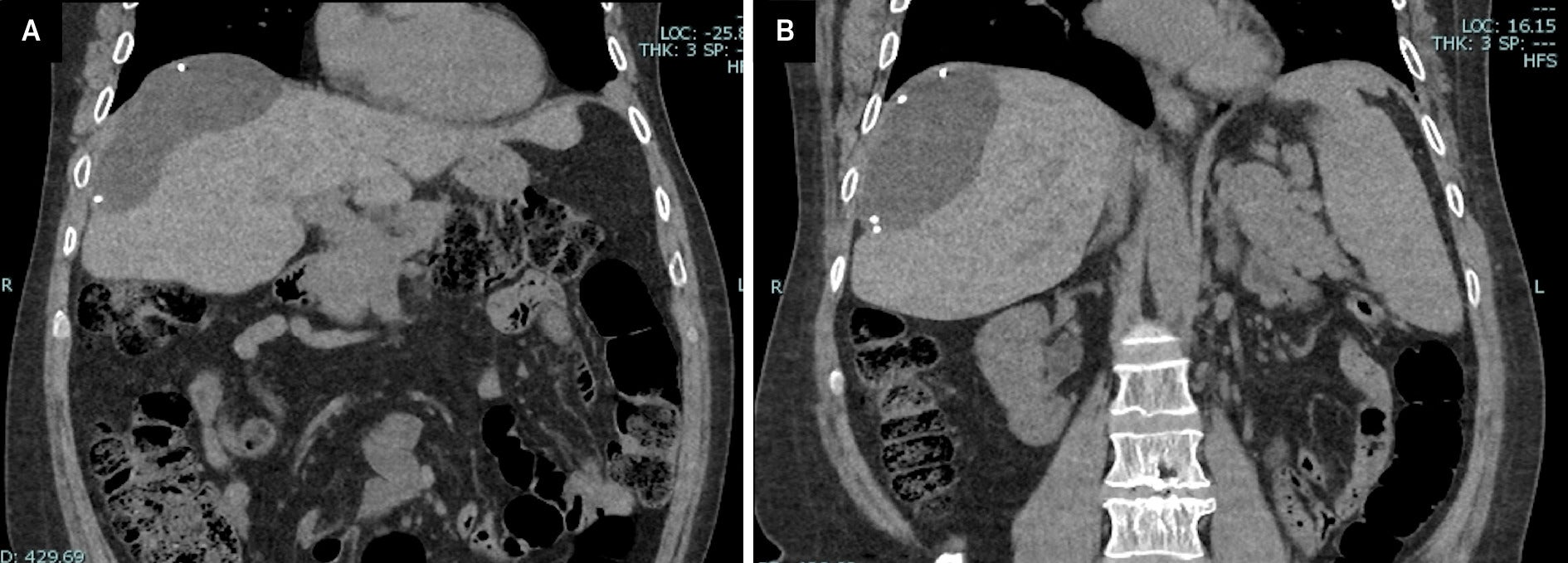
A coronal CT without contrast confirms these findings and shows the mass referenced above deforming the adjacent contour of the liver ( Figure 2 ).
(A, B) Coronal CT without contrast shows a well-demarcated abdominal mass at the superior lateral portion of the liver, deforming its contour.
Diagnosis
A diagnosis of abdominal pseudocyst (APC) was made and confirmed through imaging. Differential diagnosis of abdominal cystic mass includes pancreatic pseudocyst, lymphocele, cystic lymphangioma, mesenteric cyst, benign cystic teratoma, seroma, cystic spindle-cell tumor, and cystic mesothelioma.1
Discussion
The patient’s complex medical history, stemming from a ruptured PICA aneurysm during childhood, necessitated the use of a VP shunt for his hydrocephalus. APC is a rare long-term complication of childhood hydrocephalus, with only about 2.3% of pediatric patients who have received a VP shunt being affected by an APC later in life.2
It is crucial for the physician to account for the patient’s medical history when considering an APC, as this diagnosis occurs exclusively in the setting of a VP shunt. Consequently, it will not appear on a common list of differential diagnoses without careful consideration of the patient’s medical history. Other causes of abdominal cystic masses, such as a pancreatic pseudocyst, lymphocele, cystic lymphangioma, mesenteric cyst, benign cystic teratoma, seroma, cystic spindle-cell tumor, or cystic mesothelioma, may be more strongly considered in the absence of a history of VP shunt placement.1
APC typically manifests as well-demarcated, near water-density abdominal masses. CT imaging shows the abdominal fluid collection in close proximity to the catheter tip of the VP shunt. Associated mass effects on neighboring structures may be seen. Less commonly, APC may reside within intra-abdominal organs, adding a layer of complexity to its diagnosis and management. The variability in APC presentation underscores the importance of comprehensive imaging analysis and clinical assessment for accurate and appropriate treatment.3
The etiology of an APC is not well known. The most widely accepted mechanism is that APCs arise from an inflammatory process.3 Other proposed mechanisms related to APCs include chronic infection, foreign body reaction, and particle-like protein in CSF.3 Abdominal adhesions also potentially play a role in the pathogenesis of APCs.4 Numerous dense adhesions were found and subsequently incised in the case of this patient. These proposed mechanisms need further exploration to reach a comprehensive understanding.
An untreated APC poses multifaceted complications. These complications include inadequate CSF drainage, associated hydrocephalus, and symptomatic presentations, including abdominal discomfort and pain. Complications such as abscess formation, cellulitis, and rare instances of gastric outlet obstruction are documented in cases of infected pseudocysts. When working up the etiology of an APC, CSF studies can lead to an accurate diagnosis. A shunt tap or lumbar puncture enables the clinician to rule out catheter- or hardware-related infections. The ramifications of an untreated APC vary but often result in recurrent shunt failures and infections.4
Various interventions are used when treating an APC, depending on the clinical scenario. However, surgical resection with excision of the fibrous wall is the preferred treatment. These interventions attempt to minimize symptoms and prevent complications such as abscess formation and infection. In some cases, complete removal of shunt hardware via endoscopic third ventriculostomy may be considered.4, 5 The choice of intervention depends on many factors, such as the severity of the patient’s symptoms, the size and location of the pseudocyst in the abdominal cavity, and the patient’s overall health.
Conclusion
APC is a rare complication of an indwelling VP shunt catheters. The characteristic features of an APC on contrast-enhanced CT scans reveal well-defined abdominal fluid collection, often with mass effect, in a patient with abdominal pain and/or neurologic changes. This case demonstrates the rare occurrence of APC causing VP shunt malformation in the presence of multiple, dense abdominal adhesions. Prompt diagnosis allows the physician to initiate interventional therapies, minimize the risk of infection/abscess formation, and allow for proper management.
References
Citation
Potesta M, Guld E, Jacobson D.Abdominal Pseudocyst in a Patient with a VP Shunt. Appl Radiol. 2025;
doi:10.37549/AR-D-25-0105
October 1, 2025