Hydranencephaly
By Rosette TH, Towbin RB, Schaefer CM, Towbin AJ, Aria DJ
Case Summary
A term newborn with an enlarged head and normal reflexes; brain anomaly was identified on prenatal ultrasound imaging.
Image Findings
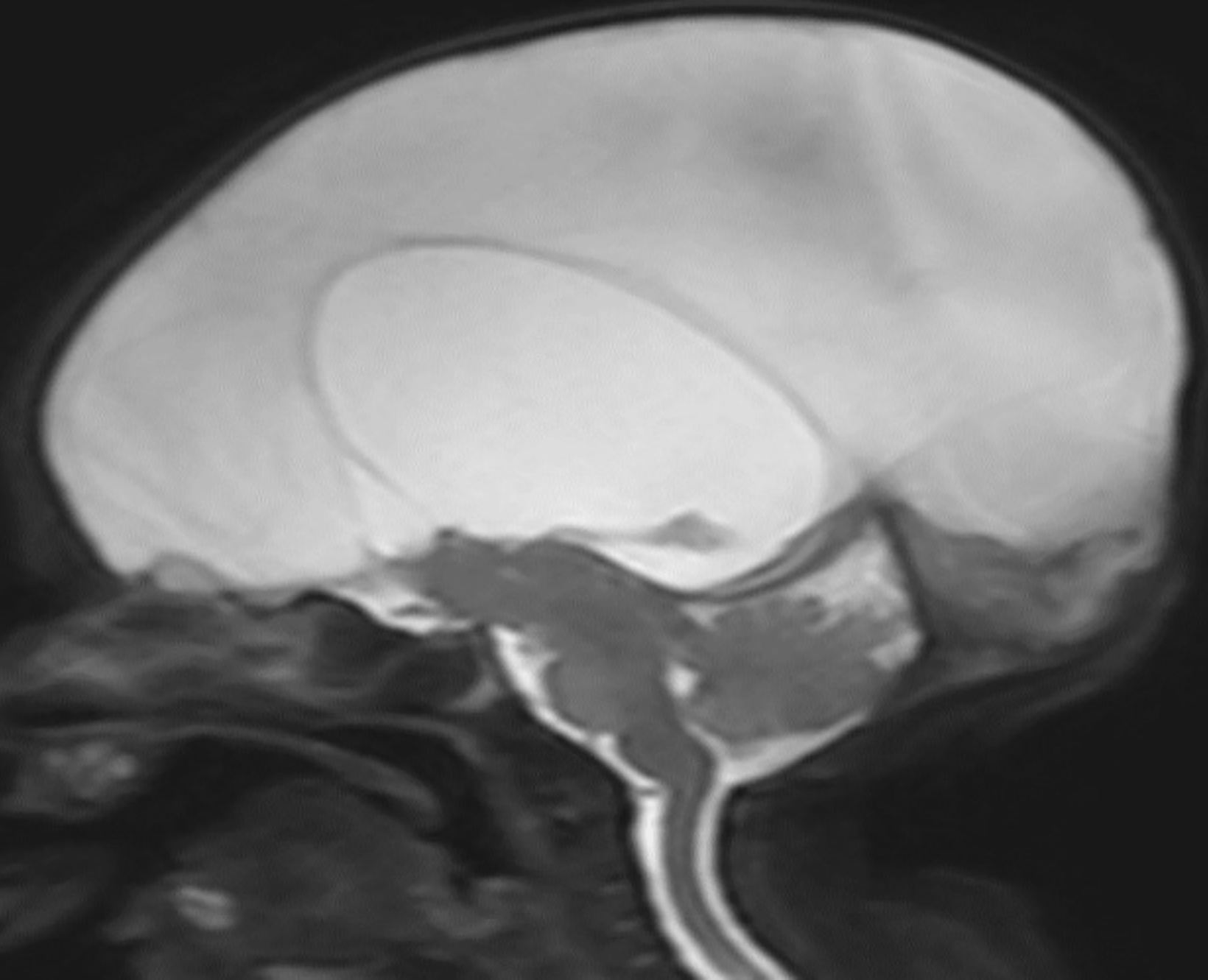
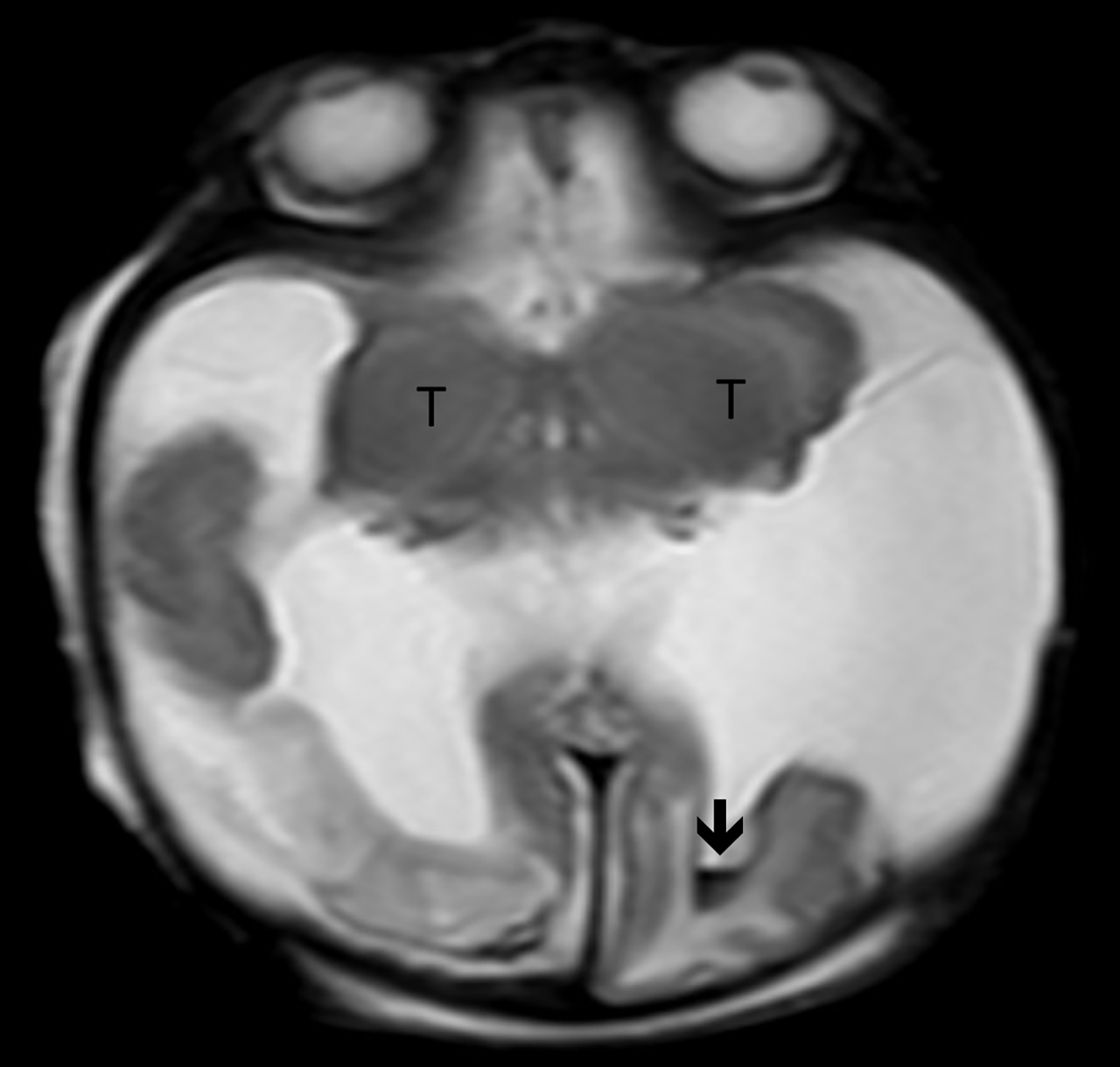
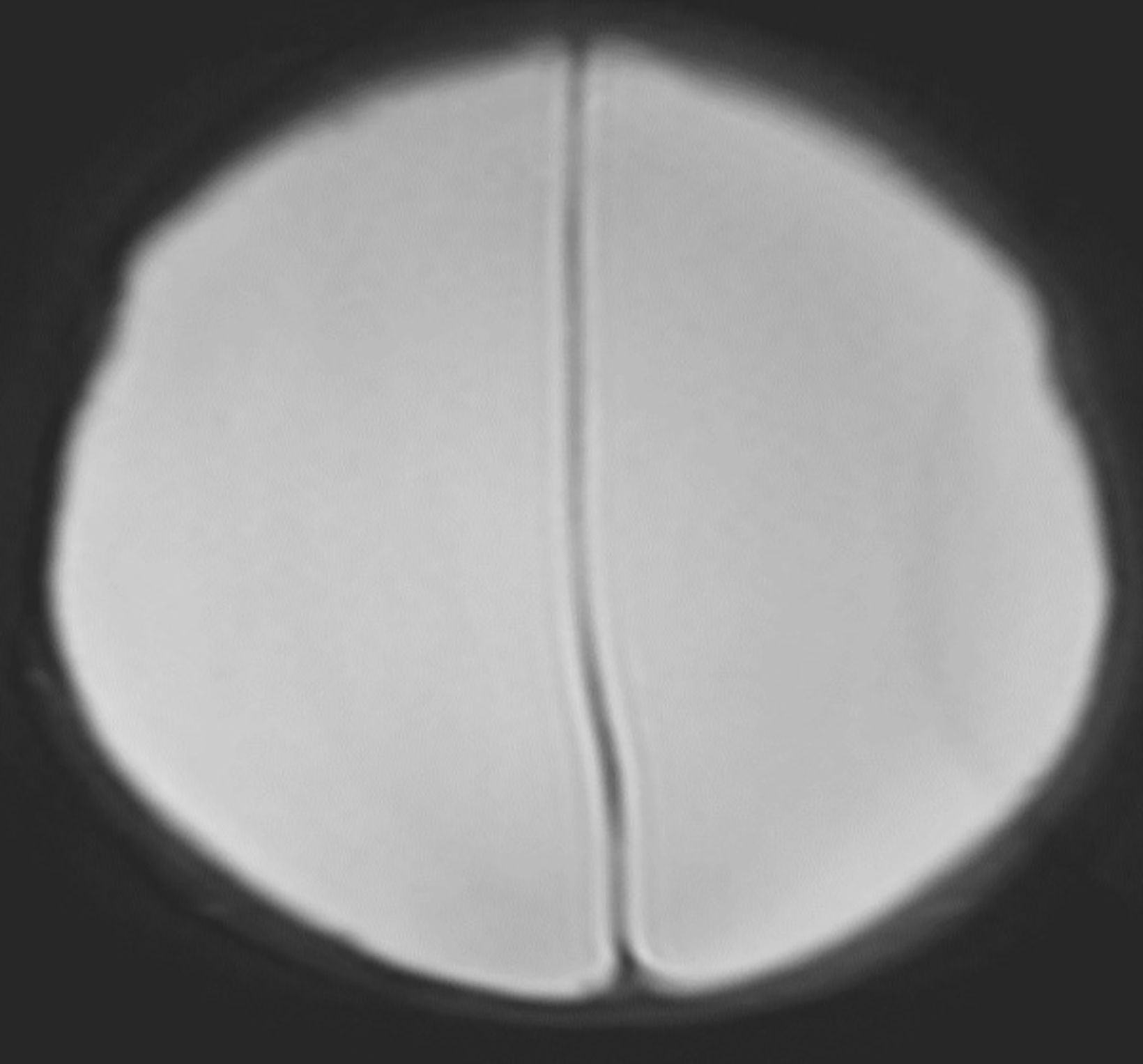
A severe brain anomaly was diagnosed prenatally by ultrasound. Postnatal brain magnetic resonance imaging revealed near-complete absence of brain tissue above the tentorium, with only a small component of the right posterior parietal and bilateral occipital lobes present. The brainstem, cerebellum, and thalami were identified below the tentorium. A normal falx cerebri was noted.
Diagnosis
Hydranencephaly.
Differential diagnosis includes severe hydrocephalus (as can be seen in the setting of aqueductal stenosis) and holoprosencephaly.
The lack of a thin rim of normal brain tissue helps to exclude severe hydrocephalus while the lack of parenchymal fusion across the midline and presence of a normal falx excludes the diagnosis of holoprosencephaly.
Discussion
Neurodevelopmental disorders occur during the early phases of embryonic development. Hydranencephaly is one type of neurodevelopmental disorder that leads to the absence or near-total absence of the cerebral hemispheres.1 Structures that typically remain intact include the cranial vault, meninges, thalami, midbrain, and cerebellum.1 The basal ganglia may also be present.
Hydranencephaly is an in utero destructive lesion of previously normally formed brain.2 Several hypotheses attempt to describe the etiology of this condition. They include: 1) bilateral internal carotid artery occlusion leading to infarction; 2) primary agenesis of the neural wall; and 3) intrauterine infection. It is also a component of Fowler syndrome (proliferative vasculopathy and hydranencephaly-hydrocephaly syndrome).1, 2 If the condition goes undiagnosed prenatally or at the time of birth, then presenting signs usually include seizures, respiratory failure, and poor posture while being in a vegetative state.
The hypothesis regarding internal carotid artery (ICA) occlusion is the most widely accepted explanation for hydranencephaly, as an intact blood supply is necessary for normal fetal brain growth and development. Early ICA occlusion can lead to blockage of the downstream arteries that supply the cerebral hemispheres, leading to infarction of the brain with subsequent reabsorption of the injured brain tissue as the infarcted brain is replaced by cerebrospinal fluid.
Hydranencephaly can be diagnosed using any imaging modality that can evaluate the fetal or newborn brain. Imaging findings include macrocephaly in utero and absence of the supratentorial brain, with a large, cerebrospinal fluid collection in the cranial vault. The brain structures primarily supplied by the posterior cerebral artery circulation (brainstem, midbrain, thalami, and portions of the basal ganglia) are preserved. Additionally, small portions of the parietal and occipital lobes may be preserved if they are supplied by small vessels outside of the ICA distribution. There is variable presence of the third ventricle. The falx cerebri may be incomplete; however, it is usually present and can help to distinguish hydranencephaly from alobar holoprosencephaly.1 Prenatal diagnosis can be made with obstetrical ultrasound or fetal MRI during the second trimester.6
The prognosis for hydranencephaly is very poor. Most patients live for weeks to months after birth. However, there are case reports of patients living up to 22 years.8,9 Disease severity may be indicated by degree of brain loss and associated anomalies. Treatments focus on managing symptoms, especially treating the hydrocephalus and seizures.
Conclusion
Hydranencephaly is a congenital neurodevelopmental anomaly in which there is an absence of the cerebral hemispheres and intact infratentorial structures. It is generally thought to occur as a result of bilateral occlusion of the ICAs. Diagnosis can be made prenatally or postnatally using ultrasound, CT, or MRI. Imaging findings include the presence of primitive brain structures, variable presence of the falx cerebri, and total or near-total absence of the cerebral hemispheres. There is no cure for hydranencephaly, and the prognosis is poor.
References
- Pretorius, DH, et al. Diagnosis of brain neuropathology in utero. Neuroradiolog., 1986; 28(5-6): 386-397.
- Greene MF, Benacerraf B, Crawford JM. Hydranencephaly: US appearance during in utero evolution. Radiology. 1985; 156(3): 779-780.
- Menshawi K, Mohr JP, Gutierrez J. A functional perspective on the embryology and anatomy of the cerebral blood supply. J Stroke. 2015; 17(2): 144-158.
- Brismar J. Persistent hypoglossal artery, diagnostic criteria. Report of a case. Acta Radiol Diagn (Stockh). 1976; 17(2): 160-166.
- Padget, DH. The circle of Willis: Its embryology and anatomy. In: Dandy, W.E., Ed., Intracranial Arterial Aneurysms, Chapter III, Comstock Publishing, New York, 67-90.
- Sepulveda W, et al. Prenatal sonography in hydranencephaly: findings during the early stages of disease. J Ultrasound Med. 2012; 31(5): 799-804.
- Quek YW, et al. Hydranencephaly associated with interruption of bilateral internal carotid arteries. Pediatr Neonatol. 2008; 49(2): 43-47.
- McAbee GN, Chan A, Erde EL. Prolonged survival with hydranencephaly: report of two patients and literature review. Pediatr Neurol. 2000. 23(1): 80-84.
- Bae, JS, Jang MU, Park SS. Prolonged survival to adulthood of an individual with hydranencephaly. Clin Neurol Neurosurg. 2008; 110(3): 307-309.
Affiliations: University of Arizona College of Medicine-Phoenix (Dr Rosette); Phoenix Children’s Hospital (Dr Richard Towbin); Cincinnati Children’s Hospital (Dr Alexander J Towbin). Disclosures: None.
