Interventional Radiology: Thirty Years of Innovation and Still Climbing

As I enter my fourth decade in the field of Interventional Radiology, I marvel at the advances my specialty has made over the past 30 years.
Throughout, these advancements have been in keeping with these 5 essential pillars: Patient Safety, Research Initiatives, Innovation, Didactical excellence, and Evolution of use and techniques (PRIDE).
These advancements can be grouped into four categories: Catheters/Wires, Diagnostic and Therapeutic Infusions, Specialty Items and, most significantly, Imaging.
Catheters and Wires
Progressively smaller caliber catheters, wires, and access sets allowed revolutionary changes in the diagnostic and treatment opportunities in IR.
This, accompanied with pre-shaped catheters, hydrophilic wires and stiff exchange wires as well as the seemingly constant advancements in microcatheters and steerable microwires, allowed interventionalists to reach previously unimagined targets.
Diagnostic and Therapeutic Infusions
Was there ever world without non-ionic contrast?
The answer is frighteningly, yes. Numerous severe contrast reactions and cases of contrast-related nephropathy have been avoided as a result of this advance in contrast agent development.
The introduction of thrombolytic agents, starting with Streptokinase, followed by Urokinase, and now tPA (Tissue Plasminogen Activator) as a tool to treat limb-threatening ischemia, thrombosed dialysis grafts, and other acute and sub-acute arterial and venous thromboses has allowed the treatment of critically-ill patients in a swift, efficacious, and cost-effective manner.
The addition of a variety of liquid and particulate embolic agents and intravascular occlusion devices, as well as the introduction of Y-90 (an isotope of yttrium) as a therapeutic option has revolutionized the IR treatment of trauma and oncology patients.
Specialty Devices
Among the most significant device advancements have been the development of intravascular stents including balloon-mounted, self-expanding, covered stents and flow diversion stents.
Intravascular filters have also advanced from early devices which were permanently placed using 24F dilators, to modern filter devices which can be placed via 6F sheaths and then percutaneously removed when no longer required.
The sequelae related to long-term indwelling IVC filters are reduced and all patients receiving a removable filter are entered in a registry and followed until removal.
The ease of placement, effectiveness, and safety of intravascular stents has changed the management of patients suffering from atherosclerotic and traumatic arterial and venous injury as well as hepatobiliary disease.
A growing armamentarium of thrombectomy devices will be added to this list.
Imaging
The first game-changer during my career was the advent of digital angiography.
Digital angiography allowed vastly improved images with reduced contrast load and radiation dose to the patient and staff. This was a major advance for patient safety.
The ability to bring a portable ultrasound unit in the angiography suite allowed real-time visualization for access of vasculature, bile ducts, renal pelvises, fluid collections, etc. with relative ease and safety.
Further advancements in ultrasound technology included ICE (Intra-Cardiac Echo) and IVUS (Intravascular ultrasound). This allowed the operator to visualize the needle at the exact point it enters a portal vein during a TIPS, saving countless needle passes and the potential complications.
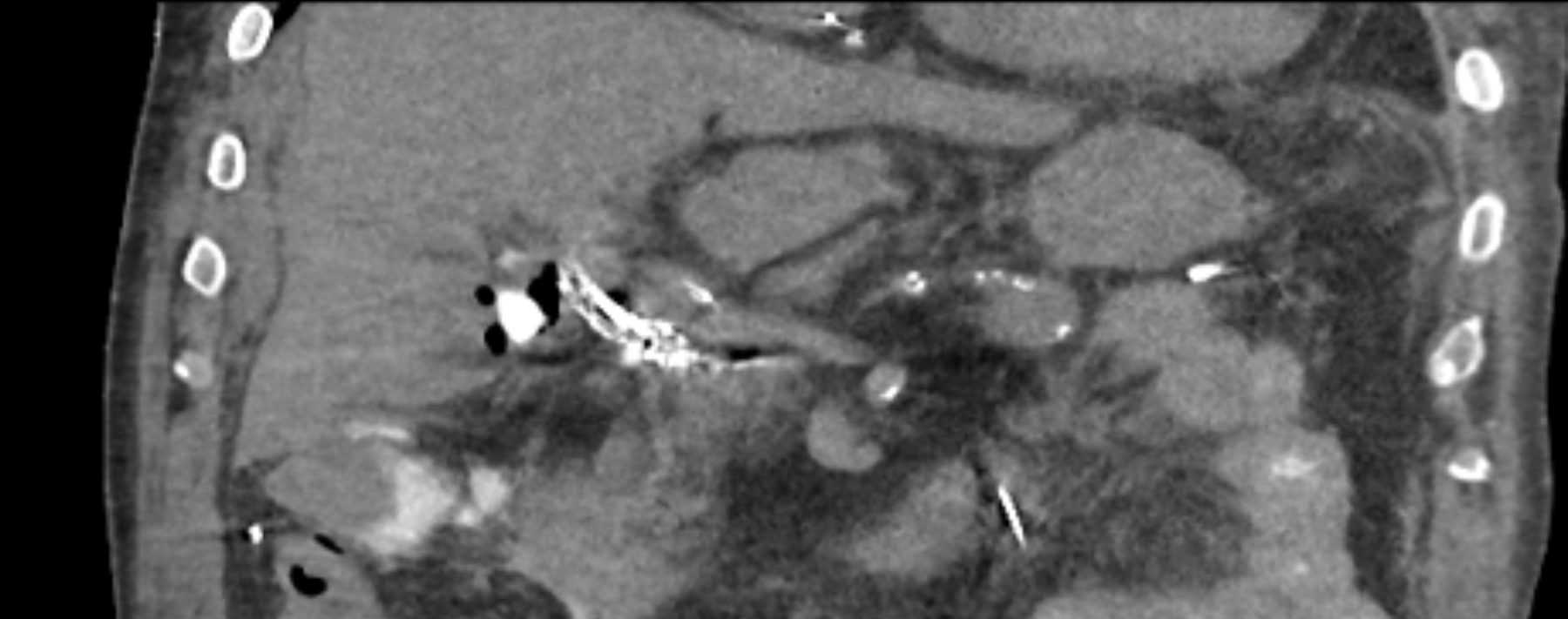
Most recently, the introduction of 4D-CT (Figure 1) has produced a seismic change in not only how IR can be practiced but in its referral pattern. Current and future IR trainees will never know the fear of operating blind while recannulating an obstructed SVC, the uneasiness that comes with, “Is my catheter in the right place”, or if the infusion catheter is precisely within the small vessel feeding the hepatic malignancy.
This has allowed the rapid expansion of an entire subspecialty of IR – Interventional Oncology. The ability to provide fluoroscopy, angiography and computed tomography in the same procedure suite has exponentially expanded the opportunities in the diagnosis and treatment of oncology and trauma patients. Newer treatments now include prostatic artery embolization for benign prostatic hypertrophy, arterial embolization in selective cases of osteoarthritis, and the percutaneous treatment of benign and malignant bony lytic lesions.
On to Greater Heights
Exciting as these developments have been, I can only imagine what amazing advancements await us in the next 30 years. Adding robotics to our current 4D-CT suite along with reducing radiation dose to miniscule levels are on the horizon.
In a shockingly short period of time, I’ve gone from dipping a straight, 7F catheter into a hot water bath to shape it, to asking my technologist to do a quick CT on the patient in the 4D-CT suite to confirm that my specialty wire and catheter have successfully traversed the 10 year-old central venous obstruction.
Arguably the greatest achievement of all has been our evolution into primary care providers. We have always been the physicians open to collaboration with other specialties. But it became evident that to truly make the maximal imprint on the field, we must be involved at all levels of care. IR physicians now staff bustling clinics and provide comprehensive longitudinal care. With the same robust vision, ingenuity, and desire to care for patients with diseases previously deemed untreatable, the entire IR care team will continue to adhere to the 5 pillars of PRIDE while raising the field of Interventional Radiology to even greater heights.
