Breast Arterial Calcification: Why Radiologists Should Start Reporting This Silent Risk Factor for Heart Disease
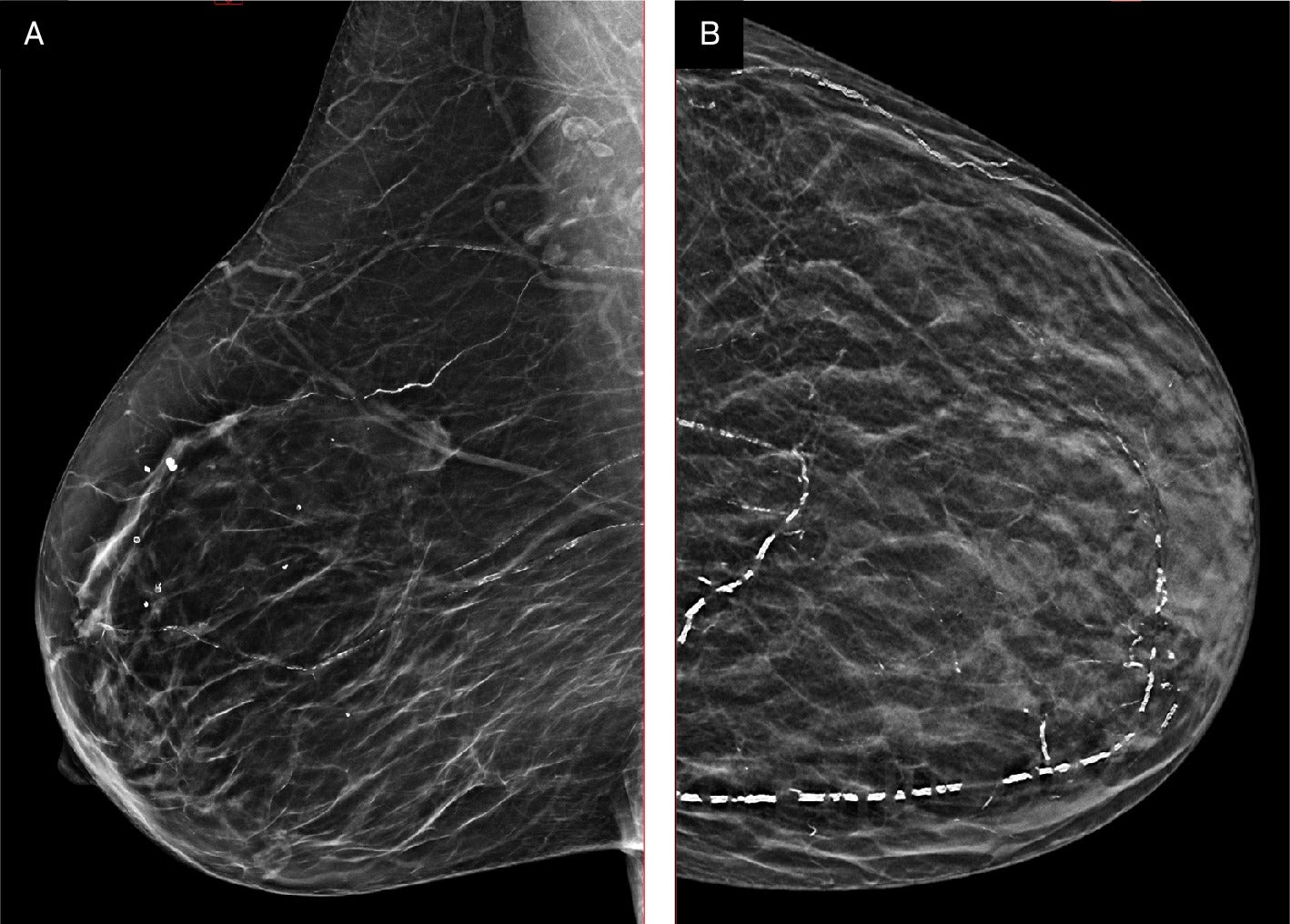
Breast arterial calcification (BAC) has long been visible to radiologists reading mammograms. It appears as characteristic linear, parallel “tram-track” calcifications outlining breast arteries1 —easy to spot, easy to classify, and entirely incidental to the task at hand: ruling out breast cancer. Because BAC is not a marker of breast malignancy, however, radiologists have historically ignored it in reports, dismissing it as a benign finding.
Yet a growing body of evidence shows that BAC is anything but benign. Its presence on mammography is strongly correlated with cardiovascular risk, including heart attacks, stroke, and cardiovascular death. That makes BAC a powerful “free” biomarker—information available to every radiologist, every day, at no additional cost, dose, or imaging burden. The challenge: radiologists must decide whether to report it.
From where Nina Vincoff, MD, stands, they should.
“We have an incredible opportunity here to do two-for-one screening for two of the biggest threats to women’s health and women’s lives,” says Dr Vincoff, who is a breast imager and the editor-in-chief of Applied Radiology . “There’s really no argument that anybody can make to me for not doing it.”
What Is BAC?
“Breast arterial calcification is an entity we’ve always seen on mammography,” explains Dr Vincoff, who until recently was the Breast Imaging Division Chief at Northwell Health in New York. “It doesn’t require special training, special equipment, or additional views. It simply appears as white linings along breast arteries.”
Importantly, BAC is not the result of the same process as the intimal calcification familiar in coronary arteries. Instead, it represents medial calcification—arterial stiffening rather than luminal narrowing. “People make much of that distinction,” noted Laurie Margolies, MD, Vice Chair for Breast Imaging at Mount Sinai Health System in New York City.
“But the bottom line is that both are associated with ischemia and infarction. Different pathways, same outcome.”
The Overlooked Killer in Women’s Health
For decades, women’s heart disease has been underdiagnosed and undertreated. Historically, prevention campaigns focused on men, while women’s symptoms were minimized or misinterpreted. “It wasn’t that long ago,” Dr Margolies recalled, “that American Heart Association pamphlets for women were all about cooking better meals for their husbands to prevent his heart attack.”
The reality, she says, is that cardiovascular disease kills more women than breast cancer, yet patients overwhelmingly fear the latter. Annual mammograms are viewed as the gold standard of preventive care, while heart health often goes unexamined, agrees Dr Vincoff.
“Women come in thinking they’ve checked the preventive care box by getting their mammogram. But they often haven’t had their cholesterol, blood pressure, or other risk factors evaluated,” she observes. “They’re so focused on breast cancer and not really thinking about heart disease at all.”
Indeed, according to the Centers for Disease Control and Prevention, more than 60 million women (44%) in the United States are living with some form of heart disease, which it labels as the leading cause of death for women in the country and says can affect women at any age.2
This makes BAC reporting uniquely powerful. A woman who thinks she’s only being screened for breast cancer may also be alerted to hidden cardiovascular risk—at the very moment she is most focused on her health.
Evidence Links BAC to Cardiovascular Risk
A robust body of literature confirms the association between BAC and adverse cardiovascular outcomes. Dr Margolies in fact co-authored a recently published study, “Breast Arterial Calcifications on Mammography: A Review of the Literature,” examining epidemiologic studies that have consistently shown that BAC prevalence rises with age, diabetes, hypertension, and chronic kidney disease—classic cardiovascular risk factors.3
Longitudinal studies link BAC to major adverse cardiac events, including myocardial infarction, stroke, and cardiovascular death, independent of traditional risk markers. In addition, the prognostic value of BAC persists regardless of statin therapy, suggesting that it provides additive risk information.
“Longitudinal studies show that BAC correlates not only with death but with major adverse cardiac events,” she says. “Cardiologists say, ‘please send us these patients and we will prevent these things.’”
The Patient Perspective: “How Dare You Not Tell Me?”
If the science were not persuasive enough, patient preference is unequivocal. In one study led by Dr Margolies, 97% of women said they would want to know if BAC was present. “The reaction was consistent: ‘How dare you know something about my body and not tell me?’” she recalls.
Dr Vincoff, meanwhile, conducted a pilot study of 500 consecutive patients. Of those with BAC, 57% spoke with their doctor about the finding within 3 months.4 Several underwent further testing and, in some cases, life-saving interventions such as stent placement or bypass surgery.
“Women can handle scary news,” she says. “They’d rather hear it and act on it than be shielded and miss the chance to prevent a heart attack.”
Lessons from Breast Density Reporting
The trajectory of BAC reporting parallels that of breast density, says Dr Margolies. For decades, density was acknowledged but rarely communicated. Advocacy from patients—women who developed advanced cancers despite “normal” mammograms—changed the landscape. Federal law now mandates breast density notification.
“We don’t want to repeat that history,” Dr Margolies cautioned. “We shouldn’t need patients to start foundations to force us to do the right thing. We already know BAC is important. We should act now.”
One Click Is All It Takes
Radiologists may hesitate, worrying about reporting burden. In reality, the workflow impact is negligible. Drs Vincoff and Margolies point out that radiologists already evaluate all calcifications carefully, distinguishing suspicious morphologies from benign or vascular.
“That decision is already made internally,” Dr Vincoff explained. “Reporting BAC is simply putting words to the thought process you’ve already had.”
Structured reporting makes it even easier. At Northwell Health, Dr Vincoff’s team adopted the Canadian Society of Breast Imaging grading scale (0‐3) and built it into reporting templates. Radiologists select the grade with a single click. Patients receive plain-language explanations through patient-friendly reporting systems, allowing them to discuss results with their physicians.
“This is trivial to do,” Dr Margolies emphasizes. “Literally one click.”
Addressing Skepticism: “It’s Not in My Lane”
Why, then, has reporting lagged? According to Drs Vincoff and Margolies, perceived irrelevance is one reason: some radiologists argue BAC is outside the lane of breast imaging. Another is pathophysiologic quibbling: critics highlight differences between medial and intimal calcification, even though the presence of both suggests a referral for cardiovascular evaluation is in order.
In addition, some argue over the absence of guidelines—unlike BI-RADS for breast findings, no US authority mandates BAC reporting. Finally, critics cite the potential for uncertainty: without standardized management pathways, radiologists fear burdening fellow clinicians with “what next?” questions.
But these objections are eroding. Cardiologists have published studies on BAC for decades, and radiologists must catch up, says Dr Vincoff. Canadian guidelines already encourage reporting, and US studies are rapidly expanding.
“Yes, we don’t yet know the perfect management algorithm,” Dr Vincoff acknowledged. “But the only way we’ll learn is by reporting, collecting data, and studying outcomes. Waiting accomplishes nothing.”
Practical Considerations
For radiologists ready to adopt BAC reporting, Drs Vincoff and Margolies recommend the following straightforward framework:
-
Use structured language: Incorporate a standardized BAC grading scale such as the one developed by the Canadian Society of Breast Imaging (0 = none; 1‐3 = increasing severity).
-
Report presence/absence in all screening mammograms: Err on the side of inclusion; any BAC warrants attention. A simple yes/no checkbox can work.
-
Educate referrers: Share literature and institutional protocols with referring clinicians, especially OB/GYNs, who may be unaccustomed to cardiovascular findings on mammograms.
-
Provide patient-friendly explanations: Whether via portals, reports, or handouts, ensure patients understand the finding and why follow-up matters.
-
Encourage cardiovascular evaluation: Patients with BAC should undergo comprehensive cardiovascular risk assessment—lipids, blood pressure, diabetes screening, smoking history, and possibly cardiology referral.
The Future of BAC Reporting
The field is moving quickly. Institutions like Northwell and Mount Sinai now universally report BAC. National attention is growing, with research about BAC reporting being published not only in radiology journals but in high-profile cardiology venues like the Journal of American Cardiology Advances.5
Ongoing research will clarify prevalence, refine grading utility, and establish evidence-based management pathways. Early data from Northwell suggest that BAC is present in about 15% of screening mammograms, a prevalence far exceeding breast cancer detection rates, says Dr Vincoff. She argues that the findings underscore BAC’s potential as a major public health tool.
“[Reporting BAC] is so easy for us to do, and there’s really no excuse for not doing it,” she reiterates. “We can change women’s lives just by empowering them with those kinds of pieces of information.”
“We may end up finding more cardiovascular disease than breast cancer through BAC reporting,” agrees Dr Margolies.
Right MLO (A) and left CC (B) views of a breast with Grade 3 breast arterial calcification. Images courtesy Canadian Society of Breast Imaging.
References
Citation
Jalkiewicz J. Breast Arterial Calcification: Why Radiologists Should Start Reporting This Silent Risk Factor for Heart Disease. Appl Radiol. 2025;(4):.
doi:10.37549/AR-D-25-0125
October 1, 2025