Why Gadolinium Matters Today
Images
This article confers 1.0 ARRT Category A Continuing Education credit, which will be awarded upon completion of an online post test. The entire text of this supplement, learning objectives, and the posttest are available at appliedradiology.org.
Gadolinium-based contrast agents (GBCAs) were first approved for magnetic resonance imaging (MRI) in 1988 based on their ability to improve soft-tissue contrast relative to noncontrast exams.1 Since then, GBCA use has greatly expanded, and GBCAs are now used routinely in approximately 45% of MRI exams in the United States.2,3 Until recently, available general-use GBCAs consisted of the conventional-relaxivity simple linear agents Magnevist® (gadopentetate dimeglumine), Omniscan™ (gadodiamide), and OptiMARK™ (gadoversetamide); the high-relaxivity substituted linear GBCA MultiHance® (gadobenate dimeglumine), and three macrocyclic agents: ProHance® (gadoteridol), Gadavist® (gadobutrol), and Dotarem® (gadoterate meglumine).4-10 (Tables 1, 2) OptiMARK and Magnevist were removed from the market in 2018 and 2019, respectively, while GE introduced Clariscan™ (gadoterate meglumine), a generic version of Dotarem, in 2019.11
Until approximately 2006, GBCAs were deemed safe for patients, particularly those with renal impairment. Moreover, their safety profiles were considered comparable. Because substantial evidence demonstrated that higher doses provided additional diagnostic yield with few associated safety concerns, doses were frequently higher than the standard (approved) 0.1 mmol/kg dose. Double or even triple doses of some agents were routinely used for MR angiography and for specific central nervous system (CNS) applications.13,14 Today only one GBCA, ProHance, retains a triple-dose (0.3 mmol/kg) indication for MRI of the CNS in adults.8 Unfortunately, several events have occurred since 2006 that have altered the perception that all GBCAs are equally safe. These include the identification of nephrogenic systemic fibrosis (NSF) as a serious potential adverse event (AE),15 and an appreciation that gadolinium (Gd) is retained in brain, bone, and soft-tissue organs,16-19 with unknown long-term clinical consequences.
In this article, we present a summary of discussions from a recent Expert Panel Forum on Advancing Clinical Practice in MR Imaging. The primary goal of the forum was to explore the real and perceived risks associated with GBCA use and to elucidate the radiologist’s role in performing the necessary risk–benefit assessment when considering contrast-enhanced MRI for specific indications. We also address two fundamental issues: 1) when is contrast necessary, and 2) what are the best practices for its use in selected applications, specifically neuroradiology/stroke imaging, breast screening, and abdominal imaging? Finally, we discuss practical administrative and cost considerations related to contrast use in MRI.
Risks vs Benefits of GBCA Use
Although the risks associated with GBCA use can be viewed as the probability of harm, the focus should center on evaluating real risk vs perceived risk. Real risk is evidence-based and determined by the severity and likelihood of harm. GBCAs vary with respect to their structure, stability, ionicity, osmolality, and viscosity, all of which can contribute to the severity and likelihood of harm. (Table 1)
Acute Adverse Events
Based on data provided in package inserts, most AEs associated with GBCAs are mild and non-serious. Serious AEs and allergic reactions requiring hospitalization are extremely rare, occurring in about 0.008% of GBCA administrations.21 Importantly, the rates and types of AEs are comparable across agents.4-11 Although contrast extravasation is an indirect safety issue associated with GBCAs, potentially causing pain and swelling at the injection site, this can be limited with GBCAs that have lower viscosity and osmolality that enable greater ease of injection.20 (Table 1)
GBCA Stability and Dechelation
Perhaps the most clinically impactful property of GBCAs relates to their stability and potential for dechelation; ie, release of the Gd ion from the chelate structure. Macrocyclic chelates encircle the Gd ion in a molecular cage, and both in vitro and in vivo data support the greater stability of these GBCAs relative to standard relaxivity linear GBCAs, particularly relative to the nonionic linear GBCAs.16-18 Nevertheless, there was little recognition of the potential clinical consequences of dechelation until 2006, when it was shown that the combination of severe renal insufficiency/failure, exposure to higher/repeat doses of GBCAs (primarily the least stable simple linear agents), and other less understood factors could lead to NSF in some patients.15
Most unconfounded cases of NSF were associated with exposure to the standard-relaxivity simple linear GBCAs, Omniscan and Magnevist; as a result, the American College of Radiology (ACR) designated these agents, along with OptiMARK, as Group I, or high-risk, agents.21 (Table 3) These agents have since been contraindicated by the US Food and Drug Administration (FDA) for use in patients with acute kidney injury (AKI) or chronic, severe kidney disease (ie, an estimated glomerular filtration rate [eGFR] <30 mL/min/1.73 m2).4-6 Group II, or low-risk, agents include the higher-relaxivity substituted linear agent MultiHance, and the macrocyclic agents Dotarem, Gadavist, and ProHance.21
In 2017, the ACR made renal function screening (either by questioning the patient or measuring serum creatinine) optional for Group II agents in inpatients and outpatients.21 Elimination of eGFR screening without increasing risk to patients is potentially beneficial in terms of both cost and time efficiency. Conversely, if Group I agents are used, an eGFR should be obtained for inpatients, while outpatients should be asked about their history of conditions that may be associated with reduced renal function.21 Note that there is a single Group III agent, Eovist® (gadoxetate disodium), a liver-specific MR contrast agent, for which there are limited data regarding NSF risk, but for which few, if any, unconfounded cases of NSF have been reported.21 Changes in clinical practice such as screening high-risk patients for renal dysfunction, use of the lowest effective contrast dose, and use of a Group II GBCA appears to have eliminated NSF risk in patients referred for contrast-enhanced MRI.
A second change with regard to the perceived safety profile of linear vs macrocyclic GBCAs occurred in 2014 with a publication that demonstrated increased signal in the dentate nucleus and globus pallidus on noncontrast T1 MRI scans in patients with a history of having received gadolinium-based contrast.19 Although this initial study investigated only patients who received Magnevist or Omniscan, subsequent studies found that T1 hypersignal on noncontrast T1 MR images occurred more frequently with linear GBCAs than with macrocyclic agents. This caused many to speculate that, as with NSF, the linear GBCAs dechelate more readily, leading to long-term Gd retention in the brain and body.23-29 Gd retention has since been identified even after exposure to low GBCA doses in patients with normal renal function,30-31 and in the presence of an intact blood-brain barrier.32 This indicates that Gd retention likely occurs to a greater or lesser extent in all patients who receive a GBCA. Among macrocyclic GBCAs, visible hypersignal has been seen so far only after multiple injections of Gadavist and Dotarem.33-39 Among linear GBCAs, greater Gd retention has been observed after Omniscan than after Magnevist, MultiHance, or Eovist.22,29,31,32,40-43 Notably, knowledge that Gd is retained in body tissues is not new; several studies have long shown that Gd is retained in bone and body tissues.16-18
Although frequently considered a marker for Gd retention, visible T1 hypersignal is actually a very poor indicator. Although many disease conditions unrelated to Gd can cause hyperintensity in the dentate nucleus and globus pallidus, the brain has been shown to retain Gd even in the absence of visible hyperintensity or demonstrable T1 shortening. Unequivocal demonstration of Gd retention comes from tissue sampling studies using inductively coupled plasma mass spectrometry (ICP-MS). Such studies provide far superior sensitivity for quantifying Gd than studies based on analysis of MRI signal intensity.22
Using ICP-MS, Murata et al demonstrated the presence of Gd in the brain following administration of all GBCAs available in the U.S. at the time, including macrocyclic agents.29 Gd was also detected in bone at much higher levels than in the brain.29 Unfortunately, the study was performed on tissue samples from a relatively small number of human decedents (N=9) who, in some cases, passed away only days after contrast administration. Hence, further confirmatory studies are needed in a larger population. Gd retention studies are performed more easily in animals. Two recent such studies comparing Gd retention among macrocyclic agents 28 days after exposure confirmed that differences do exist, with significantly lower levels of Gd noted with ProHance than with Dotarem and Gadavist in the cerebellum, cerebrum, kidneys, liver, and skin.44,45 A third study performed in rats demonstrated Gd clearance differences among the macrocyclic agents in the first weeks and months after administration, with ProHance clearing much more rapidly than Gadavist and Dotarem.43 This might be clinically significant given that one rat year equates to roughly 30 human years, and might be of particular relevance when imaging very young patients, whose brain and cognitive function are still developing.
In May 2017, the FDA stated that although Gd retention has been observed, no adverse health effects have been identified and no restrictions on GBCA use are warranted. However, the agency cautioned that GBCA use should be limited wherever possible.46 The FDA also stated that, based on the literature, Gd retention levels appear to be greater with linear agents than with macrocyclic agents. At about the same time, a summit meeting of drug industry representatives, medical professionals, and FDA personnel met to discuss Gd retention and the possible implications and future actions.47 It was decided that new language would be added to the prescribing information for GBCAs, warning of the potential for Gd retention, particularly with linear agents, and recommending that risk minimization measures be practiced in at-risk populations. Notably, the European Medicines Agency (EMA) position differs markedly from the FDA’s, with all simple linear agents removed from the market and leaving only macrocyclic GBCAs available for general use, along with the substituted linear agents MultiHance and Primovist (Eovist) for liver imaging.48
With no unequivocal evidence of clinical sequelae from retained Gd, assessing the real risk of Gd retention is difficult. GBCAs have been approved and used routinely in clinical practice for more than 30 years, with some 450 million doses administered worldwide with little acute or long-term adverse reactions. However, until further long-term studies confirm that no adverse clinical outcomes are associated with Gd retention, careful GBCA selection and use is warranted in at-risk populations.
Serial Imaging
Care should be taken in patients requiring serial MRI examinations, particularly those with seizures or multiple sclerosis (MS), and in young women with dense breasts who require MRI for breast cancer screening or monitoring. Contrast should be used primarily in cases where it has the greatest potential to impact patient management. Moreover, macrocyclic GBCA use is considered prudent in such cases to minimize the potential risks of Gd retention.
Pediatric Patients
Most MRI examinations in children require contrast. These include workups of neoplasia, infections, and inflammatory processes, particularly at initial diagnosis, with exceptions for most congenital and/or structural disorders. The potential impact of Gd retention in pediatric patients remains unknown, as long-term data are unavailable. However, logic would dictate, and trends support, that macrocyclic agent use in children would be prudent. In this regard, animal studies have shown ProHance to be cleared more rapidly than Gadavist and Dotarem, resulting in lower levels of Gd retention in the first weeks and months.43-45 If the human situation reflects that of animals, then the first 5 weeks of rat life would correspond to approximately 3 human years. In these patients, less Gd would be retained if ProHance were used.
On the other hand, whereas all the macrocyclic agents (Dotarem, Gadavist, and ProHance) and the substituted linear agent MultiHance, are approved for use in children older than 2 years of age, only Dotarem, Gadavist, and MultiHance have a neonate indication.7-10 Among these agents, MultiHance is unique in possessing higher r1 relaxivity, meaning that greater signal is obtained at equivalent dose or equivalent signal at lower dose compared with all other GBCAs. (Table 2) MultiHance has a flexible dosing indication in neonates and infants, allowing for doses of 0.05 – 0.1 mmol/kg.7 Thus, a lower dose and, potentially, lower levels of retained Gd are possible with MultiHance.
Improving Outcomes with Contrast-Enhanced Imaging for Select Applications
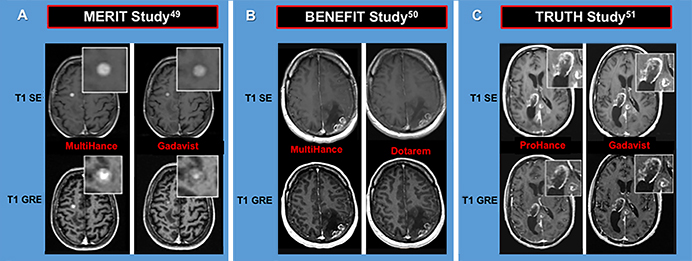
The Expert Panel Forum on Advancing Clinical Practice in MR Imaging highlighted contrast use in several applications. “Why Gadolinium Matters Today,” a presentation delivered by David Enterline, MD, provided an overview of similarities and differences among linear and macrocyclic GBCAs. A summary of select efficacy data is shown in Figure 1, along with a link to the full video presentation.
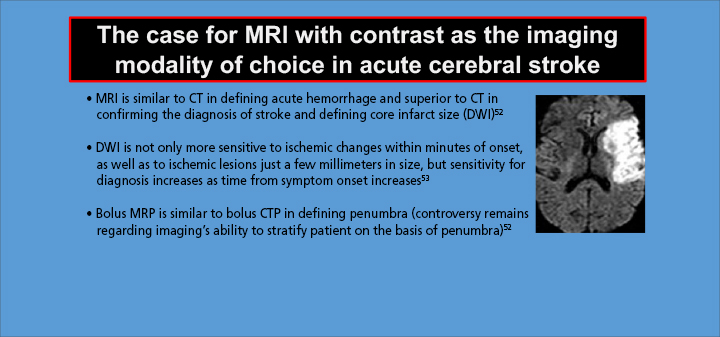
In “Contrast Enhanced MR Acute Stroke Protocol in the ED,” John Karis, MD, discussed the goals of acute stroke MR imaging, as well as some of the technical and practice considerations in imaging this condition. (See Figure 2 for the conclusions of his presentation and a link to the full video.)
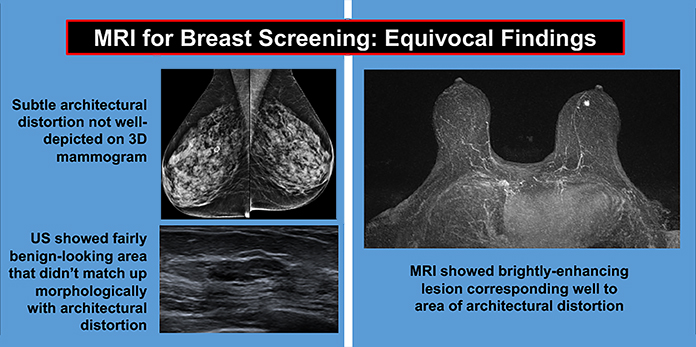
James Sancrant, DO, spoke on various aspects of breast MRI screening, including indications, performance, and protocols. Dr. Sancrant presented a case in which breast MRI was used to image a patient who underwent 3D mammogram and ultrasound. While, both modalities generated equivocal results, breast MRI clearly showed a brightly-enhancing lesion. (Figure 3) A link to the video presentation is provided in the figure legend.
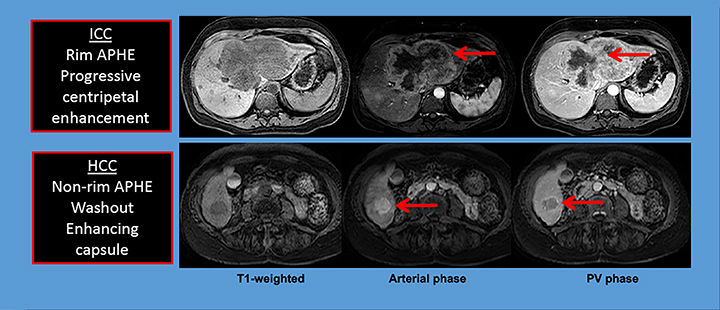
“Contrast-enhanced MR of the Abdomen and Pelvis,” by Kristin Porter, MD, PhD, outlined the ACR’s appropriateness criteria for abdominal and pelvic MR imaging and discussed a number of cases highlighting the use of contrast-enhanced MRI of the liver and urologic system, and pelvic imaging in women. Figure 4 shows an example of a hepatic application for MRI, the differentiation of mass-forming intrahepatic cholangiocarcinoma (ICC) from hepatocellular carcinoma (HCC). (See the figure legend for a link to the full video presentation.)
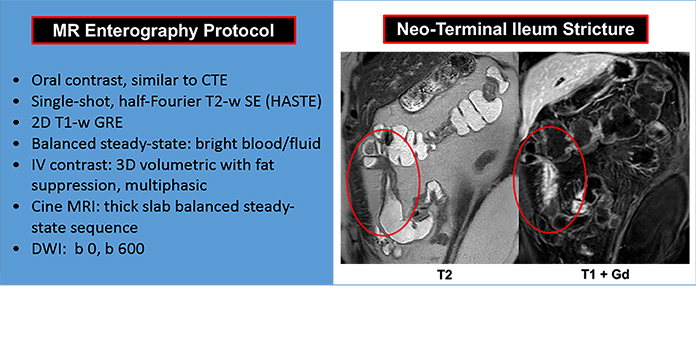
Contrast-enhanced MRI of the bowel was the focus of a presentation by Jorge Soto, MD, who reviewed indications and shared his institution’s protocols for the procedure. Dr. Soto also showed several examples of patients undergoing MRI for Crohn’s disease, rectal carcinoma, perianal fistulas, and other conditions. See Figure 5 for a summary of Dr. Soto’s findings in the follow-up of a patient with recurrent Crohn’s disease who had undergone resection of the terminal ileum.
Contrast-Enhanced MRI: Practice Considerations
Economic considerations are vital in today’s healthcare environment. Practice considerations including the selection and utilization of MR contrast can impact workflow, which in turn affects costs. For example, GBCA-enhanced imaging can increase scan time, but also potentially reduces the need for additional and/or unnecessary imaging, which may lead to overall cost savings. Decisions related to which GBCA(s) a practice uses can have economic implications: one may choose to stock several GBCAs to allow for selection of an optimal agent based on an individualized risk-benefit assessment or, alternatively, only 1 or 2 agents based on pricing or contractual constraints. In either case, an increasing number of practices are choosing to use a macrocyclic agent based on their safety profile with respect to NSF risk and Gd retention, particularly if the applications include pediatric applications and/or serial imaging.
Radiologists are not always directly involved in GBCA selection at their institution. In such cases, communication between the Radiology Department, hospital administration and/or contrast decision making committees, is important. An evidence-based case can be made by the Radiologists when macrocyclic or higher-relaxivity agents offer the possibility of improved diagnostic confidence, help to address potential medico-legal issues, or simply provide physicians and patients with greater peace of mind.
Conclusion
Contrast-enhanced MRI is fundamental to clinical practice and is faster and more efficient than many other diagnostic procedures. To perform an effective, individualized risk–benefit analysis, radiologists should be familiar with the differences in properties and associated risks among GBCAs and how these relate to agent selection for specific applications.
References
- Smith TE, Steven A, Bagert BA. Gadolinium Deposition in Neurology Clinical Practice. Ochsner J. 2019;19:17-25.
- Cass I and Saouaf R. Gadolinium-based contrast in breast MRI: What OB/GYNS need to know. Contemporary OB/GYN. 2019;64. Available at: https://www.contemporaryobgyn.net/mri/gadolinium-based-contrast-breast-mri-what-obgyns-need-know. Accessed May 9, 2020.
- Rinck PA. Magnetic Resonance in Medicine. A Critical Introduction. The Basic Textbook of the European Magnetic Resonance Forum. 12th edition, 2018|2020. BoD, Germany.
- Omniscan™ (gadodiamide) injection [prescribing information]. Princeton, NJ: GE Healthcare; August 2013.
- Magnevist® (gadopentetate dimeglumine) injection [prescribing information]. Wayne, NJ: Bayer HealthCare Pharmaceuticals; June 2014.
- OptiMARK™ (gadoversetamide) injection [prescribing information]. Bloomington, IN: Guerbet LLC; August 2016.
- MultiHance® (gadobenate dimeglumine) injection [prescribing information]. Princeton, NJ; Bracco Diagnostics Inc.; July 2013.
- ProHance® (Gadoteridol) Injection, [prescribing information]. Princeton, NJ: Bracco Diagnostics Inc.; November 2013.
- Gadavist® (gadobutrol) injection [prescribing information]. Wayne, NJ; Bayer HealthCare Pharmaceuticals; April 2016.
- Dotarem® (gadoteric acid) [prescribing information]. Bloomington, IN: Guerbet LLC; September, 2017.
- Clariscan™ (gadoterate meglumine) [prescribing information]. Marlborough, MA: GE Healthcare Inc.; November, 2019.
- Shen Y, Goerner FL, Snyder C, et al. T1 relaxivities of gadolinium-based magnetic resonance contrast agents in human whole blood at 1.5, 3, and 7 T. Invest Radiol. 2015;50:330-338.
- Filippi M, Campi A, Martinelli V, et al. Comparison of triple dose versus standard dose gadolinium-DTPA for detection of MRI enhancing lesions in patients with primary progressive multiple sclerosis. J Neurol Neurosurg Psychiatry. 1995;59:540-544.
- Essig M, Lodemann KP, Le-Huu M, et al. Intraindividual comparison of gadobenate dimeglumine and gadobutrol for cerebral magnetic resonance perfusion imaging at 1.5 T. Invest Radiol. 2006;41: 256-263.
- Thomsen HS, Marckmann P, Logager VB. Nephrogenic systemic fibrosis (NSF): a late adverse reaction to some of the gadolinium based contrast agents. Cancer Imaging. 2007;7:130-137.
- Gibby WA, Gibby KA, Gibby WA. Comparison of Gd DTPA-BMA (Omniscan) versus Gd HP-DO3A (ProHance) retention in human bone tissue by inductively coupled plasma atomic emission spectroscopy. Invest Radiol. 2004 Mar;39:138-142.
- Tweedle MF, Wedeking P, Kumar K. Biodistribution of radiolabeled, formulated gadopentetate, gadoteridol, gadoterate, and gadodiamide in mice and rats. Invest Radiol. 1995;30:372-380.
- White GW, Gibby WA, Tweedle MF. Comparison of Gd(DTPA-BMA) (Omniscan) versus Gd(HP-DO3A) (ProHance) relative to gadolinium retention in human bone tissue by inductively coupled plasma mass spectroscopy. Invest Radiol. 2006;41:272-278.
- Kanda T, Ishii K, Kawaguchi H, et al. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology. 2014;270:834–841.
- Tweedle MF. The ProHance story: the making of a novel MRI contrast agent. Eur Radiol. 1997;7 Suppl 5:225-230.
- American College of Radiology (ACR) Committee on Drugs and Contrast Media. ACR Manual on Contrast Media, 2020. Available at: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf. Accessed June 5, 2020.
- McDonald RJ, Levine D, Weinreb J, et al. Gadolinium Retention: A Research Roadmap from the 2018 NIH/ACR/RSNA Workshop on Gadolinium Chelates. Radiology. 2018;289:517-534.
- Errante Y, Cirimele V, Mallio CA, Di Lazzaro V, Zobel BB, Quattrocchi CC. Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Invest Radiol. 2014;49:685-690.
- Radbruch A, Weberling LD, Kieslich PJ, et al Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology. 2015;275:783-791.
- Radbruch A, Weberling LD, Kieslich PJ, et al High-signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted images: evaluation of the macrocyclic gadolinium-based contrast agent gadobutrol. Invest Radiol. 2015;50:805-810.
- Quattrocchi CC, Mallio CA, Errante Y, Beomonte Zobel B. High T1 signal intensity in dentate nucleus after multiple injections of linear gadolinium chelates. Radiology. 2015;276:616-617.
- Quattrocchi CC, Mallio CA, Errante Y, et al Gadodiamide and dentate nucleus T1 hyperintensity in patients with meningioma evaluated by multiple follow-up contrast-enhanced magnetic resonance examinations with no systemic interval therapy. Invest Radiol. 2015;50:470-472.
- 28. Weberling LD, Kieslich PJ, Kickingereder P, et al Increased signal intensity in the dentate nucleus on unenhanced T1-weighted images after gadobenate dimeglumine administration. Invest Radiol. 2015;50:743-748.
- Murata N, Gonzalez-Cuyar LF, Murata K, et al Macrocyclic and other non-group 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Invest Radiol. 2016;51:447-453.
- Barbieri S, Schroeder C, Froehlich JM, Pasch A, Thoeny HC. High signal intensity in dentate nucleus and globus pallidus on unenhanced T1-weighted MR images in three patients with impaired renal function and vascular calcification. Contrast Media Mol Imaging. 2016;11:245-250.
- Ramalho J, Castillo M, AlObaidy M, et al High signal intensity in globus pallidus and dentate nucleus on unenhanced T1-weighted MR images: evaluation of two linear gadolinium-based contrast agents. Radiology. 2015;276:836-844.
- McDonald RJ, McDonald JS, Kallmes DF, et al Gadolinium Deposition in Human Brain Tissues after Contrast-enhanced MR Imaging in Adult Patients without Intracranial Abnormalities. Radiology. 2017:161595.
- Bjørnerud A, Vatnehol SAS, Larsson C, Due-Tønnessen P, Hol PK, Groote IR. Signal enhancement of the dentate nucleus at unenhanced MR imaging after very high cumulative doses of the macrocyclic gadolinium-based contrast agent gadobutrol: An observational study. Radiology. 2017;Sep 8:170391.
- Splendiani A, Corridore A, Torlone S, et al. Visible T1-hyperintensity of the dentate nucleus after multiple administrations of macrocyclic gadolinium-based contrast agents: yes or no? Insights Imaging. 2019;10:82.
- Splendiani A, Perri M, Marsecano C, et al. Effects of serial macrocyclic based contrast materials gadoterate meglumine and gadobutrol administrations on gadolinium-related dentate nuclei signal increases in unenhanced T1-weighted brain: a retrospective study in 158 multiple sclerosis (MS) patients. Radiol Med. 2018;123:125-134.
- Stojanov DA, Aracki-Trenkic A, Vojinovic S, Benedeto-Stojanov D, Ljubisavljevic S. Increasing signal intensity within the dentate nucleus and globus pallidus on unenhanced T1W magnetic resonance images in patients with relapsing-remitting multiple sclerosis: correlation with cumulative dose of a macrocyclic gadolinium-based contrast agent, gadobutrol. Eur Radiol. 2016;26:807-815.
- Rossi Espagnet MC, Bernardi B, Pasquini L, Figà-Talamanca L, Tomà P, Napolitano A. Signal intensity at unenhanced T1-weighted magnetic resonance in the globus pallidus and dentate nucleus after serial administrations of a macrocyclic gadolinium-based contrast agent in children. Pediatr Radiol. 2017;47:1345-1352.
- Kelemen P, Alaoui J, Sieron D, et al. T1-weighted grey matter signal intensity alterations after multiple administrations of gadobutrol in patients with multiple sclerosis, referenced to white matter. Sci Rep. 2018;8:16844.
- Moreno J, Vaz NB, Soler JC, et al. High signal intensity in the dentate nucleus on unenhanced T1-weighted MR images in melanoma patients receiving macrocyclic gadolinium-based contrast. J Radiol Diagn Methods. 2018;1:101-107.
- Food and Drug Administration (FDA) Website. Medication Guides. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=medguide.page. Accessed July 9, 2020.
- Robert P, Violas X, Grand S et al (2016) Linear gadolinium-based contrast agents are associated with brain gadolinium retention in healthy rats. Invest Radiol. 51:73-82.
- 42. Lohrke J, Frisk AL, Frenzel T et al (2017) Histology and gadolinium distribution in the rodent brain after the administration of cumulative high doses of linear and macrocyclic gadolinium-based contrast agents. Invest Radiol. 52:324-333.
- Jost G, Frenzel T, Boyken J, Lohrke J, Nischwitz V, Pietsch H. Long-term Excretion of Gadolinium-based Contrast Agents: Linear versus Macrocyclic Agents in an Experimental Rat Model. Radiology. 2019;290:340-348.
- Bussi S, Coppo A, Botteron C et al (2018) Differences in gadolinium retention after repeated injections of macrocyclic MR contrast agents to rats. J Magn Reson Imaging. 47:746–752
- Bussi S, Coppo A, Celeste R, et al. Macrocyclic MR contrast agents: evaluation of multiple-organ gadolinium retention in healthy rats. Insights Imaging. 2020;11:11.
- Food and Drug Administration (FDA) Website. FDA Drug Safety Communication: FDA identifies no harmful effects to date with brain retention of gadolinium-based contrast agents for MRIs; review to continue. May 22, 2017. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-identifies-no-harmful-effects-date-brain-retention-gadolinium. Accessed May 9, 2020.
- Gadolinium Toxicity Website. FDA Advisory Committee votes to revise warnings for all gadolinium-based contrast agents. September 8, 2017. Available at: https://gadoliniumtoxicity.com/2017/09/17/fda-advisory-cmte-votes-to-revise-warnings-for-gbcas/. Accessed May 9, 2020.
- European Medicines Agency (EMA) Website. PRAC confirms restrictions on the use of linear gadolinium agents. July 7, 2017. Available at: https://www.ema.europa.eu/en/documents/referral/gadolinium-article-31-referral-prac-confirms-restrictions-use-linear-gadolinium-agents_en.pdf. Accessed May 9, 2020.
- Seidl Z, Vymazal J, Mechl M, et al. Does Higher Gadolinium Concentration Play a Role in the Morphologic Assessment of Brain Tumors? Results of a Multicenter Intraindividual Crossover Comparison of Gadobutrol Versus Gadobenate Dimeglumine (The MERIT Study). Am J Neuroradiol. 2012;33:1050-1058.
- Vaneckova M, Herman M, Smith MP, et al. The Benefits of High Relaxivity for Brain Tumor Imaging: Results of a Multicenter Intraindividual Crossover Comparison of Gadobenate Dimeglumine with Gadoterate Meglumine (The BENEFIT Study). Am J Neuroradiol. 2015;36:1589-1598.
- Maravilla KR, Smith MP, Vymazal J, et al. Are there differences between macrocyclic gadolinium contrast agents for brain tumor imaging? Results of a multicenter intraindividual crossover comparison of gadobutrol with gadoteridol (the TRUTH study). Am J Neuroradiol. 2015;36:14-23.
- Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293-298.
- Sanelli PC, Sykes JB, Ford AL, Lee JM, Vo KD, Hallam DK. Imaging and treatment of patients with acute stroke: an evidence-based review. Am J Neuroradiol. 2014; 35:1045-1051.
Citation
D E, J K, M M, KK P, J S, JA S. Why Gadolinium Matters Today. Appl Radiol. 2021;(1):supplement.
January 19, 2021