Understanding Patient Barriers to Utilization of Low-dose CT Lung Cancer Screening in a High-risk Population
Images
Abstract
Objective and Hypothesis: The purpose of this study was to assess factors that may affect low-dose CT (LDCT) utilization for lung cancer screening in a diverse population. The authors hypothesized that a lack of medical provider support may contribute to underutilization of LDCT for lung cancer screening.
Methods and Materials: A 22-question survey tool was developed and distributed to patients in the radiology department waiting room of a large, urban academic institution over a four-week period. The questionnaire assessed demographics, smoking history, knowledge about LDCT, and potential barriers to getting screened. Data are reported and frequencies.
Results: A total of 124 patients responded to the questionnaire. 50% were current or former smokers. 94% of respondents saw their primary care provider within the past year, although 89% said they had not heard about LDCT from their doctors. 90% knew that that smoking is the most common cause of lung cancer, although only 64% knew that lung cancer can be treated successfully at least “sometimes.” 85% reported to be at least somewhat concerned that they or someone they know could die of lung cancer, and 86% were willing to visit their provider to learn more about lung cancer screening. Cost and conflict with work schedules were the most frequently reported reasons for nonadherence to medical appointments.
Conclusions: These data identified an information and communication gap related to lung cancer screening with LDCT, especially in a high-risk population. These results support the need to better understand factors contributing to this gap and to reduce barriers to communication and access.
Keywords: lung cancer; cancer screening; low-dose CT; health disparities; patient centered care
Introduction
Lung cancer is the second-most common cancer and the leading cause of cancer-related deaths in the United States.1 Cigarette smoking is the number one risk factor for lung cancer, linked to about 80-90% of lung cancers in the United States.1 Like most cancers, the stage of diagnosis strongly influences length of survival, with a five-year relative survival of 60% for localized disease, 30% for regional disease, and 6% for metastatic disease.1 Over 50% of cases continue to be diagnosed at the metastatic stage.2 Although advances in healthcare and disease prevention have led to improved lung cancer outcomes, racial and socioeconomic disparities persist.1,3,4 Black Americans who smoke have a higher incidence of lung cancer, advanced disease on diagnosis, and mortality even when their cancer is diagnosed at the same stage as White individuals.5,6
Low-dose CT (LDCT) has become the preferred method of lung cancer screening, although adoption remains inconsistent, with several disparities in the community setting.6 The landmark National Lung Screening Trial (NLST) demonstrated a 20% reduction in mortality among high-risk patients when utilizing LDCT instead of chest X-rays for screening, which has been attributed to disease detection at an earlier, more localized stage.3
The U.S. Preventive Services Task Force (USPSTF) updated its recommendations in 2021, which increased the number of people eligible for LDCT screening to include those 50-80 years old with a 20 pack-year history and who currently smoke or have quit within the past 15 years.7,8 The need to screen high-risk individuals has also been recognized by numerous medical societies, and LDCT lung cancer screening is covered by Medicare, although variability exists for Medicaid coverage across states.8-12
Unfortunately, screening prevalence has been lagging and heterogeneous, with recent studies showing that only 5-20% of eligible individuals receive LDCT screening, with ongoing concerns about inequities across racial and ethnic groups.4,13-18
Furthermore, limited data exist on the impact of lung cancer screening in racial and ethnic minority populations despite their higher disease burden.6,11,19 There is also concern that the NLST results may not be generalizable to all populations, as 91% of the participants were White, and efforts to introduce racial and ethnic diversity into the NLST have had limited success .18,20-22
Based on these unmet needs and health disparities, more data on community perceptions and barriers to LDCT screening are needed, especially among diverse populations. Identification of barriers and system failures can help guide the development of interventions. We hypothesized that a lack of medical provider support plays a role in underutilization of LDCT for lung cancer screening. Thus, the purpose of this study was to assess for factors that may affect LDCT utilization for lung cancer screening in an urban population that is already connected with a healthcare system.
Methods and Materials
The authors developed a questionnaire based on background research on disparities in lung cancer screening. Questions were designed to obtain data and elicit potential barriers to lung cancer screening with LDCT. The survey (available online at appliedradiology.com) comprised 22 questions:
- 5 on patient demographics;
- 2 on access and utilization of healthcare;
- 3 on smoking history;
- 1 on concern about lung cancer;
- 2 on knowledge about lung cancer;
- 1 on willingness to learn more about lung cancer screening;
- 1 on whether LDCT had been mentioned by a healthcare provider;
- 6 on awareness of and knowledge of LDCT lung cancer screening; and
- 1 on reasons for non-adhering to appointments.
Question formats included rating scale, dichotomous, and multiple-choice. Institutional review board approval was obtained prior to study initiation, and all participants consented to participate.
This study focused on barriers to obtaining lung cancer screening in patients who already had access to healthcare. Thus, participants were recruited from the waiting room of a radiology department in a large, urban academic institution over a four-week period. A designated research assistant distributed questionnaires to patients after they registered for their radiology diagnostic imaging or procedure. Participants were given the option to either return the questionnaire upon completion prior to leaving the registration area or to complete the questionnaire with the research assistant. A total of 124 questionnaires were collected.
Data are summarized as frequencies. The knowledge score about the lung cancer screening process was calculated on a scale of 0 to 5 based on correct answers, with a higher score indicating higher knowledge. Tabulation and analysis were performed using Stata SE 14.2 (StataCorp, College Station, TX).
Results
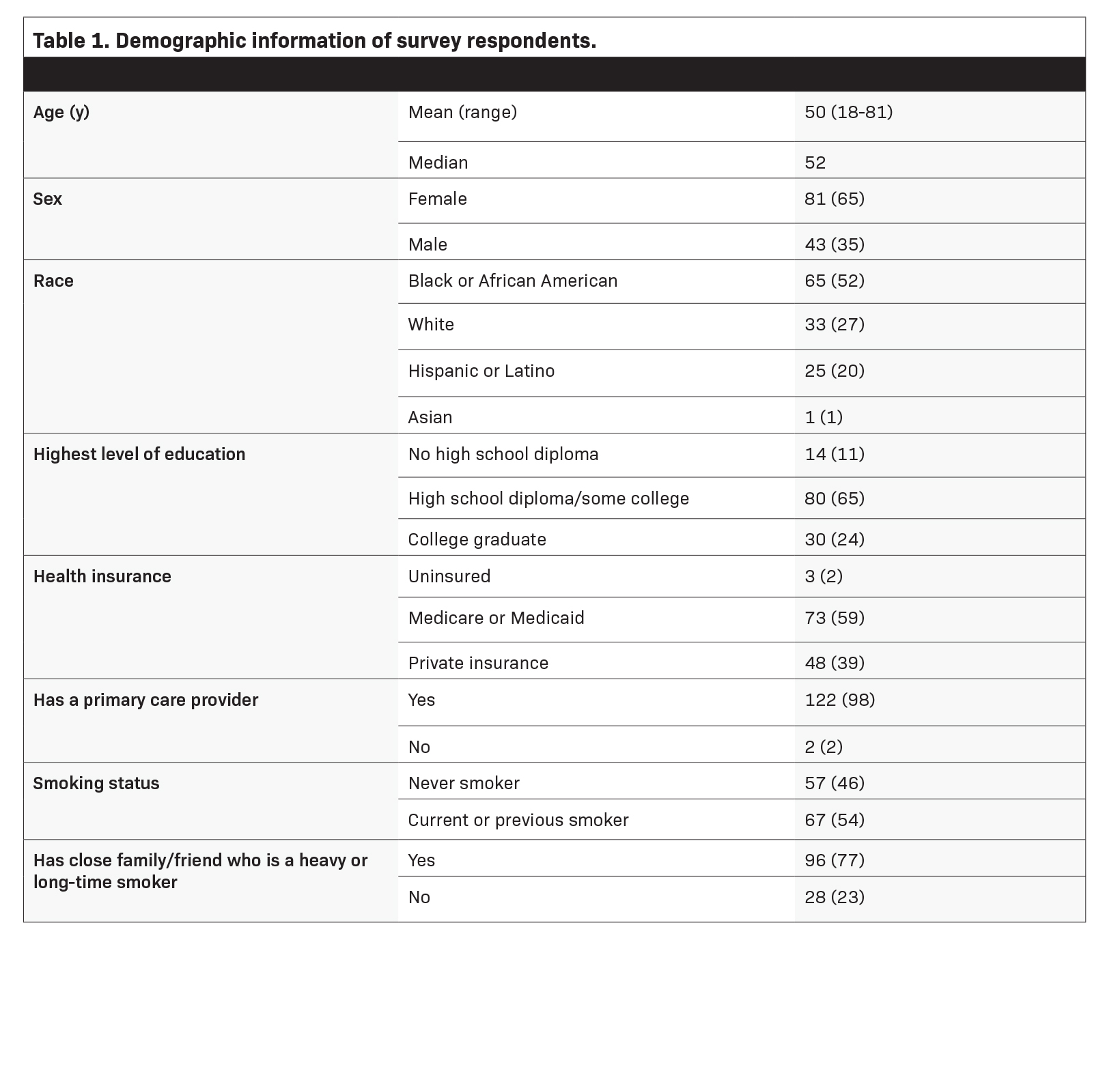
Table 1 presents the demographic information of respondents. 52% identified as Black/African American, and 59% had Medicare or Medicaid for insurance. 98% of respondents reported having a primary care provider; 94% reported visiting their provider within the past year. 54% of respondents were current or former smokers, and 77% had friends and/or family members who were heavy/long-time smokers.
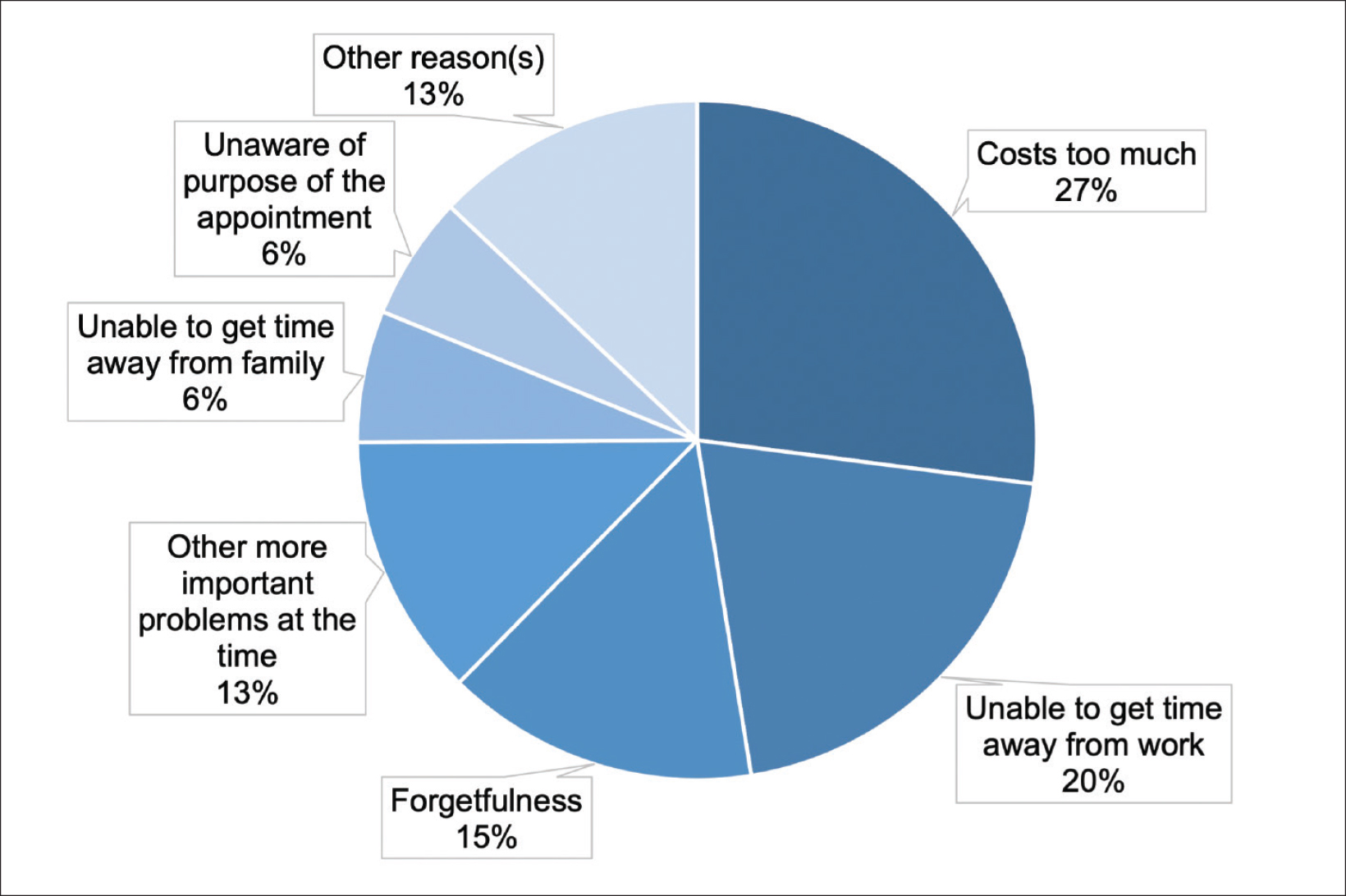
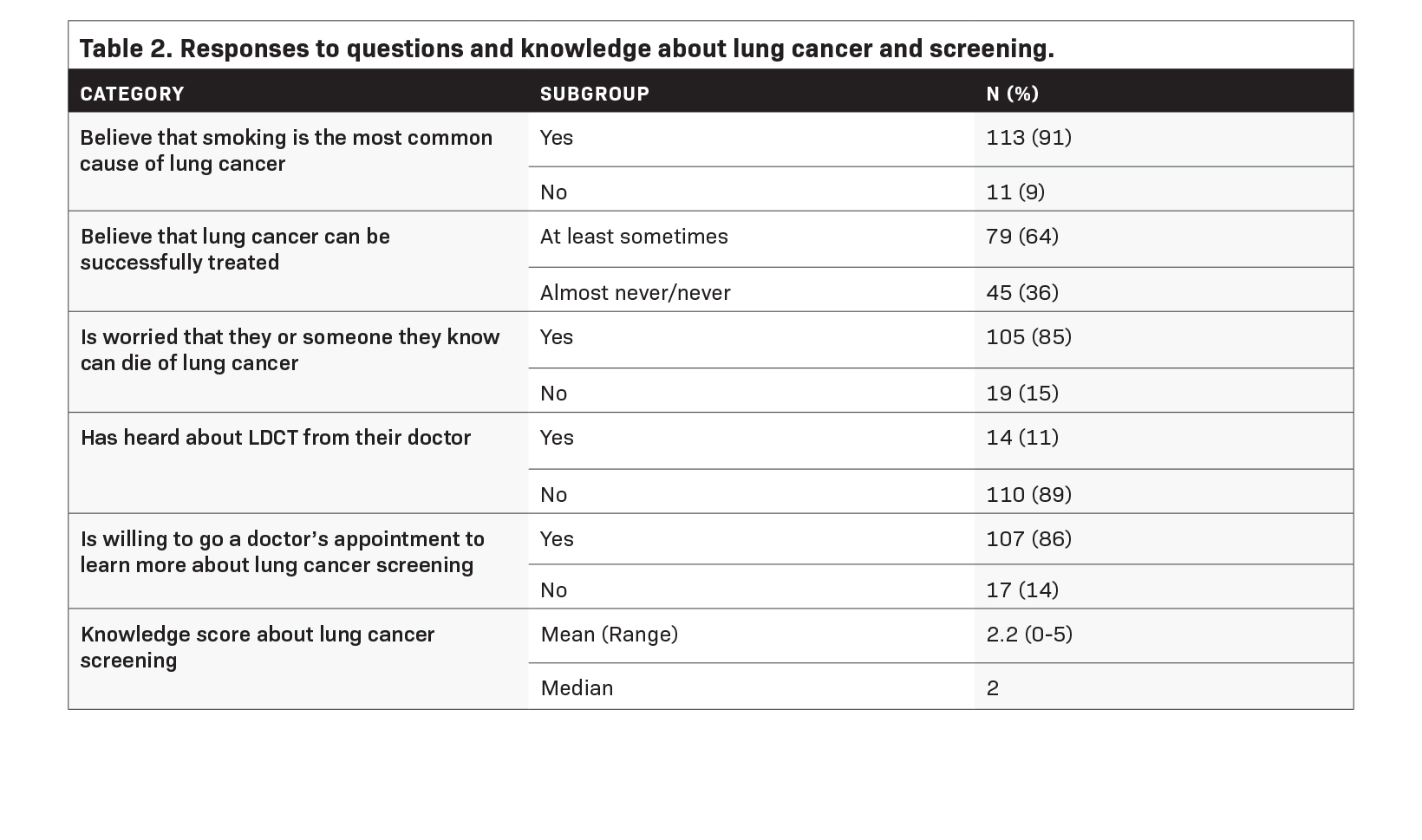
Table 2 presents data on perspectives and knowledge about lung cancer and screening. 91% of respondents agreed that smoking is the most common cause of lung cancer, although only 64% thought that lung cancer can be treated successfully at least “sometimes.” 85% of respondents reported being at least somewhat concerned that they or someone they know can die of lung cancer. 89% of respondents said they had not heard about LDCT lung cancer screening from their doctors, although 86% reported a willingness to visit a doctor to learn more about screening. The mean score on items assessing knowledge about lung cancer screening was 2/6 (33%). Figure 1 presents the breakdown of reasons that respondents thought contributed to their inability to attend scheduled medical appointments. Overall, 56% and 43% of respondents cited cost and inability to get out of work, respectively, as the most likely reasons.
Discussion
Low-dose CT for lung cancer screening has been shown to be at least as efficacious and cost effective as screening programs for breast and colon cancer.21 However, recruitment of racial and ethnic minority patients at high risk of developing lung cancer requires time, effort, and infrastructure support.22,23 Among the range of hurdles to introducing lung cancer screening into a community of diverse backgrounds, the authors specifically aimed to evaluate barriers that could be alleviated by changes made among hospitals and healthcare providers. For example, previous studies have demonstrated that Black individuals often live in more racially segregated communities compared to their White counterparts, which is associated with a later stage of diagnosis and lower cancer-specific survival.24
Therefore, the study population comprised patients at an urban institution in a Black-predominant community with the assumption that these patients were more likely to have insurance and connection to the healthcare system; thus, it was projected these patients would have a greater ability to access medical care, including appropriate screening exams.
These data demonstrated that respondents were relatively well informed about the link between smoking and the risk of developing lung cancer and were concerned about the associated morbidities. However, most respondents lacked fundamental knowledge about lung cancer screening and treatment opportunities, as approximately one-third did not believe that lung cancer was treatable. Patients may thus be unaware of the opportunity and importance of screening if their physicians are not appropriately assessing for or recommending it.
Nevertheless, most respondents indicated a willingness to visit a provider for more information, highlighting the importance of the doctor-patient relationship. Understanding the barriers for this communication gap and interventions facilitating provider communication with patients about lung cancer screening could help support patient adherence to such screening, especially since primary care physicians may be less familiar with the USPSTF recommendations.17,25-27 For example, the American Academy of Family Physicians has previously stated that evidence is insufficient to recommend for or against lung cancer screening with LDCT, and their recommendation to follow the USPSTF guidelines was not updated until March of 2021.28
The doctor-patient relationship has been shown to be an influential component of obtaining lung cancer and other disease-related screenings.29 Provider-level support, such as through patient navigators and development of culturally competent, shared decision-making tools, can help support the doctor-patient relationship and reduce barriers to care.5,11,27
In addition to deficient communication, respondents endorsed socioeconomic reasons for lack of adherence to appointments, especially cost and inability to take time off from work, likely related to accessibility and transportation. These findings are concordant with findings from other studies, and such barriers are of particular importance in lung cancer as it disproportionately affects patients of lower socioeconomic status who, for example, often have less access to healthcare services and may experience higher levels of distrust of their providers.5,6 Innovative interventions are needed to mitigate these barriers to screening, especially in communities that are at higher risk of death from lung cancer. Such interventions could include mobile imaging campaigns, provision of transportation benefits, expansion of telehealth consultations, and collaboration with community leaders.5,6,23
Study Limitations
Limitations of this study include the voluntary nature of the survey, convenience sampling of patients in the radiology waiting room at a single institution, and limited generalizability beyond the specific urban setting. No baseline population data were gathered, so response rate was not assessed. Nevertheless, the respondent demographics suggest a diverse cohort based on self-identified racial and educational backgrounds, which aligns with the study goals to evaluate an at-risk population. Additionally, the study assessed patients who already had access to the medical system, so these data likely overestimate knowledge and access. Appropriate access to and communication about lung cancer screening is likely even lower in the community setting.
In conclusion, this study identified a need for education of patients and providers with respect to the efficacy of early detection and treatment of lung cancer, as well as about the details of lung cancer screening. Ultimately, the success of LDCT for lung cancer screening depends on adequate awareness and patient access to the healthcare system, as well as a trusting patient-doctor relationship. Further studies are needed to better elucidate the factors contributing to disparities in LDCT lung cancer screening, with inclusion of other racial and ethnic minorities. The efficacy of interventions such as culturally appropriate educational material on LDCT, utilization of patient navigators to liaise with patients and doctors, and provision of transportation benefits to enable patients to keep medical appointments for lung cancer screening should also be evaluated.
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33.
- Cancer stat facts: Lung and bronchus cancer. National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program Web site. https://seer.cancer.gov/ statfacts/html/lungb.html. Published 2023. Accessed 1 Aug, 2023.
- Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
- Pinsky PF, Lau YK, Doubeni CA. Potential disparities by sex and race or ethnicity in lung cancer screening eligibility rates. CHEST. 2021;160(1):341-350.
- Coughlin SS, Matthews-Juarez P, Juarez PD, Melton CE, King M. Opportunities to address lung cancer disparities among African Americans. Cancer Med. 2014;3(6):1467-1476.
- Maki KG, Talluri R, Toumazis I, Shete S, Volk RJ. Impact of U.S. Preventive Services Task Force lung cancer screening update on drivers of disparities in screening eligibility. Cancer Med. 2023;12(4):4647-4654.
- Force UPST. Screening for lung cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(10):962-970.
- Pinheiro LC, Groner L, Soroka O, et al. Analysis of eligibility for lung cancer screening by race after 2021 changes to US Preventive Services Task Force screening guidelines. JAMA Netw Open. 2022;5(9):e2229741-e2229741.
- Screening for lung cancer with low dose computed tomography (LDCT). Centers for Medicare & Medicaid. https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&ncaid=304. Published 2022. Accessed 1 Aug, 2023.
- Gupta N, Halpern EJ, Rao VM. Association between Medicaid expansion status and lung cancer screening exam growth: Findings from the ACR lung cancer registry. Clin Imaging. 2021;73:79-85.
- Rivera MP, Katki HA, Tanner NT, et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society state- ment. Am J Respir Crit Care Med. 2020;202(7):e95-e112.
- Liu Y, Colditz GA, Kozower BD, et al. Association of Medicaid expansion under the Patient Protection and Affordable Care Act with non-small cell lung cancer survival. JAMA Oncol. 2020;6(8):1289-1290.
- Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States—2010 to 2015. JAMA Oncol. 2017;3(9):1278-1281.
- Fedewa SA, Kazerooni EA, Studts JL, et al. State variation in low-dose computed tomography scanning for lung cancer screening in the United States. J Natl Cancer Inst. 2020;113(8):1044-1052.
- Narayan AK, Gupta Y, Little BP, Shepard JO, Flores EJ. Lung cancer screening eligibility and use with low-dose computed tomography: Results from the 2018 Behavioral Risk Factor Surveillance System cross-sectional survey. Cancer. 2021;127(5):748-756.
- Narayan AK, Chowdhry DN, Fintelmann FJ, Little BP, Shepard J-AO, Flores EJ. Racial and ethnic disparities in lung cancer screening eligibility. Radiology. 2021;301(3):712-720.
- Lopez-Olivo MA, Maki KG, Choi NJ, et al. Patient adherence to screening for lung cancer in the US: A systematic review and meta-analysis. JAMA Netw Open. 2020;3(11):e2025102-e2025102.
- Aldrich MC, Mercaldo SF, Sandler KL, Blot WJ, Grogan EL, Blume JD. Evaluation of USPSTF lung cancer screening guidelines among African American adult smokers. JAMA Oncol. 2019;5(9):1318-1324.
- Kunitomo Y, Bade B, Gunderson CG, et al. Racial differences in adherence to lung cancer screening follow-up: A systematic review and meta-analysis. Chest. 2022;161(1):266-275.
- Tanner NT, Gebregziabher M, Halbert CH, Payne E, Egede LE, Silvestri GA. Racial differences in outcomes within the National Lung Screening Trial: Implications for widespread implementation. Am J Respir Crit Care Med. 2015;192(2):200-208.
- Pasquinelli MM, Tammemägi MC, Kovitz KL, et al. Risk prediction model versus United States Preventive Services Task Force lung cancer screening eligibility criteria: Reducing race disparities. J Thorac Oncol. 2020;15(11):1738-1747.
- Duda C, Mahon I, Chen MH, et al. Impact and costs of targeted recruitment of minorities to the National Lung Screening Trial. Clin Trials. 2011;8(2):214-223.
- Barta JA, Shusted CS, Ruane B, et al. Racial differences in lung cancer screening beliefs and screening adherence. Clin Lung Cancer. 2021;22(6):570-578.
- Annesi CA, Poulson MR, Mak KS, et al. The impact of residential racial segregation on non-small cell lung cancer treatment and outcomes. Ann Thorac Surg. 2022;113(4):1291-1298.
- Lin Y, Liang L-J, Ding R, Prosper AE, Aberle DR, Hsu W. Factors associated with nonadherence to lung cancer screening across multiple screening time points. JAMA Netw Open. 2023;6(5):e2315250-e2315250.
- Martinez MC, Stults CD, Li J. Provider and patient perspectives to improve lung cancer screening with low-dose computed tomography 5 years after Medicare coverage: A qualitative study. BMC Prim Care. 2022;23(1):332-332.
- Lee SJC, Lee J, Zhu H, et al. Assessing barriers and facilitators to lung cancer screening: Initial findings from a patient navigation intervention. Popul Health Manag. 2023;26(3):177-184.
- Lung cancer - Clinical preventive service recommendation. American Academy of Family Physicians. https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/lung-cancer.html. Published 2021. Accessed 1 Aug, 2023.
- Borondy Kitts AK. The patient perspective on lung cancer screening and health disparities. J Amer Coll Radiol. 2019;16(4):601-606.
Citation
Matsumoto MM, Erkmen CP, Dako F. Understanding Patient Barriers to Utilization of Low-dose CT Lung Cancer Screening in a High-risk Population. Supplement to Applied Radiology. 2024;(1):11-15.
January 25, 2024