Ureteral Obturator Hernia
Images
Case Summary
An elderly patient with a remote history of renal transplantation presented with several days of dysuria, malaise, and nausea. The patient was also tachycardic with suprapubic tenderness and laboratory evaluation revealed creatinine elevation.
Imaging Findings
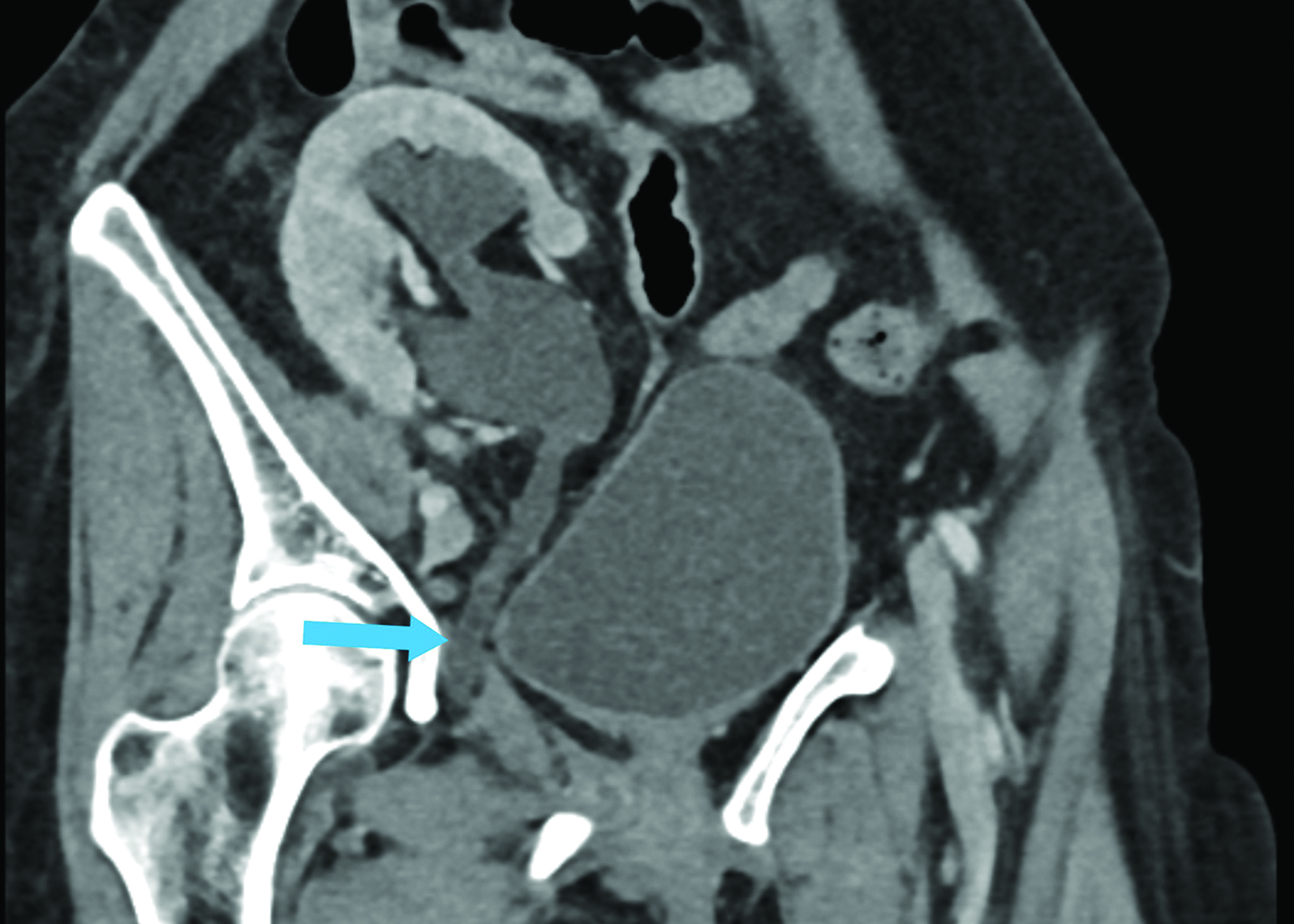
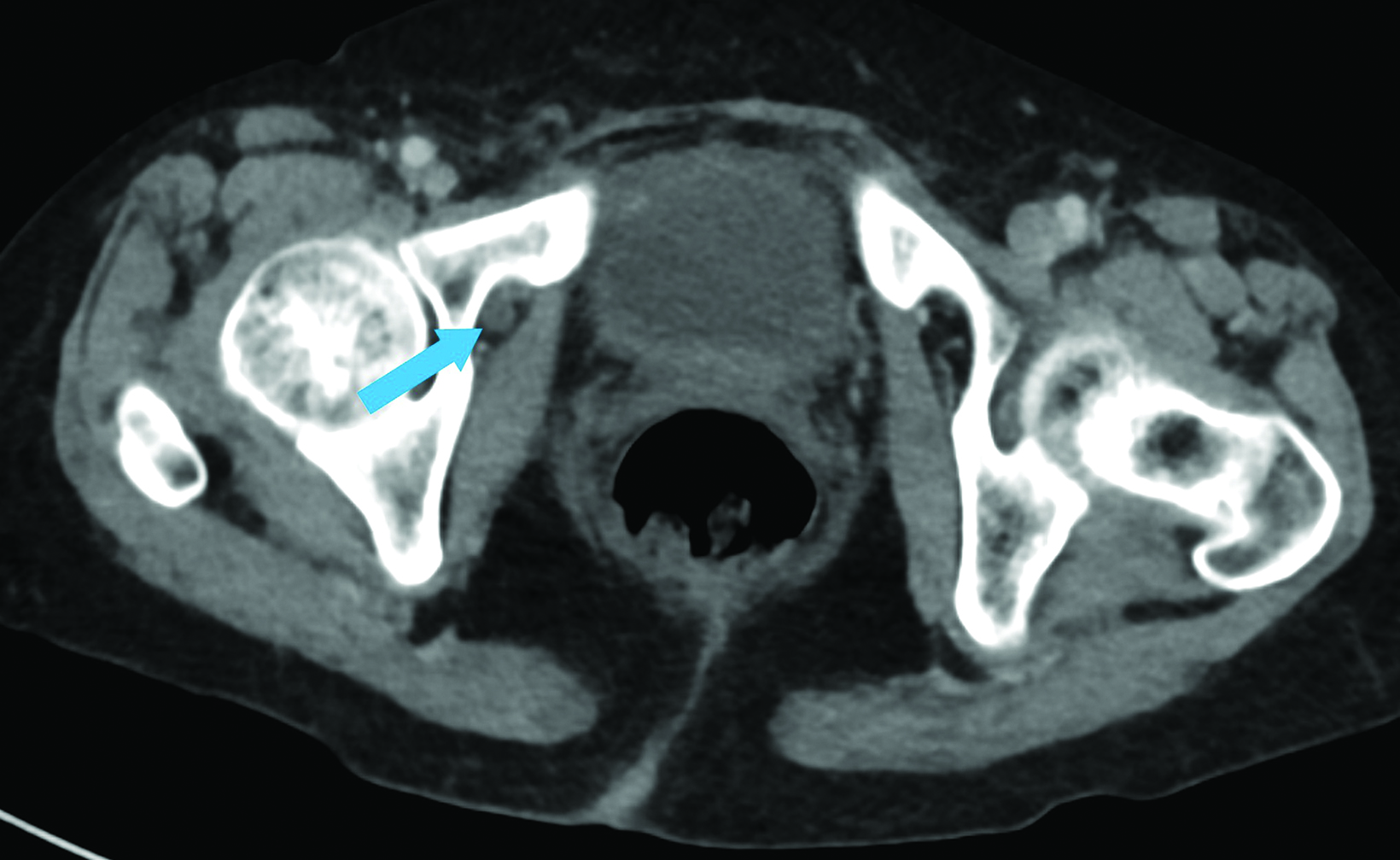
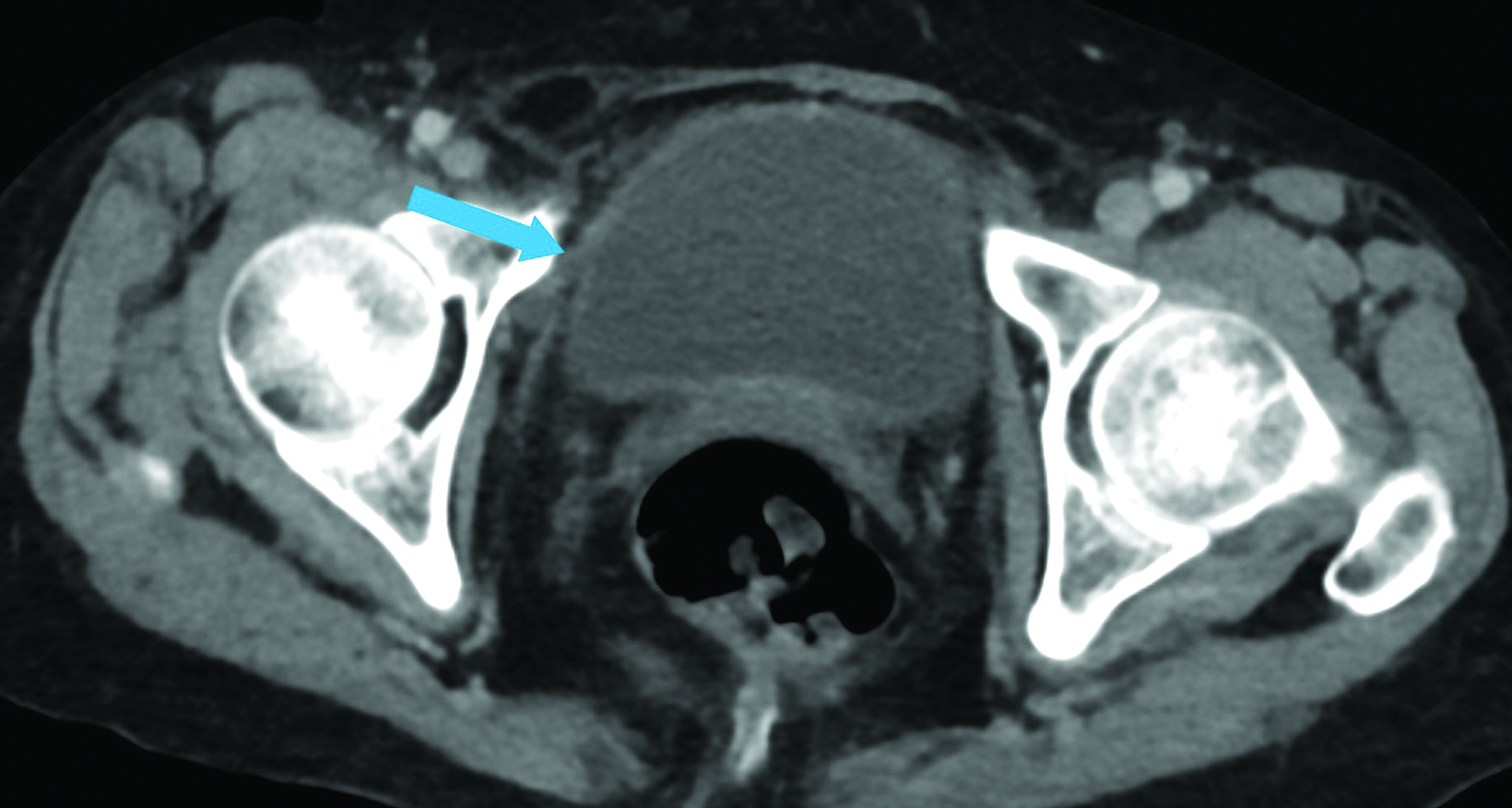
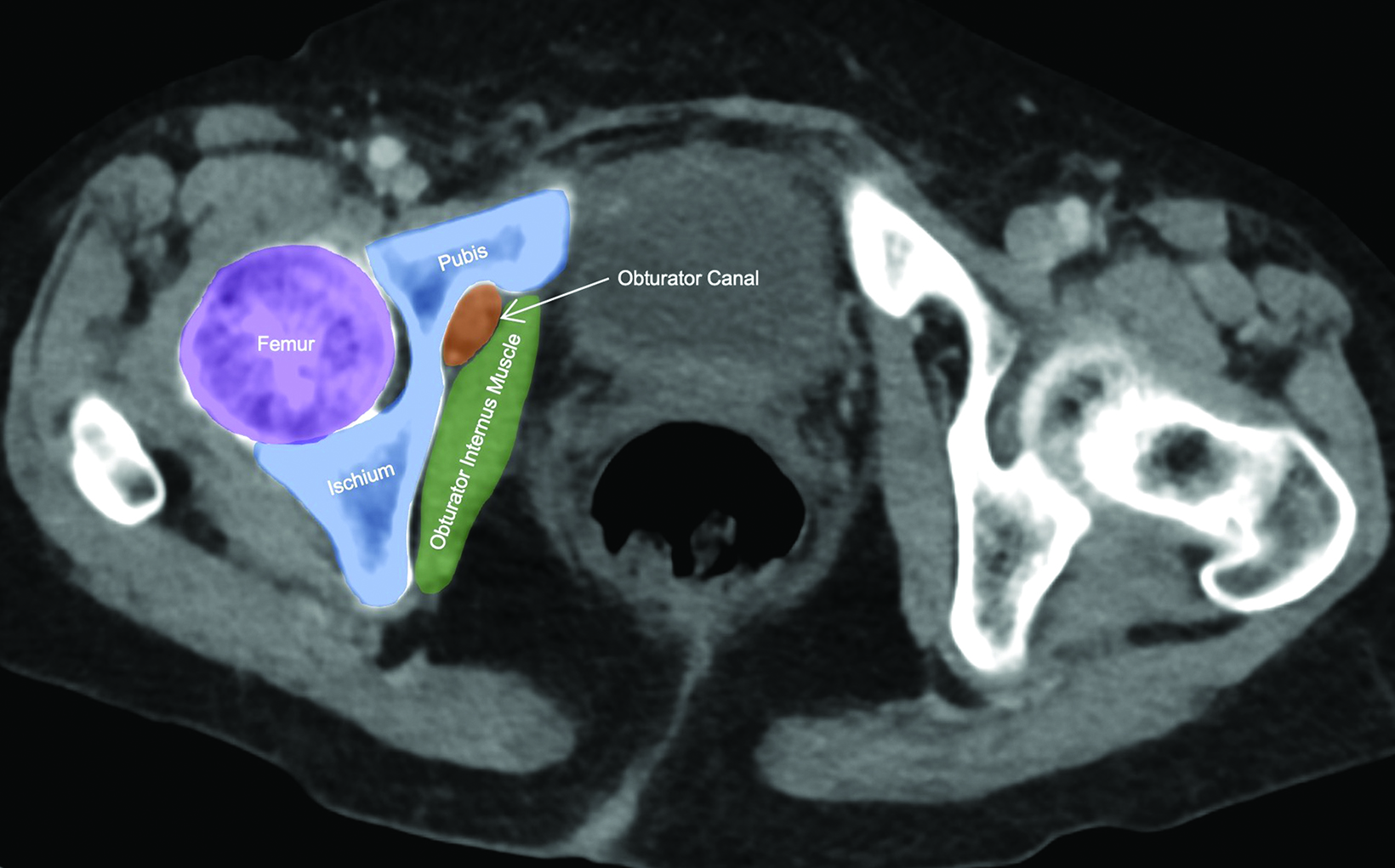
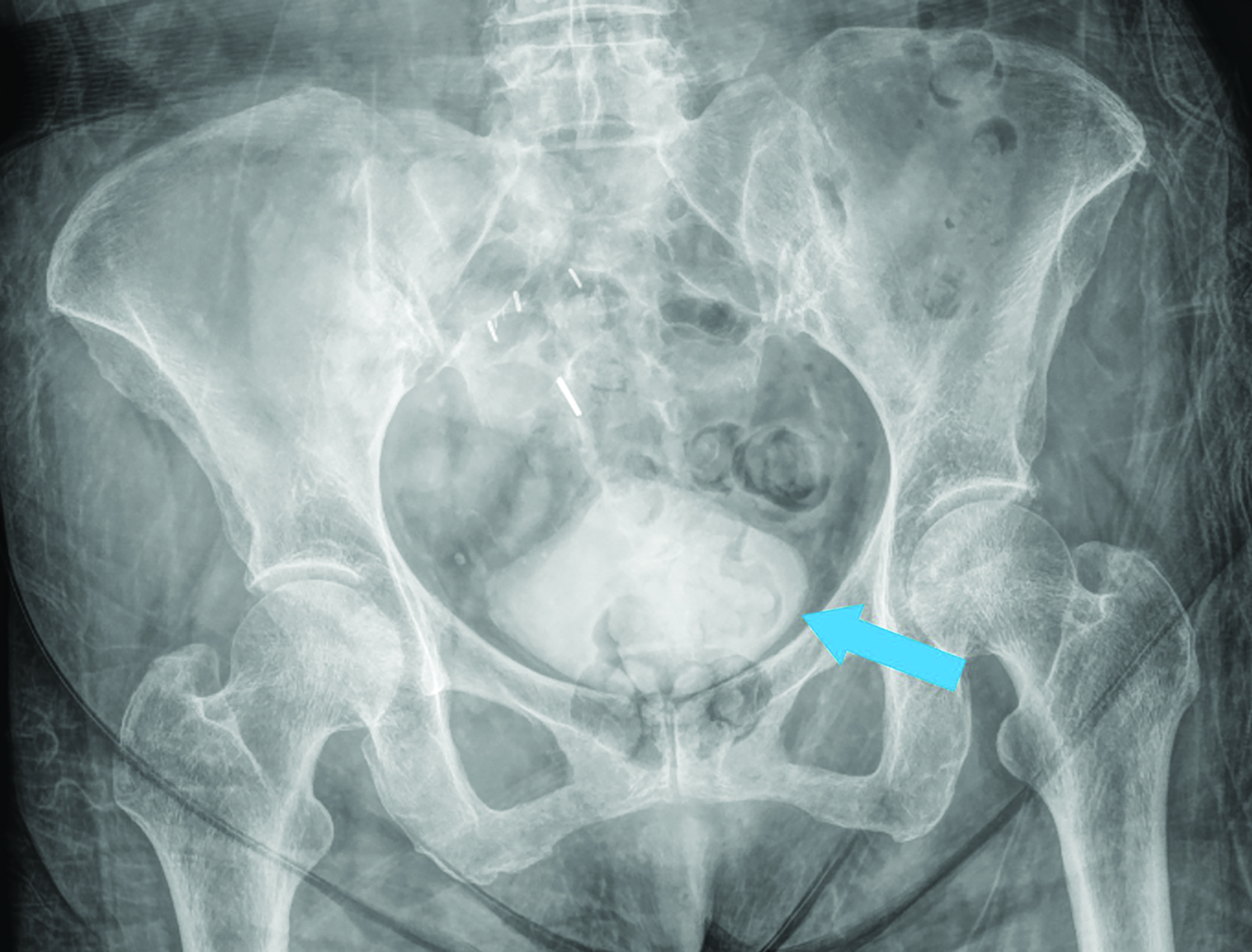
Abdominal contrast-enhanced CT (Figures 1,2) demonstrated hydroureteronephrosis of the transplant kidney in the right iliac fossa and distal herniation of the ureter into the right obturator canal. Follow-up radiography demonstrated contrast opacifying the bladder (Figure 3), indicating delayed passage of urine into the bladder. The patient’s renal function returned to baseline with fluid resuscitation, and they did not require immediate intervention for obstructive uropathy.
Diagnosis
Ureteral obturator hernia
Discussion
Ureteral hernia is a rare condition most commonly found incidentally on imaging or during surgical procedures.1 Ureteral herniation can occur in a number of anatomic locations, including the inguinal canal, femoral ring, sciatic foramen, obturator foramen, and diaphragm.2 Among these, obturator herniation is exceptionally rare, with only three cases having been reported in the literature.3–5
There are several important characteristics of ureteral obturator hernias (UOHs). First, they are a rare type of abdominal wall hernia that is nine times more common in women than in men.6 This may be due in part to their wider pelvis, more triangular obturator canal opening, and larger transverse diameter. Other factors that increase the risk of UOH are related to progressive relaxation of the pelvic floor, which is associated with advanced age, emaciation, increased intrabdominal pressure, and multiparity.7 Loss of preperitoneal fat and lymphatic tissue over the obturator canal with aging and/or malnutrition also increases the space around the vessels and nerves, thus predisposing to herniation. Diagnosis is difficult as symptoms are often nonspecific, and palpable masses or associated pain are often not present at physical exam.4 Therefore, UOHs are often found incidentally on imaging or during surgery for intestinal obstruction or peritonitis.7
There are several additional factors to consider. First, UOHs are considerably more rare than are hernias involving the bowel. They often present with nonspecific urinary symptoms such as dysuria, abdominal pain, nausea, and vomiting.3 As in our case, renal transplant is associated with increased risk of ureteral herniation, particularly as time from transplant increases.5,8 This may be due to redundancy of the transplant ureter or the anterior and inferior location of many transplanted kidneys.9
The main complication of UOH is ureteral obstruction, which can lead to hydronephrosis and, potentially, kidney damage and/ or infection. Previous cases of UOH with ureteral obstruction and worsening kidney function have required urgent nephrostomy and/or surgical hernia repair.3–5 However, in our case, follow-up imaging demonstrated contrast passage into the bladder, indicating urine excretion. Along with the patient’s decreasing creatinine, this reduced the concern for major obstruction and renal damage. Therefore, urgent intervention was not required. However, the patient was scheduled for a nonurgent surgical evaluation for potential ureteral obturator hernia repair.
Because its symptoms overlap with other conditions, UOH often is not diagnosed until surgery. However, imaging can visualize the hernia and sequelae such as hydroureteronephrosis from obstruction. In cases where imaging is indeterminate, delayed-phase CT with contrast excretion from the renal transplant may help to better delineate the course of the ureter.
Conclusion
We present a rare case of a ureteral obturator hernia. This entity occurs almost exclusively in elderly women and is often accompanied by nonspecific urinary and/or abdominal symptoms. Ureteral obturator hernias may be associated with prior renal transplants. Owing to the ambiguity of symptoms, imaging plays an important role in diagnosing the condition and evaluating for ureteral obstruction, which may necessitate urgent diversion with nephrostomy and/or surgical hernia repair.
References
Citation
BH L, S L, P S, L N. Ureteral Obturator Hernia. Appl Radiol. 2023;(6):43-45.
November 3, 2023