How We Do It: Peripherally Inserted Central Catheter Placement (PICC)
By Grewal S, Towbin R, Schaefer C, Aria D


Complex central venous access has been a mainstay of the pediatric interventionalist’s practice. Initially introduced in the 1970s for parenteral nutrition,1,2 silastic or polyurethane peripherally inserted central catheters (PICC) are inserted via a peripheral vein. Although the upper arm is the most common entry site, any peripheral vein may be utilized if the diameter is large enough and if the vein is in continuity with central veins and the right atrium. Ideal catheter placement is generally assisted by fluoroscopic or ultrasound guidance, or less commonly by using alternatives such as intra-atrial EKG monitoring. The decision to place a central venous catheter (CVC) or a PICC follows no standardized criteria; and is currently based on maximizing venous conservation, predicted length of time central access is needed, vessel patency, patient age and size, illnesses, as well as patient, physician or venous access nurse preference. PICCs are favored in children who are older (greater than one year) with larger peripheral veins and preferred in patients with need for 2-4 weeks of central venous access, and/or those with pulmonary disease or dysfunction. Children less than 1 year of age are also candidates for PICC insertion although alternative sites such as saphenous vein or femoral veins may be utilized3. When the femoral vein is selected, it is generally tunneled to create an entry site away from the diaper area to minimize the chance for infection. In most cases, a 3 French single-lumen or 4 French double-lumen non-tunneled PICC is inserted for children weighing less than or greater than 10 kg respectively.
INDICATIONS
The indications for PICC insertion have expanded since its introduction to a broader sphere of use. While originally predominantly used as a substitute for serial peripheral angio-catheters, PICCs are currently utilized for many of the applications of tunneled central venous catheters. Predominantly, they are used for long-term parenteral nutrition, long-term delivery of chemotherapy, prolonged antibiotic course, blood draws, fluids/electrolyte maintainence, and used for frequent blood sampling in children of all ages especially those with challenging venous access.
TECHNIQUE
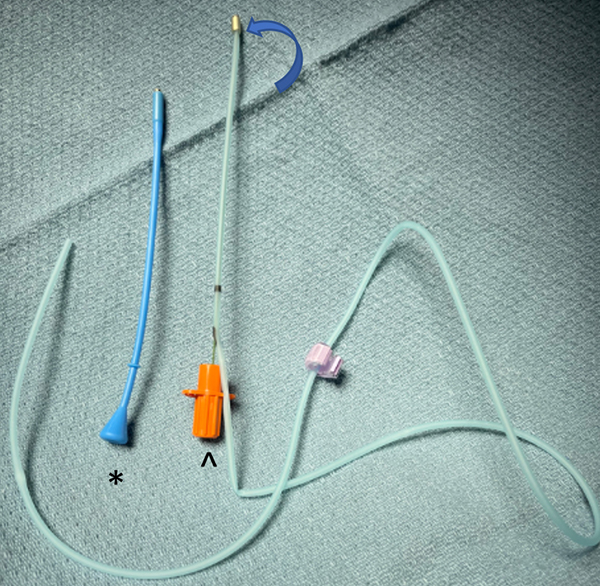
When deciding which equipment to select, the weight, age, and condition of the patient along with the preference and expertise of the proceduralist are considered for needle, catheter, and guide wire selection. For venipuncture, a sheathed needle or single wall needle are preferred with the recommendation that the bore is large enough (≥22 gauge) to allow insertion of at least an 0.018-inch guide wire, but small enough to minimize the risk of vasospasm. In very small infants, a smaller gauge needle and guide wire may be needed, while in neonates catheter size may be 2.6 French or smaller and does not easily go over a guide wire. These catheters are inserted via a peel away sheath with a stiffening wire inside the catheter.
PICC placement is commonly performed under general anesthesia in young children. Older and mature children may have PICC insertion using a combination of topical or local anesthetics alone or in combination with intravenous sedation. Children are kept NPO for six hours prior to PICC insertion if sedation is considered. Topical anesthesia with EMLA requires application approximately one hour before the procedure. However, if a J-tip is used the site may be anesthetized immediately prior to the procedure. Though infrequently needed before the procedure, tests for CBC, platelet count, PT, and PTT may be indicated in patients with suspected bleeding diathesis. Prophylactic antibiotics were found to not decrease PICC-related infections and are not routinely adminstered.1,2,4
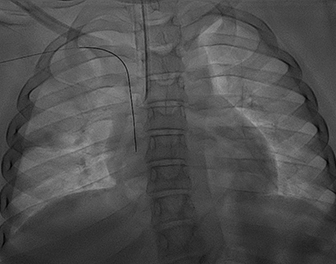
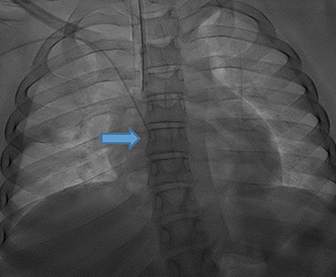
The patient is positioned supine with the upper extremity secured to an arm board at a right angle to the trunk. The venous anatomy is assessed with ultrasound and the most desirable vein is selected for access. Of the three veins in the upper arm (basilic, cephalic, and brachial) above the ante-cubital fossa, the most commonly selected vein is the basilic vein. In children who are less than 1 year of age, the cephalic vein may have a normally smaller diameter of the medial segment that can prevent central catheter positioning. Therefore, the cephalic vein is usually not our first choice in this sub-population. After the venous access site is selected, the skin of the upper arm entry site is sterilized and draped. To minimize risk of contamination, a large sterile field is prepped using sterile sheets. A 27- or 30-gauge needle is used to anesthetize the skin and subcutaneous tissue around the entry site with buffered 1% lidocaine. Real-time ultrasound guidance is used to access the venous system using Seldinger technique. After blood return is achieved, a guide wire is advanced and positioned with tip in the right atrium or inferior vena cava using fluoroscopic guidance. After insertion of the peel-away sheath, the PICC is cut to a customized length by measuring the distance from skin entry site to the distal superior vena cava approximately 1-2 vertebral bodies below the carina using a modified bent guide wire technique4 . The catheter is positioned between 1.5 and 2.0 vertebral body units below the carina (Figure 1).
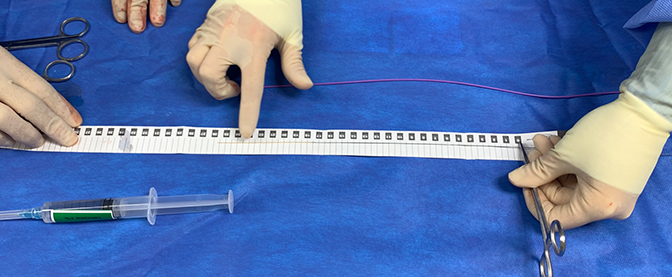
MODIFIED BENT GUIDE WIRE TECHNIQUE
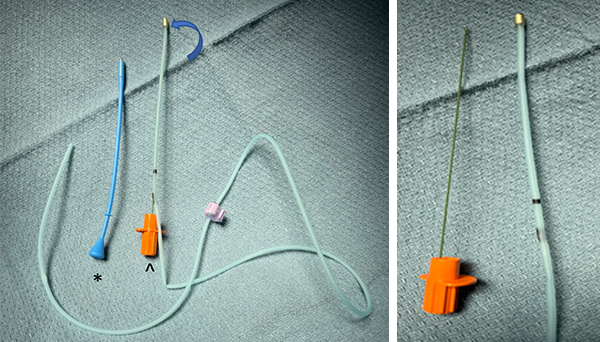
A modified bent guide wire technique is used to accurately customize catheter length immediately proximal to the cavoatrial junction. To accomplish this, the wire’s exit from the peel-away sheath is clamped with a hemostat (Figure 2A), and the wire is than removed from the sheath. The length of the external component of the sheath is subtracted from the tip of the wire and the hemostat is repositioned (Figure 2B). Once the hemostat is positioned on the wire where the catheter will exit the skin, the catheter is cut to the measured length (Figure 2C) and inserted through the peel away sheath into the venous system. A 0.018” angled glide wire traverses the PICC to direct the catheter into position using fluoroscopic guidance. Proper placement is confirmed fluoroscopically and a fluoroscopic spot film is obtained for documentation. The PICC line is secured, and the entry site is covered with gauze and an occlusive transparent dressing. Finally, the catheter is heparinized with 1.5mL of 10U/mL solution, and the final PICC length and positioning are recorded. When no longer needed, uncuffed PICCs may be removed by holding pressure at the exit site and simply pulling out the line, while cuffed PICCs may require blunt dissection of the cuff from the surrounding subcutaneous tissue ingrowth. In the latter setting, local or general anesthesia may be necessary based on the child’s ability to cooperate.
CONCLUSION
In the pediatric population the extent of PICC use and the need for central venous access is continuing to grow.5The rates of success and complication of percutaneous techniques by interventionalists are shown to be better than bedside placement.6,7. The bent guide wire techniques is useful to customize the catheter length to the size of the child and minimize the amount of catheter that needs to be secured on the skin surface which can lead to inadvertent catheter loss or malposition.
References
- Westergaard B, Classen V, Walther-Larsen S. Peripherally inserted central catheters in infants and children – indications, techniques, complications and clinical recommendations. Acta Anaesthesiologica Scandinavica. 2012; 57(3):278-287.
- Crowley JJ, Pereira JK, Harris LS, Becker CJ. Peripherally inserted central catheters: experience in 523 children. Radiology. 1997; 204(3):617-621.
- Aria D, Vatsky S, Kaye R, Schaefer C, Towbin R. Greater Saphenous Venous Access as an Alternative in Children. Pediatr Radiol. 2014 Feb;44(2):187-92. Epub 2013 Oct 6.
- Barrier A, Williams DJ, Connelly M, Creech CB. Frequency of peripherally inserted central catheter complications in children. Pediatr Infect Dis J. 2012;31(5):519–521.
- Baskin KM, Jimenez RM, Cahill AM, Jawad AF, Towbin RB. Cavoatrial junction and central venous anatomy: implications for central venous access tip position. J Vasc Interv Radiol. 2008 Mar;19(3):359-65. p
- Duszak R Jr, Bilal N, Picus D, Hughes DR, Xu BJ. Central venous access: evolving roles of radiology and other specialties nationally over two decades. Journal of the American College of Radiology. 2013; 10(8):603-612.
- Noh HM, Kaufman JA, Rhea JT, Kim SY, Geller SC, Waltman AC. Cost Comparison of Radiologic Versus Surgical Placement of Long-Term Hemodialysis Catheters. American Journal of Roentgenology. 1999; 172(3):673-675.p
Shivraj Grewal is a medical student at the University of Arizona College of Medicine Phoenix and Drs. Towbin, Schaefer, and Aria are with the Phoenix Children’s Hospital.
