Superior Gluteal Artery Pseudoaneurysm
By Najmi N, Darwish SET, Zaer N





CASE SUMMARY
An otherwise healthy 25-year-old presented with complaints of severe left gluteal pain. Approximately 2 months previously, the patient sustained a stab wound to the left buttock. At that time, a contrast-enhanced CT (CECT) performed at another facility demonstrated a 1.5 cm focal pooling of contrast in the deep left gluteal musculature with no intramuscular hematoma or active extravasation. The wound was packed, and the patient discharged. On presenting at our hospital, the patient complained of severe and unremitting left gluteal pain, along with paresthesia in the left distal calf/ankle region.
IMAGING FINDINGS
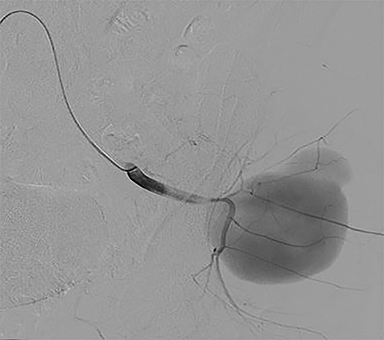
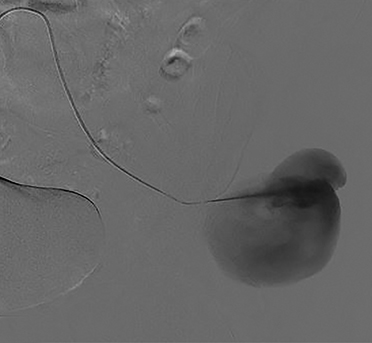
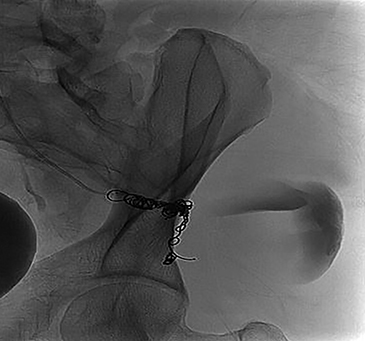
Initial CECT of the pelvis in the arterial phase demonstrated a 1.5 cm focal pooling of contrast adjacent to the superior gluteal artery (SGA) with no evidence of active extravasation or hematoma (Figure 1). A subsequent CECT of the pelvis in the portovenous phase demonstrated a large, lobulated, and partially thrombosed pseudoaneurysm, measuring approximately 11 cm in diameter and arising from the left SGA (Figure 2). Selective catheterization of the proximal left SGA and angiography confirmed the presence of an arterial pseudoaneurysm (Figure 3).
DIAGNOSIS
Superior gluteal artery pseudoaneurysm
DISCUSSION
Pseudoaneurysms of the gluteal artery are rare, constituting less than 1% of all pseudoaneurysms. They are more common in the SGA than in the inferior gluteal artery (IGA). Although the exact incidence of SGA pseudoaneurysms is unknown, fewer than 150 cases have been reported.1,2 Blunt and penetrating pelvic trauma are the most common causes of pseudoaneurysm, followed by pelvic surgeries and interventional procedures like bone marrow biopsy, mycotic infections, connective tissue disorders, vasculitis, and atherosclerosis.1,3
Pseudoaneurysms caused by trauma may present a weeks to years after the initial incident. Symptoms are nonspecific; they include buttock and sciatic pain, pressure in the buttock, and swelling. Occasionally a pulsation or bruit is observed over the mass, which may help to differentiate it from other diagnoses.4
As these lesions often present with gluteal swelling, the two most important differential diagnoses are abscess and soft-tissue mass. Misdiagnosing these lesions as an abscess or soft-tissue mass can result in a life-threatening complication if the patient undergoes aspiration or biopsy.1
High flow from the SGA can lead to a rapidly enlarging pseudoaneurysm and be potentially fatal due to eventual rupture and hemorrhage.3 The preferred modality for diagnosis is CT angiography (CTA), which can exclude the other aforementioned causes of gluteal swelling. The pseudoaneurysm appears as a contrast-filled structure communicating with an artery.2 Color Doppler ultrasound (US) will show characteristics of turbulent flow within a pseudoaneurysm (yin-yang sign).5
As in our case, endovascular embolization is the first-line treatment for non-complicated pseudoaneurysms; the procedure effectively achieves complete thrombosis with fast recovery and decreased risk of iatrogenic nerve and arterial injuries.4 Short-term follow-up with CTA should be considered to ensure complete thrombosis. In addition to embolization, stent grafting and direct thrombin injection have been suggested.5 Open surgery is also an option when endovascular therapy fails to repair the aneurysm or control the compressive symptoms.1,5
CONCLUSION
Superior gluteal artery pseudoaneurysms are rare but should be considered as a differential diagnosis of gluteal swelling and pain, especially in patients with a history of trauma. Treatment should be considered even with small SGA pseudoaneurysms, as continuous high arterial flow risks progressive enlargement and rupture. Endovascular embolization can achieve complete thrombosis with selective precision and minimal to no collateral injury. Short-term follow-up with CTA should be considered to ensure complete thrombosis.
REFERENCES
- Taif S, Derweesh A, Talib M. Superior gluteal artery pseudoaneurysm presenting as a gluteal mass: case report and review of literature. J Clin Imaging Sci. 2013;3:49. Published 2013 Oct 29. doi:10.4103/2156-7514.120805
- Corbacioglu KS, Aksel G, Yildiz A. Ruptured superior gluteal artery pseudoaneurysm with hemorrhagic shock: Case report. Turk J Emerg Med. 2016;16(1):26–28. Published 2016 Mar 10. doi:10.1016/j.tjem.2015.10.002
- Sueyoshi E, Sakamoto I, Nakashima K, Minami K, Hayashi K. Visceral and Peripheral Arterial Pseudoaneurysms. AJR Am J Roentgenol. 2005;185:741–9.
- Babu A, Gupta A, Sharma P, Ranjan P, Kumar A. Blunt traumatic superior gluteal artery pseudoaneurysm presenting as gluteal hematoma without bony injury: A rare case report. Chin J Traumatol. 2016;19(4):244–246. doi:10.1016/j.cjtee.2015.11.018
- Saad PF, Saad KR, Armstrong DM, Soares BL, de Almeida PH, Razuk Filho Á. Inferior gluteal artery pseudoaneurysm related to intramuscular injection. Int J Surg Case Rep. 2014;6C:29–32. doi:10.1016/j.ijscr.2014.10.080
Affiliation: St Vincent Hospital, Worcester, MA
